Podcast
Questions and Answers
What is the primary function of the myocardium layer in the heart?
What is the primary function of the myocardium layer in the heart?
- To pump blood through contraction of cardiac muscle tissue (correct)
- To form a barrier between the heart and surrounding structures
- To facilitate friction-free movement of the heart
- To provide a protective outer layer for the heart
Which chamber of the heart is responsible for receiving deoxygenated blood from the head, neck, and arms?
Which chamber of the heart is responsible for receiving deoxygenated blood from the head, neck, and arms?
- Left ventricle
- Left atrium
- Right atrium (correct)
- Right ventricle
Where is the apex of the heart located?
Where is the apex of the heart located?
- Next to the left atrium
- Superior to the second rib
- In the center of the mediastinum
- Between the fifth and sixth ribs near the diaphragm (correct)
What is the function of the pericardium?
What is the function of the pericardium?
Which layer of the heart is the thinnest and composed of connective tissue?
Which layer of the heart is the thinnest and composed of connective tissue?
What characterizes the function of the right side of the heart?
What characterizes the function of the right side of the heart?
Which blood vessel returns deoxygenated blood from the lower parts of the body to the heart?
Which blood vessel returns deoxygenated blood from the lower parts of the body to the heart?
How many chambers does the heart have?
How many chambers does the heart have?
What is the primary function of the left ventricle?
What is the primary function of the left ventricle?
Which valve is situated between the left atrium and the left ventricle?
Which valve is situated between the left atrium and the left ventricle?
What characteristic allows the heart's conduction system to generate rhythmic contractions?
What characteristic allows the heart's conduction system to generate rhythmic contractions?
Which structure serves as the pacemaker of the heart?
Which structure serves as the pacemaker of the heart?
How does the sympathetic nervous system affect the cardiovascular system?
How does the sympathetic nervous system affect the cardiovascular system?
What is the average duration of a cardiac cycle?
What is the average duration of a cardiac cycle?
Which sound is produced when the AV valves close?
Which sound is produced when the AV valves close?
What type of blood vessels carry blood back to the heart?
What type of blood vessels carry blood back to the heart?
What condition can cause a heart murmur?
What condition can cause a heart murmur?
Which type of circulation delivers oxygenated blood to the body?
Which type of circulation delivers oxygenated blood to the body?
What is the primary role of Purkinje fibers in the heart?
What is the primary role of Purkinje fibers in the heart?
What is a common characteristic of an audible murmur with a valve stenosis?
What is a common characteristic of an audible murmur with a valve stenosis?
Which statement accurately describes the atrioventricular node?
Which statement accurately describes the atrioventricular node?
Which grading of murmur indicates it is audible without experience?
Which grading of murmur indicates it is audible without experience?
What is the primary purpose of performing an electrocardiogram (EKG)?
What is the primary purpose of performing an electrocardiogram (EKG)?
Which cardiac enzyme is considered the most cardiac specific and sensitive for detecting myocardial damage?
Which cardiac enzyme is considered the most cardiac specific and sensitive for detecting myocardial damage?
What type of monitor allows patients to move freely while being monitored for cardiac events?
What type of monitor allows patients to move freely while being monitored for cardiac events?
In thallium scanning, what does a 'cold spot' indicate?
In thallium scanning, what does a 'cold spot' indicate?
What does a B-type Natriuretic Peptide (BNP) level above 100 pg/ml suggest?
What does a B-type Natriuretic Peptide (BNP) level above 100 pg/ml suggest?
Which of the following is NOT a method of performing percutaneous coronary intervention (PCI)?
Which of the following is NOT a method of performing percutaneous coronary intervention (PCI)?
What is the maximum duration over which ambulatory or Holter monitors typically record heart rhythms?
What is the maximum duration over which ambulatory or Holter monitors typically record heart rhythms?
What is the primary indication for performing exercise-stress testing?
What is the primary indication for performing exercise-stress testing?
When assessing a patient on anticoagulant therapy, what does the INR measure?
When assessing a patient on anticoagulant therapy, what does the INR measure?
Which of the following is true regarding exercise-stress testing?
Which of the following is true regarding exercise-stress testing?
