Podcast
Questions and Answers
Steroid hormones are derived from what?
Steroid hormones are derived from what?
- Amino acids
- Peptides
- Proteins
- Cholesterol (correct)
Which of the following is characteristic of non-steroid hormones?
Which of the following is characteristic of non-steroid hormones?
- Hydrophobic nature
- Ability to pass through phospholipid bilayer
- Binding to surface receptor proteins (correct)
- Production in adrenal glands
Amino acid hormones are derived from which amino acid?
Amino acid hormones are derived from which amino acid?
- Phenylalanine
- Serine
- Tryptophan
- Tyrosine (correct)
What is a common result of both peptide and steroid hormone action?
What is a common result of both peptide and steroid hormone action?
What is the name of the structure that suspends the pituitary gland?
What is the name of the structure that suspends the pituitary gland?
Which gland is known as the 'master gland' of the endocrine system?
Which gland is known as the 'master gland' of the endocrine system?
What are the two main lobes of the pituitary gland?
What are the two main lobes of the pituitary gland?
What is the embryological origin of the anterior pituitary?
What is the embryological origin of the anterior pituitary?
Which of the following is the largest component of the anterior pituitary?
Which of the following is the largest component of the anterior pituitary?
Which type of cell in the anterior pituitary stains dark red?
Which type of cell in the anterior pituitary stains dark red?
What hormone do somatotrophs secrete?
What hormone do somatotrophs secrete?
Which of the following carries oxytocin and ADH?
Which of the following carries oxytocin and ADH?
What connects the two lobes of the thyroid gland?
What connects the two lobes of the thyroid gland?
How many parathyroid glands are there?
How many parathyroid glands are there?
Which artery supplies the inferior and posterior aspects of the thyroid gland?
Which artery supplies the inferior and posterior aspects of the thyroid gland?
Which vein does the superior thyroid vein drain into?
Which vein does the superior thyroid vein drain into?
Which structure supplies the parathyroid glands?
Which structure supplies the parathyroid glands?
Which of the following directly innervates the thyroid gland through the parasympathetic nervous system?
Which of the following directly innervates the thyroid gland through the parasympathetic nervous system?
What hormone do parafollicular cells (C cells) secrete?
What hormone do parafollicular cells (C cells) secrete?
Which cells secrete PTH?
Which cells secrete PTH?
The exocrine gland of the pancreas secretes what?
The exocrine gland of the pancreas secretes what?
What hormones does the endocrine gland of the pancreas secrete?
What hormones does the endocrine gland of the pancreas secrete?
Which nerve provides parasympathetic innervation to the pancreas?
Which nerve provides parasympathetic innervation to the pancreas?
Which cells in the islets of Langerhans secrete insulin?
Which cells in the islets of Langerhans secrete insulin?
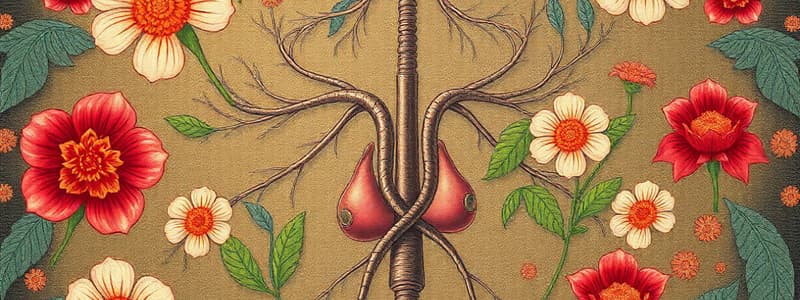
What type of hormones are secreted by the adrenal gland?
What type of hormones are secreted by the adrenal gland?
Where are catecholamines produced in the adrenal gland?
Where are catecholamines produced in the adrenal gland?
What type of hormone is secreted in the zona glomerulosa?
What type of hormone is secreted in the zona glomerulosa?
Somatomedins stimulate what process?
