Podcast
Questions and Answers
What is the primary function of GnRH released by the hypothalamus?
What is the primary function of GnRH released by the hypothalamus?
- Acts on Sertoli cells to stimulate RNA synthesis
- Inhibits the secretion of LH and FSH
- Stimulates the production of testosterone from cholesterol
- Regulates the expression of LH and FSH (correct)
What is the effect of testosterone on Sertoli cells?
What is the effect of testosterone on Sertoli cells?
- Stimulates RNA synthesis and protein production
- Regulates the hypothalamic-pituitary axis
- Inhibits the production of inhibin
- Binds to intracellular receptors and stimulates ABP secretion (correct)
What is the primary function of LH in the reproductive system?
What is the primary function of LH in the reproductive system?
- Stimulates the production of FSH
- Acts on Sertoli cells to stimulate RNA synthesis
- Regulates the secretion of GnRH
- Acts on Leydig cells to stimulate testosterone production (correct)
What is the effect of inhibin on FSH secretion?
What is the effect of inhibin on FSH secretion?
What is the primary function of FSH in the reproductive system?
What is the primary function of FSH in the reproductive system?
What is the effect of testosterone on the hypothalamic-pituitary axis?
What is the effect of testosterone on the hypothalamic-pituitary axis?
What is the primary function of ABP in the reproductive system?
What is the primary function of ABP in the reproductive system?
What is the primary function of the hypothalamo-hypophysial axis?
What is the primary function of the hypothalamo-hypophysial axis?
What is the effect of FSH on RNA synthesis in Sertoli cells?
What is the effect of FSH on RNA synthesis in Sertoli cells?
What is the primary function of Leydig cells in the reproductive system?
What is the primary function of Leydig cells in the reproductive system?
Flashcards are hidden until you start studying
Study Notes
Hormone Regulation
- Serotonin controls sleep, pain control, sexual behavior, and hormone secretion in seasonally breeding mammals.
Hormone Activity
- Lipid-soluble hormones (thyroid and steroid hormones) have intracellular receptors, alter gene expression, and turn specific genes on or off.
- Water-soluble hormones (eicosanoids, polypeptide, and amine) have receptors as integral transmembrane proteins on the plasma membrane, using signal transduction.
Signal Transduction
- Steps:
- Hormone (first messenger) activates membrane G-protein.
- Adenylyl cyclase is activated, turning ATP into cAMP (second messenger).
- cAMP activates a protein kinase.
- The kinase phosphorylates a protein, activating or inactivating it.
- Phosphodiesterase inactivates cAMP if no more hormones bind to their extracellular receptors.
Gonadogenesis
Stage of Indifferent Gonads
- Gonads develop from mesenchyma, coelomic epithelium, and Primordial Germ Cells.
- Genital Ridge formation: genital ridges are formed at the 5th week of development by the proliferation of mesenchyme covered by coelomic epithelium.
Germ Cell Migration to Genital Ridges
- Primordial Germ Cells (PGCs) gather at the allantois, then pass into the yolk duct, the intestine, the dorsal mesentery, and finally reach the genital ridges.
Sex Cords Formation
- Sex cords (vascularized) are formed by a second group of cells deriving from the coelomic epithelium, which moves and surrounds the PGCs.
Chromosomal-Genetic Sexual Dimorphism
- X and Y chromosomes, with Y chromosome dominance.
Reproductive Messengers
Mode of Secretion
- Secretory process depends on the nature of secretion, blood supply of the secreting tissue, and solubility of the hormone (water-soluble or lipid-soluble).
- Endocrine: mediators are secreted into the interstitial fluid, then diffuse into blood capillaries, and circulate until they reach the target cells.
Classification of Hormones
Lipids
- Steroids and Eicosanoids, often carried on transporters.
- Steroids:
- Derived from cholesterol, which is synthesized from acetate.
- Cholesterol is converted to pregnenolone in the inner mitochondrial membrane.
- Pregnenolone is converted to sex steroids in the smooth ER.
- Four main families of steroids: progestagens, androgens, oestrogens, and corticosteroids.
- Biosynthetic unit enzymes interconvert them.
- Eicosanoids:
- Water-soluble, needing transporters to cross the plasma membrane.
- Comprise Prostaglandins and Leukotrines, with PGs having a greater role in reproductive processes.
- Arachidonic acid is a main precursor for PGs.
Functions of Testosterone
- Activation of hypophyseal testicular axis
- Differentiation of male genital organs
- Masculinization of urogenital sinus and external genitalia
- Acquisition of secondary sex characteristics and male behavior
- Maintenance and integrity of germ line (along with FSH)
- Initiation and maintenance of spermatogenesis
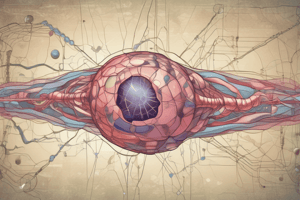
Control of Testicular Functions
Neuro-Endocrine Control
- The hypothalamo-hypophyseal axis regulates the reproductive system.
- GnRH released by the hypothalamus forms a blood vascularization with capillaries of the portal system, allowing rapid hormone transfer.
- GnRH controls the expression of LH and FSH, which have a pulsatile mode of release.
Functions of LH and FSH
- LH: acts on Leydig cells, stimulating production of testosterone from cholesterol.
- Testosterone: binds to intracellular receptors on Sertoli cells, stimulating them to secrete ABP.
- FSH: binds to extracellular receptors on Sertoli cells, stimulating RNA synthesis, testicular fluid production, and protein synthesis (including inhibin and ABP).
Negative Feedback Regulation
- Testosterone has a negative feedback on GnRH, inhibiting the secretion of LH and FSH.
- Inhibin: produced by Sertoli cells, inhibits the secretion of FSH by negative feedback.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.