What is typically used to estimate the ejection fraction in echocardiography?
What is typically used to estimate the ejection fraction in echocardiography?
What limits the effectiveness of CK and CK-MB as markers for myocardial infarction?
What limits the effectiveness of CK and CK-MB as markers for myocardial infarction?
What is the main function of a coronary stent?
What is the main function of a coronary stent?
What is primarily responsible for the degree of stretch in a ventricle before the next contraction?
What is primarily responsible for the degree of stretch in a ventricle before the next contraction?
Which statement about diastole is correct?
Which statement about diastole is correct?
How is cardiac output (CO) calculated?
How is cardiac output (CO) calculated?
What condition may arise from excessive end-diastolic volume in the left ventricle?
What condition may arise from excessive end-diastolic volume in the left ventricle?
What does afterload primarily refer to?
What does afterload primarily refer to?
What is one use of cardiac catheterization?
What is one use of cardiac catheterization?
What role does contrast dye play in an angiogram?
What role does contrast dye play in an angiogram?
Which of the following can affect the afterload experienced by the ventricles?
Which of the following can affect the afterload experienced by the ventricles?
What happens to cardiac contractility when preload is optimized?
What happens to cardiac contractility when preload is optimized?
What is an important nursing action to take after an angiogram?
What is an important nursing action to take after an angiogram?
Which of the following occurs first during the cardiac cycle?
Which of the following occurs first during the cardiac cycle?
During which phase of the cardiac cycle does the majority of ventricular filling occur?
During which phase of the cardiac cycle does the majority of ventricular filling occur?
What is a common requirement for both angiogram and cardiac catheterization procedures?
What is a common requirement for both angiogram and cardiac catheterization procedures?
Which condition may be monitored for after cardiac catheterization to prevent complications?
Which condition may be monitored for after cardiac catheterization to prevent complications?
What is the main function of the heart's pericardium?
What is the main function of the heart's pericardium?
How does the structure of the heart enable it to function as two separate pumps?
How does the structure of the heart enable it to function as two separate pumps?
Describe the location of the heart within the chest cavity.
Describe the location of the heart within the chest cavity.
What role does the myocardium play in heart function?
What role does the myocardium play in heart function?
What are the two main components of the cardiac cycle influenced by the structure of heart chambers?
What are the two main components of the cardiac cycle influenced by the structure of heart chambers?
What two major blood vessels return deoxygenated blood to the right atrium?
What two major blood vessels return deoxygenated blood to the right atrium?
What is the significance of the heart's apex being slightly left of the midline?
What is the significance of the heart's apex being slightly left of the midline?
How does the structure of cardiac muscle contribute to the heart's function?
How does the structure of cardiac muscle contribute to the heart's function?
What signs might indicate a patient is experiencing bleeding, and what assessments should the nurse perform?
What signs might indicate a patient is experiencing bleeding, and what assessments should the nurse perform?
How does a Holter monitor assist in the assessment of patients with suspected cardiac disease?
How does a Holter monitor assist in the assessment of patients with suspected cardiac disease?
What is the primary purpose of performing a thallium scan?
What is the primary purpose of performing a thallium scan?
What does a BNP level above 100 pg/ml indicate regarding heart failure?
What does a BNP level above 100 pg/ml indicate regarding heart failure?
Why is Troponin I considered the gold standard cardiac enzyme for detecting myocardial damage?
Why is Troponin I considered the gold standard cardiac enzyme for detecting myocardial damage?
Describe the role of a telemetry monitor in cardiac patient care.
Describe the role of a telemetry monitor in cardiac patient care.
What is the significance of performing exercise-stress testing in cardiac assessments?
What is the significance of performing exercise-stress testing in cardiac assessments?
Explain how electrocardiography (EKG) assists in diagnosing cardiac issues.
Explain how electrocardiography (EKG) assists in diagnosing cardiac issues.
What are the primary interventions available for an acute STEMI?
What are the primary interventions available for an acute STEMI?
How are cardiac enzymes monitored in patients receiving anticoagulant therapy?
How are cardiac enzymes monitored in patients receiving anticoagulant therapy?
What is the function of a coronary stent in cardiac care?