Somatomedins stimulate what process?
Which hormone does the hypothalamus secrete to stimulate growth hormone release?
Which hormone does the hypothalamus secrete to stimulate growth hormone release?
What is the primary effect of ADH?
What is the primary effect of ADH?
Where is ADH released?
Where is ADH released?
What triggers the release of insulin?
What triggers the release of insulin?
What inhibits insulin secretion?
What inhibits insulin secretion?
Where is glucagon produced?
Where is glucagon produced?
Which hormone promotes the breakdown of glycogen stores in the liver?
Which hormone promotes the breakdown of glycogen stores in the liver?
What is the main function of cortisol?
What is the main function of cortisol?
Where are cortisol receptors found?
Where are cortisol receptors found?
Where are thyroid hormones produced?
Where are thyroid hormones produced?
What does TSH bind to?
What does TSH bind to?
Where does parathryoid hormone come from?
Where does parathryoid hormone come from?
Normal/high calcium cause what?
Normal/high calcium cause what?
What is the precursor molecule for steroid hormones?
What is the precursor molecule for steroid hormones?
Which amino acid is the precursor for the synthesis of thyroid hormones, epinephrine, and norepinephrine?
Which amino acid is the precursor for the synthesis of thyroid hormones, epinephrine, and norepinephrine?
What is the anterior pituitary also known as?
What is the anterior pituitary also known as?
From what embryonic tissue does the anterior pituitary originate?
From what embryonic tissue does the anterior pituitary originate?
Which of the following is the largest part of the anterior pituitary?
Which of the following is the largest part of the anterior pituitary?
Which type of chromophil cell stains dark red?
Which type of chromophil cell stains dark red?
Which of the following structures carries ADH and oxytocin?
Which of the following structures carries ADH and oxytocin?
What structure connects the two lobes of the thyroid gland?
What structure connects the two lobes of the thyroid gland?
How many parathyroid glands are typically found in humans?
How many parathyroid glands are typically found in humans?
What artery supplies the inferior aspect of the thyroid gland?
What artery supplies the inferior aspect of the thyroid gland?
Into which vein does the superior thyroid vein drain?
Into which vein does the superior thyroid vein drain?
Which blood vessels supply the parathyroid glands?
Which blood vessels supply the parathyroid glands?
Which hormone is secreted by parafollicular cells (C cells) in the thyroid gland?
Which hormone is secreted by parafollicular cells (C cells) in the thyroid gland?
Which cells secrete parathyroid hormone (PTH)?
Which cells secrete parathyroid hormone (PTH)?
Which of the following is secreted by the endocrine gland of the pancreas?
Which of the following is secreted by the endocrine gland of the pancreas?
In what part of the adrenal gland are catecholamines produced?
In what part of the adrenal gland are catecholamines produced?
What process do somatomedins stimulate?
What process do somatomedins stimulate?
Which hormone decreases bone formation and decreases production of type 1 collagen?
Which hormone decreases bone formation and decreases production of type 1 collagen?
Parathyroid hormone comes from which source?
Parathyroid hormone comes from which source?
Calcium levels when high or normal cause what?
Calcium levels when high or normal cause what?
Flashcards
Steroid Hormones
Steroid Hormones
Hydrophobic, found in adrenal glands and gonads, and derived from cholesterol.
Non-steroid Hormones
Non-steroid Hormones
Hydrophilic, unable to pass through the phospholipid bilayer. They bind to surface receptor proteins.
Pituitary Gland
Pituitary Gland
A small, oval-shaped gland located on the underside of the cerebrum, suspended by the infundibulum, and lodged within the hypophyseal fossa.
Adenohypophysis
Adenohypophysis
Signup and view all the flashcards
Neurohypophysis
Neurohypophysis
Signup and view all the flashcards
Chromophils
Chromophils
Signup and view all the flashcards
Acidophils (Somatotrophs)
Acidophils (Somatotrophs)
Signup and view all the flashcards
Chromophobes
Chromophobes
Signup and view all the flashcards
Thyroid Gland Arterial Supply
Thyroid Gland Arterial Supply
Signup and view all the flashcards
Thyroid Gland Venous Drainage
Thyroid Gland Venous Drainage
Signup and view all the flashcards
Thyroid Gland Cells
Thyroid Gland Cells
Signup and view all the flashcards
Pancreas
Pancreas
Signup and view all the flashcards
Pancreatic Islet Cells
Pancreatic Islet Cells
Signup and view all the flashcards
Adrenal Gland Secretions
Adrenal Gland Secretions
Signup and view all the flashcards
Adrenal Cortex
Adrenal Cortex
Signup and view all the flashcards
Adrenal Medulla
Adrenal Medulla
Signup and view all the flashcards
Somatomedins
Somatomedins
Signup and view all the flashcards
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Signup and view all the flashcards
Insulin
Insulin
Signup and view all the flashcards
Glucagon
Glucagon
Signup and view all the flashcards
Cortisol Production Control
Cortisol Production Control
Signup and view all the flashcards
Thyroid Hormone Effects
Thyroid Hormone Effects
Signup and view all the flashcards
Parathyroid Hormone (PTH)
Parathyroid Hormone (PTH)
Signup and view all the flashcards
Innate Immune Response
Innate Immune Response
Signup and view all the flashcards
Adaptive Immune Response
Adaptive Immune Response
Signup and view all the flashcards
Dendritic Cells
Dendritic Cells
Signup and view all the flashcards
Lymphocytes
Lymphocytes
Signup and view all the flashcards
Natural Killer Cells
Natural Killer Cells
Signup and view all the flashcards
B Cells
B Cells
Signup and view all the flashcards
T Cells
T Cells
Signup and view all the flashcards
MHC Class I Molecules
MHC Class I Molecules
Signup and view all the flashcards
MHC Class II Molecules
MHC Class II Molecules
Signup and view all the flashcards
T cell Activation
T cell Activation
Signup and view all the flashcards
Th1 cells
Th1 cells
Signup and view all the flashcards
Th2 Cells
Th2 Cells
Signup and view all the flashcards
Th17 receptor
Th17 receptor
Signup and view all the flashcards
Natural killer cell
Natural killer cell
Signup and view all the flashcards
Antibody dependent cell meditated cytotoxicity (ADCC)
Antibody dependent cell meditated cytotoxicity (ADCC)
Signup and view all the flashcards
B cell receptor
B cell receptor
Signup and view all the flashcards
Lymph-node entry
Lymph-node entry
Signup and view all the flashcards
path activation
path activation
Signup and view all the flashcards
IgM/IgD
IgM/IgD
Signup and view all the flashcards
IgG antibody
IgG antibody
Signup and view all the flashcards
Lectin binding pathway
Lectin binding pathway
Signup and view all the flashcards
Study Notes
- Steroid hormones are hydrophobic and nonpolar, synthesized from cholesterol in adrenal glands and gonads.
- Non-steroid hormones are peptides or proteins, hydrophilic, unable to pass through the phospholipid bilayer, and bind to surface receptor proteins.
- Amino acid hormones derive from tyrosine, including thyroid hormone, epinephrine, and norepinephrine.
- Both peptide and steroid hormones can cause changes in gene expression.
Pituitary Gland
- The pituitary gland is a small, oval-shaped gland located on the underside of the cerebrum, suspended by the infundibulum, and lodged within the hypophyseal fossa.
- Serves as the endocrine interface between the central nervous system and the body.
- Composed of two lobes: the anterior (adenohypophysis) and posterior (neurohypophysis).
- The anterior pituitary originates from the adenohypophyseal pouch (Rathe’s pouch), an out-pouching of the oral cavity roof, derived from oral ectoderm.
- Anterior pituitary has three parts: pars distalis (largest, secretory), pars tuberalis (infundibular stalk extension), and pars intermedia (thin, avascular layer).