What is the function of a coronary stent in cardiac care?
In what scenarios are ambulatory monitors most beneficial?
In what scenarios are ambulatory monitors most beneficial?
What is the purpose of echocardiography in cardiac assessments?
What is the purpose of echocardiography in cardiac assessments?
What complications can arise from a myocardial infarction as indicated by cardiac enzymes?
What complications can arise from a myocardial infarction as indicated by cardiac enzymes?
What are the two types of valves in the heart and their functions?
What are the two types of valves in the heart and their functions?
Describe the primary role of the left ventricle in the circulatory system.
Describe the primary role of the left ventricle in the circulatory system.
What are the implications of the delay caused by the atrioventricular node?
What are the implications of the delay caused by the atrioventricular node?
How do the sympathetic and parasympathetic nervous systems influence heart function?
How do the sympathetic and parasympathetic nervous systems influence heart function?
What is a heart murmur and how can it be assessed?
What is a heart murmur and how can it be assessed?
Explain the concept of automaticity in the heart's conduction system.
Explain the concept of automaticity in the heart's conduction system.
What is the role of the sino-atrial (SA) node in cardiac function?
What is the role of the sino-atrial (SA) node in cardiac function?
What are the main types of blood vessels involved in systemic circulation?
What are the main types of blood vessels involved in systemic circulation?
Discuss the significance of the cardiac cycle's phases, systole and diastole.
Discuss the significance of the cardiac cycle's phases, systole and diastole.
What is the function of Purkinje fibers in the heart?
What is the function of Purkinje fibers in the heart?
What cardiovascular changes occur in the body during exercise?
What cardiovascular changes occur in the body during exercise?
What is the primary component of coronary circulation?
What is the primary component of coronary circulation?
How is a heart murmur graded?
How is a heart murmur graded?
What happens during pulmonary circulation?
What happens during pulmonary circulation?
How does preload influence cardiac output?
How does preload influence cardiac output?
What is the definition of afterload in cardiac physiology?
What is the definition of afterload in cardiac physiology?
What occurs during ventricular diastole?
What occurs during ventricular diastole?
Why is contractility significant in the cardiac cycle?
Why is contractility significant in the cardiac cycle?
What risks are associated with excessive end-diastolic volume in the left ventricle?
What risks are associated with excessive end-diastolic volume in the left ventricle?
How does cardiac catheterization aid in diagnosing heart conditions?
How does cardiac catheterization aid in diagnosing heart conditions?
What precaution should be taken regarding allergies before an angiogram?
What precaution should be taken regarding allergies before an angiogram?
What is the role of an informed consent in invasive cardiac procedures?
What is the role of an informed consent in invasive cardiac procedures?
What indicates a need for monitoring vital signs after cardiac catheterization?
What indicates a need for monitoring vital signs after cardiac catheterization?
How does fluoroscopy contribute to cardiac procedures?
How does fluoroscopy contribute to cardiac procedures?
What complications can arise if proper post-procedure care is neglected after cardiac catheterization?
What complications can arise if proper post-procedure care is neglected after cardiac catheterization?
What can measuring right or left ventricular stroke work index help to assess?
What can measuring right or left ventricular stroke work index help to assess?
What is the significance of observing blood flow patterns in relation to afterload?
What is the significance of observing blood flow patterns in relation to afterload?
What is the purpose of using contrast dye in angiography?
What is the purpose of using contrast dye in angiography?
How does an increased systemic vascular resistance affect cardiac output?
How does an increased systemic vascular resistance affect cardiac output?
Flashcards are hidden until you start studying
Study Notes
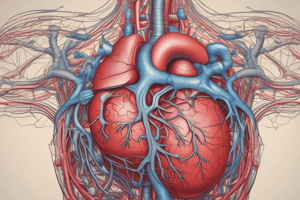
Heart Overview
- The heart, roughly the size of a fist, pumps 1,000 gallons of blood daily and beats about 100,000 times, circulating blood through 60,000 miles of vessels.
- Located in the mediastinum, the heart's base sits superior to the second rib, while the apex is positioned between the fifth and sixth ribs, slightly to the left.
Heart Wall Layers
- Pericardium: A two-layered membrane that encases the heart, with serous fluid separating the layers to facilitate movement.