- Anterior pituitary contains chromophils (dark staining) and chromophobes (light staining).
- Chromophils include acidophils (dark red, somatotrophs for growth hormone, lactotrophs for prolactin) and basophils (purple-blue, corticotrophs, gonadotrophs, thyrotrophs).
- The posterior pituitary contains unmyelinated axons carrying oxytocin and ADH, along with supporting glial cells, and Herring bodies.
Thyroid and Parathyroid Glands
- The thyroid gland has two lobes connected by an isthmus, located along the anterior and lateral aspects of the trachea and inferior larynx.
- Four parathyroid glands are on the posterior side of each thyroid lobe.
- The superior thyroid artery (branches: anterior, posterior, lateral) and inferior thyroid artery (branches: ascending/superior and inferior) supply the thyroid gland.
- Superior, middle, and inferior thyroid veins drain the thyroid venous plexus.
- Superior thyroid veins drain into the internal jugular vein.
- Middle thyroid veins drain into the internal jugular vein.
- Inferior thyroid veins drain into the brachiocephalic vein or superior vena cava.
- Inferior thyroid arteries arise from the thyrocervical trunk, supplying the parathyroid glands.
- The thyroid venous plexus follows the path of thyroid veins.
- Sympathetic and parasympathetic nervous systems act on thyroid gland blood vessels to constrict or dilate.
- Parasympathetic innervation via vagus nerve (CN X), external branch of superior laryngeal nerve, and recurrent laryngeal nerve.
- Parathyroid glands receive only sympathetic innervation from superior and middle cervical ganglia.
- The thyroid gland contains follicles (with colloid and epithelial cells secreting thyroid hormones) and parafollicular cells (C cells secreting calcitonin).
- The parathyroid gland has a fibrous capsule, connective tissue, up to 40% adipose tissue, and chief and oxyphil cells.
- Chief cells secrete PTH (smaller, pale cytoplasm).
- Oxyphil cells do not secrete PTH and increase with age (larger, dark nuclei, more mitochondria).
Pancreas
- The pancreas is a retroperitoneal organ with exocrine and endocrine functions.
- Exocrine gland secretes pancreatic juices into the duodenum.
- Endocrine gland secretes insulin and glucagon into the bloodstream.
- Pancreas is divided into the head, uncinate process, neck, body, and tail.
- Arterial supply includes pancreatic branches of the splenic artery and anterior/posterior pancreaticoduodenal arteries.
- Venous drainage is from pancreatic veins.
- Sympathetic innervation is via greater and lesser splanchnic nerves.
- Parasympathetic innervation is via the vagus nerve.
- Small endocrine cells are located in the islets of Langerhans.
- Four main islet cell types: beta cells (insulin), alpha cells (glucagon), delta cells (somatostatin), and PP cells (pancreatic polypeptide).
Adrenal Glands
- Paired endocrine glands sit on each kidney's superior pole and secrete steroid hormones and catecholamines.
- Secrete steroid hormones in response to stress, fluid balance, and ion homeostasis.
- Also secretes catecholamine hormones like epinephrine and norepinephrine (secreted during sympathetic responses).
- The right suprarenal gland is pyramid-shaped, posterior to the inferior vena cava and right liver lobe.
- The left suprarenal gland is semilunar, anterior to the right crus of the diaphragm, posterior to the stomach, pancreas, and spleen.
- Outer cortex produces steroid hormones, and inner medulla produces catecholamines.
- Arterial supply includes superior, middle, and inferior suprarenal arteries.
- The right suprarenal vein drains into the vena cava, and the left suprarenal vein drains into the left renal vein.
- Adrenal cortex zones: zona glomerulosa (mineralocorticoids), zona fasciculata (glucocorticoids, largest), and zona reticularis (gonadocorticoids/sex hormones).
- Adrenal medulla contains chromaffin cells arranged in clusters with capillaries.
Hormonal Control and Regulation
- Somatomedins stimulate cell growth and division.
- Hypothalamus secretes GHRH into the hypophyseal portal system, stimulating somatotrophs to release growth hormone.
- Increased somatotropin stimulates the hypothalamus to release GHRH; hypoglycemia, epinephrine, and estrogen and testosterone also stimulate release.
- Somatomedin hormones from the liver and bone signal the anterior pituitary to stop growth hormone production; growth hormone and somatomedins signal the hypothalamus.
- Growth hormone stimulates cellular metabolism, triggering lipolysis in adipose tissues, gluconeogenesis and glycogenolysis in the liver, increases insulin resistance in tissues, stimulating tissue growth, and stimulating release of IGF-1, which promotes muscle and bone growth (indirect effect).
- ADH inhibits urine production (antidiuretic hormone).
- Synthesized in paraventricular and supraoptic nuclei in the hypothalamus, released into the posterior pituitary and bloodstream.
- Elevated blood osmolarity detected by supraoptic nuclei and low blood pressure detected by baroreceptors trigger ADH release.
- ADH targets kidney cells (distal convoluted tubule, collecting duct cells) via AVPR2 receptors to increase water reabsorption, decreasing blood osmolarity and arterial smooth muscle cells.
- Insulin, produced by pancreatic beta cells, is triggered by increased glucose levels, the hormones glucagon and cortisol (indirect), and acetylcholine (parasympathetic nervous system).
- Insulin secretion is inhibited by norepinephrine (sympathetic nervous system) and somatostatin.
- Insulin is anabolic, promoting glucose-glycogen, fatty acids-fat, and amino acids-protein conversion, and targets the liver, adipose tissue, and skeletal muscle.
- Glucagon, from alpha cells in the islets of Langerhans, raises blood glucose during fasting.
- Glucagon triggers include low blood glucose and adrenaline and is inhibited by high blood glucose, somatostatin, and growth hormone.
- Glucagon promotes the breakdown of glycogen, fat, energy molecules glucose, and fatty acids, targeting the liver and adipose tissue.
- Cortisol production is controlled by the hypothalamus-pituitary axis.
- Hypothalamus secretes CRH, stimulating corticotrophs in the anterior pituitary to release ACTH, which travels to the adrenal cortex to stimulate cortisol production in cells of the zona fasciculata.
- Cortisol receptors are found throughout the body and act on adipose tissue (lipolysis), liver (gluconeogenesis, increased glycogen storage), muscles (proteolysis), general tissues (insulin resistance), blood vessels (vasoconstriction, increased blood pressure), and bone (decreases bone formation, and decreases production of type 1 collagen).
- Cortisol negatively feeds back the hypothalamus, reducing CRH and ACTH secretion.
- Thyroid hormones include T3 (triiodothyronine) and T4 (thyroxine).
- Follicular cells in the thyroid gland produce thyroid hormones.
- Low thyroid hormone levels stimulate TRH secretion by the hypothalamus, stimulating thyrotrophs in the anterior pituitary to release TSH, which then stimulates T3 and T4 release from the thyroid gland.
- Negative feedback from high thyroid hormone levels lowers secretion.
- Thyroid hormones bound to plasma proteins.
- Free T3 and T4 are active.
- Thyroid hormones increase Na-K ATPase activity, oxygen consumption, and metabolic rate.
- Catabolic effects include increased proteolysis, lipolysis, and gluconeogenesis.
- Cardiovascular effects include increased heart contractility and heart rate.
- Increased growth and development.
- Parathyroid hormone (PTH) comes from the parathyroid glands' chief cells.
- PTH release in inhibited by normal/high calcium and stimulated by low calcium levels.
- PTH increases extracellular calcium by, releasing calcium and phosphate from bones, decreasing serum phosphate, and increasing serum calcium through tubular and principal kidney cells.
Immune System
- The innate immune response consists of barriers (chemical and physical), macrophages, and natural killer cells. It is fast, has no memory, and is non-specific.