- Myocardium: The thickest layer composed of cardiac muscle, responsible for blood pumping through contractions.
- Endocardium: The innermost layer, made of thin connective tissue.
Heart Functionality
- Acts as two pumps: the right side handles deoxygenated blood sent to the lungs, while the left pumps oxygenated blood to the body.
Heart Chambers
- Divided into four chambers: right atrium, right ventricle, left atrium, and left ventricle.
- Right Atrium: Receives deoxygenated blood via superior vena cava (head, neck, arms), inferior vena cava (lower body), and coronary sinus (heart muscle).
- Right Ventricle: Pumps deoxygenated blood to the lungs through the pulmonary artery.
- Left Atrium: Receives oxygenated blood from the lungs through pulmonary veins.
- Left Ventricle: The strongest chamber, pumps oxygenated blood throughout the body via the aorta.
Heart Valves
- Atrioventricular Valves:
- Tricuspid valve (3 cusps) between right atrium and ventricle.
- Mitral valve (2 cusps) between left atrium and ventricle.
- Semilunar Valves:
- Pulmonary valve (3 cusps) between right ventricle and pulmonary artery.
- Aortic valve (3 cusps) between left ventricle and aorta.
Conduction System
- Comprised of specialized tissue enabling rhythmic contractions termed automaticity.
- Key components include:
- SA Node: Heart's pacemaker, located in the right atrium, initiates atrial contraction.
- AV Node: Delays impulse transmission, allowing complete atrial contraction.
- Bundle of His: Divides into left and right branches, causing ventricular contraction.
Heart Sounds
- Characterized by "Lub-Dub" sounds:
- “Lub” (S1) occurs when AV valves close.
- “Dub” (S2) occurs when semilunar valves close.
- Murmurs may indicate abnormal valve function or conditions like septal defects.
Blood Vessel Types
- Arteries: Carry blood away from the heart; branch into arterioles, leading to capillaries.
- Veins: Collect blood from capillaries, forming larger venules that return blood to the heart.
Circulation Types
- Systemic Circulation: Blood pumped from the left ventricle through the aorta to the body; returns to the right atrium.
- Coronary Circulation: Right and left coronary arteries supply oxygen to the heart muscle.
- Pulmonary Circulation: Deoxygenated blood flows from the right ventricle to the lungs; oxygenated blood returns to the left atrium.
Cardiac Output Components
- Cardiac Output (CO): Affected by heart rate and stroke volume.
- Preload: Ventricular stretch before contraction related to blood volume.
- Afterload: Resistance ventricles must overcome to eject blood.
- Contractility: Strength of heart muscle contractions during systole.
Cardiac Monitoring Techniques
- Chest Radiography: Assesses heart size and shape.
- Fluoroscopy: Allows observation of heart movement in real-time.
- Angiogram: Visualizes blood vessels after contrast medium injection.
- Cardiac Catheterization: Visualizes heart structures and measures pressures.
- Electrocardiogram (EKG): Monitors cardiac impulses through electrodes.
Cardiac Enzymes and Biomarkers
- Troponin I: Sensitive and specific marker for myocardial damage.
- B-type Natriuretic Peptide (BNP): Indicates heart failure when levels exceed 100 pg/ml.
Interventional Procedures
- Percutaneous Coronary Intervention (PCI): Aims to restore blood flow in acute myocardial infarction; includes procedures like angioplasty and stenting.
- Coronary Stent: Keeps arteries open post-stenosis treatment.
Additional Monitoring
- Holter Monitor: Monitors heart rhythms over 12-48 hours for suspected conditions.
- Stress Testing: Assesses cardiac function under physical exertion.
- Thallium Scanning: Identifies myocardial ischemia via radioactive isotope tracing.
- Echocardiography: Uses ultrasound to evaluate heart structure and function.
After Procedure Care
- Monitor vital signs and assess insertion sites post-catheterization to prevent complications like hemorrhage.
Heart Overview
- The heart, roughly the size of a fist, pumps 1,000 gallons of blood daily and beats about 100,000 times, circulating blood through 60,000 miles of vessels.