- Macrophages recognize pathogens by PAMPs (bacterial/fungal wall components, flagella proteins, viral RNA/DNA).
- Macrophages engulf pathogens in phagosomes, which fuse with lysosomes to form phagolysosomes, destroying their contents, also utilizes oxidative burst.
- White blood cells, including myeloid cells and phagocytic cells (neutrophils, macrophages, dendritic cells), release cytokines.
- The adaptive immune response is specific for viruses and bacteria (antigens), relies on cell activation, has memory, and involves T and B cells.
- Neutrophils ingest and destroy pathogens via phagocytosis and oxidative burst.
- Dendritic cells ingest pathogens, present antigens to T cells, and migrate to lymph nodes.
- Lymphocytes include B cells, T cells, and natural killer cells.
- B and T cells are adaptive immune cells, while natural killer cells are innate immune cells.
- B cells mature in the bone marrow, while T cells mature in the thymus.
- Natural killer cells target cells infected with viruses or cancer cells, killing them via cytotoxic granules and APOPTOSIS.
- B cells differentiate into plasma cells and produce antibodies.
- B cells find corresponding antigens and present them to T cells, which then triggers the B cell to transform into a plasma cell.
- Plasma cells secrete antibodies specific to the antigen, providing humoral immunity.
- There are two types of T cells: helper T cells (coordinate immune responses) and cytotoxic T cells (kill infected cells).
- T cells require antigen-presenting cells to have matured.
- Helper T cells (CD4) present to MHC II molecules, secreting cytokines.
- Cytotoxic T cells (CD8) recognize antigens on MHC I molecules and kill target cells.
- Once activated, T cells clone themselves.
Immune System Molecules
- MHC (major histocompatibility complex) molecules (also known as human leukocyte antigens - HLA) ensure T cells recognize and react to antigens.
- MHC I molecules are found on ALL nucleated cells, while MHC II molecules are found ONLY on antigen-presenting cells (macrophages, dendritic cells, B cells).
- MHC I molecules have alpha and beta 2 micro-globulin chains, an alpha chain with one alpha domain along with peptide-binding grooves, and present ONLY to cytotoxic T cells and Natural Killer Cells.
- MHC II molecules have alpha and beta chains and bind larger peptides to helper T cells only.
- Helper T cells express CD4, are responding to MHC Class II molecules, present on antigen presenting cells ONLY.
- Cytotoxic T cells express CD8, are responding to MHC Class I molecules, Present on ALL NUCLEATED cells in the body.
- T cells start out as naïve then get activated, resulting in differentiation Effector cell can be either, cytokines present around the cell determine the type of T cell it will be
- The CD3 complex is on the T cell membrane and binds the antigen and MHC molecule.
- CD4 and CD8 molecules secure the interaction between T cell receptors and MHC molecules.
- Activation of T cells requires T cell receptors to bind to the antigen
- Activation of T cells requires antigen (signal goes down the CD3 complex and CD4 or CD8 molecule) Co-Stimulation (Ligand CDc28 on T cell binds with B7 molecule on the antigen presenting cell).
- CD28 (for co-stimulation), binds to B7 structure on antigen presenting cell, second step to activate T cell.
- Immune synapse, T cell receptor is bounded to antigen+ CD4 or CD8 bound to MHC+B7 is bound to CD28.
- After T cells are activated, they will clone themselves.
- IL-2 Production- active T cell binds to IL-2 that they make which activates T helper cell start to rapidly undergo cell division called clonal expansion.
T Helper Cells
- T helper cells, including Th1, Th2, Th17, Tfh, and Tregs, originate from antigen-presenting cells.
- Th1 cells increase macrophages' ability to kill organisms and proliferate NK cells, cytotoxic T cells, and B cells.
- Th1 secretes interferon-gamma, boosting macrophages' ability to kill ingested pathogens via the oxidative burst.