- Located in the mediastinum, the heart's base sits superior to the second rib, while the apex is positioned between the fifth and sixth ribs, slightly to the left.
Heart Wall Layers
- Pericardium: A two-layered membrane that encases the heart, with serous fluid separating the layers to facilitate movement.
- Myocardium: The thickest layer composed of cardiac muscle, responsible for blood pumping through contractions.
- Endocardium: The innermost layer, made of thin connective tissue.
Heart Functionality
- Acts as two pumps: the right side handles deoxygenated blood sent to the lungs, while the left pumps oxygenated blood to the body.
Heart Chambers
- Divided into four chambers: right atrium, right ventricle, left atrium, and left ventricle.
- Right Atrium: Receives deoxygenated blood via superior vena cava (head, neck, arms), inferior vena cava (lower body), and coronary sinus (heart muscle).
- Right Ventricle: Pumps deoxygenated blood to the lungs through the pulmonary artery.
- Left Atrium: Receives oxygenated blood from the lungs through pulmonary veins.
- Left Ventricle: The strongest chamber, pumps oxygenated blood throughout the body via the aorta.
Heart Valves
- Atrioventricular Valves:
- Tricuspid valve (3 cusps) between right atrium and ventricle.
- Mitral valve (2 cusps) between left atrium and ventricle.
- Semilunar Valves:
- Pulmonary valve (3 cusps) between right ventricle and pulmonary artery.
- Aortic valve (3 cusps) between left ventricle and aorta.
Conduction System
- Comprised of specialized tissue enabling rhythmic contractions termed automaticity.
- Key components include:
- SA Node: Heart's pacemaker, located in the right atrium, initiates atrial contraction.
- AV Node: Delays impulse transmission, allowing complete atrial contraction.
- Bundle of His: Divides into left and right branches, causing ventricular contraction.
Heart Sounds
- Characterized by "Lub-Dub" sounds:
- “Lub” (S1) occurs when AV valves close.
- “Dub” (S2) occurs when semilunar valves close.
- Murmurs may indicate abnormal valve function or conditions like septal defects.
Blood Vessel Types
- Arteries: Carry blood away from the heart; branch into arterioles, leading to capillaries.
- Veins: Collect blood from capillaries, forming larger venules that return blood to the heart.
Circulation Types
- Systemic Circulation: Blood pumped from the left ventricle through the aorta to the body; returns to the right atrium.
- Coronary Circulation: Right and left coronary arteries supply oxygen to the heart muscle.
- Pulmonary Circulation: Deoxygenated blood flows from the right ventricle to the lungs; oxygenated blood returns to the left atrium.
Cardiac Output Components
- Cardiac Output (CO): Affected by heart rate and stroke volume.
- Preload: Ventricular stretch before contraction related to blood volume.
- Afterload: Resistance ventricles must overcome to eject blood.
- Contractility: Strength of heart muscle contractions during systole.
Cardiac Monitoring Techniques
- Chest Radiography: Assesses heart size and shape.
- Fluoroscopy: Allows observation of heart movement in real-time.
- Angiogram: Visualizes blood vessels after contrast medium injection.
- Cardiac Catheterization: Visualizes heart structures and measures pressures.
- Electrocardiogram (EKG): Monitors cardiac impulses through electrodes.
Cardiac Enzymes and Biomarkers
- Troponin I: Sensitive and specific marker for myocardial damage.
- B-type Natriuretic Peptide (BNP): Indicates heart failure when levels exceed 100 pg/ml.
Interventional Procedures
- Percutaneous Coronary Intervention (PCI): Aims to restore blood flow in acute myocardial infarction; includes procedures like angioplasty and stenting.
- Coronary Stent: Keeps arteries open post-stenosis treatment.
Additional Monitoring
- Holter Monitor: Monitors heart rhythms over 12-48 hours for suspected conditions.
- Stress Testing: Assesses cardiac function under physical exertion.
- Thallium Scanning: Identifies myocardial ischemia via radioactive isotope tracing.
- Echocardiography: Uses ultrasound to evaluate heart structure and function.
After Procedure Care
- Monitor vital signs and assess insertion sites post-catheterization to prevent complications like hemorrhage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.