- Th2 cells fight parasitic infections, producing cytokines that stimulate B cells to make IgE, stimulate mast cells, and basophils to bind to the Fc region of IgE that coats parasitic worms, which triggers cells to degranulate, and kills parasite.
- Th17 produces IL-17 to recruit neutrophils and fight bacterial and fungal infections.
- T follicular helper cells can help establish memory cells and plasma cells that make IgG, makes them express cytokine receptors, which allows them to produce IL-21 and interferon gamma stimulating B cells to differentiate into memory and plasma cells.
- Cytotoxic CD8 T cells bind nonspecifically to MHC I molecules, releasing perforin and granzymes to trigger apoptosis in target cells.
- Natural killer cells deliver granzymes and perforin non-specifically, recognize cell surface molecules of cells infected with viruses, intracellular bacteria, or cancerous cells.
- Antibody-dependent cell-mediated cytotoxicity (ADCC) involves natural killer cells using CD16 to bind to the Fc portion of IgG antibodies bound to viral proteins on infected cells.
- The B cell receptor, is basically an antibody, has a fragment antigen-binding region or (fab region, two fab fragments) that binds to the antigen, and a Constant region/fragment region, when it matures into a plasma cell, where then the receptor gets secreted as an antibody (exact same antigen).
- There are heavy chains, which all receptors early on are IgM.
- The cell will express igD in addition to IgM and, it is a Mature B cell.
- A mature b cell can travel to the lymphatic system.
Lymphatic Systems
- Lymph nodes are scattered throughout the body, and can be entered by travelling from lymphatics through the afferent lymphatic vessel, and from blood through the high endothelial venues (HEVs).
- T cells remain in Paracortical region
- Cortical region B cells migrate to the cortical region of the lymph node, forming the primary lymphoid follicles.
- If a B cell is activated, it replicates in the follicle and forms the germinal center, and, follicle will be known as the secondary lymphoid follicle.
- Antigens enter through the afferent lymphatic vessel and travel to the follicle and they (interact with B Cells in the follicle)
- For B cells to be activated, they must interact with a pathogen or complement fragment
- Do not require antigen presenting cells to present the antigen.
- Antigen crosslinks two B cell receptors.
- When the B cell is activated, it will differentiate into plasma cells and secrete antibodies. that react with pathogen or complement fragment
- For to make antibodies other than IgM b cells must interact with helper t cell (aka, isotope switching requires change in DNA, and once switched it cannot go back to IgM again)
- The B cell is linked to helper T cells when: T cell expresses molecule CD40L and binds it to CD40, this makes B cell express cytokine receptors, and makes t cell secrete cytokines.
Antibodies
- IgM b cell receptor, secreted as antibody, forms pentamer structure, help activation of the complement pathway.
- IgG is most abundant, binds two antigens serving as opsonin, part of opsonization process, activates the complement pathway, and works with NK cells to preform antibody dependent cell mediated Cycytotoxity
- Only antibody that can cross the placenta, protecting babies for 6 months
- IgA 20%, primary antibody in mucosal sites (such as the mouth, gut, and lungs)
- IgA Functions-opsonin, Binds and neutralizes pathogens where they enter the body.
- Babies receive lots of IgA in breast milk
- IgE.004% mount allergic responses, mount anti parasitic responses monomer
- IgD less than one precent, found alongside IgM and mature B lymphocytes monomer
- C1q subunits bind to the Fc portion of an antibody when it is bound to antigen, C1r cleaves C1s, and C1 is then activated in the classical pathway.
- Activated C1 cleaves C4 into C4a, and C4 binds to the surface pathogen, creating C3 convertase.
- C9 protein forms the membrane attack complex, creating holes in the cell membrane.
- Lymphatic vessels drain into lymph nodes, then the lymphatic trunks, then two main ducts, right lymphatic and thoractic duct.
- Contents of lymph drain into the superior vena cava to get to right atrium
- Lymph drain from White pulp where antibody coated bacteria are filtered out Red pulp is where old and defective blood cells are destroyed and are broken down and recycled"
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.