Podcast
Questions and Answers
What is the main purpose of decalcification?
What is the main purpose of decalcification?
- To fix the tissue before embedding in paraffin.
- To enhance the staining process for better visibility of the cells.
- To remove calcium ions from bone or calcified tissue, making it easier to cut sections. (correct)
- To preserve the tissue for further processing.
Which of these is NOT a type of decalcifying agent?
Which of these is NOT a type of decalcifying agent?
- Heavy metals (correct)
- Weak organic acids
- Chelating agents
- Strong mineral acids
Which of the following is a strong mineral acid used for decalcification?
Which of the following is a strong mineral acid used for decalcification?
- Trichloroacetic Acid
- Formic Acid
- Chromic Acid
- Nitric Acid (correct)
Why are acid decalcifying agents commonly used?
Why are acid decalcifying agents commonly used?
What is the principle behind the use of strong mineral acids in decalcification?
What is the principle behind the use of strong mineral acids in decalcification?
What is the main advantage of using weak organic acids for decalcification?
What is the main advantage of using weak organic acids for decalcification?
When should decalcification be performed during tissue processing?
When should decalcification be performed during tissue processing?
Which of these factors can affect the efficiency of decalcification?
Which of these factors can affect the efficiency of decalcification?
What is the primary advantage of using Neutral EDTA for bone decalcification?
What is the primary advantage of using Neutral EDTA for bone decalcification?
What is the disadvantage of using Neutral EDTA?
What is the disadvantage of using Neutral EDTA?
What is the typical time frame for bone decalcification using Neutral EDTA?
What is the typical time frame for bone decalcification using Neutral EDTA?
Which decalcification method utilizes an ion exchange resin?
Which decalcification method utilizes an ion exchange resin?
What is the primary function of the ion exchange resin in decalcification?
What is the primary function of the ion exchange resin in decalcification?
What is the recommended decalcifying agent for minute bone spicules?
What is the recommended decalcifying agent for minute bone spicules?
What is a possible consequence of using Chromic Acid (Flemming's Fluid) for decalcification?
What is a possible consequence of using Chromic Acid (Flemming's Fluid) for decalcification?
Which decalcifying agent is NOT recommended for fluids containing mineral acids like nitric or hydrochloric acid?
Which decalcifying agent is NOT recommended for fluids containing mineral acids like nitric or hydrochloric acid?
What is a major disadvantage of using chromic acid for decalcification?
What is a major disadvantage of using chromic acid for decalcification?
What is a possible drawback of using electrophoresis for decalcification?
What is a possible drawback of using electrophoresis for decalcification?
What is a key advantage of the calcium oxalate test for decalcification?
What is a key advantage of the calcium oxalate test for decalcification?
Which of the following factors can influence the rate of decalcification?
Which of the following factors can influence the rate of decalcification?
Which of the following statements is TRUE regarding highly concentrated decalcifying solutions?
Which of the following statements is TRUE regarding highly concentrated decalcifying solutions?
What is the primary purpose of using a decalcifying solution after fixation and before impregnation?
What is the primary purpose of using a decalcifying solution after fixation and before impregnation?
Which of the following factors can negatively impact the quality of a specimen after decalcification?
Which of the following factors can negatively impact the quality of a specimen after decalcification?
Which of the following techniques is NOT commonly used for decalcification?
Which of the following techniques is NOT commonly used for decalcification?
Why is it unnecessary to decalcify toenails?
Why is it unnecessary to decalcify toenails?
Which of the following statements is TRUE regarding the decalcification process?
Which of the following statements is TRUE regarding the decalcification process?
Which decalcification method is best suited for small biopsies when rapid diagnosis is required within 24 hours or less?
Which decalcification method is best suited for small biopsies when rapid diagnosis is required within 24 hours or less?
What is a primary advantage of using Hydrochloric Acid for decalcification?
What is a primary advantage of using Hydrochloric Acid for decalcification?
What is a potential drawback of using Hydrochloric Acid for decalcification?
What is a potential drawback of using Hydrochloric Acid for decalcification?
What is the primary advantage of using Von Ebner’s Fluid for decalcification?
What is the primary advantage of using Von Ebner’s Fluid for decalcification?
What is a limitation of using Von Ebner’s Fluid for decalcification?
What is a limitation of using Von Ebner’s Fluid for decalcification?
Which of the following is NOT a characteristic of Formol-Nitric Acid?
Which of the following is NOT a characteristic of Formol-Nitric Acid?
Which decalcification method is considered inferior to Nitric acid?
Which decalcification method is considered inferior to Nitric acid?
Which decalcification method is best suited for large or heavily mineralized cortical bone specimens?
Which decalcification method is best suited for large or heavily mineralized cortical bone specimens?
What is the recommended fluid to tissue ratio for decalcification?
What is the recommended fluid to tissue ratio for decalcification?
Which of these factors will increase the rate of decalcification?
Which of these factors will increase the rate of decalcification?
How does the size of the tissue affect decalcification?
How does the size of the tissue affect decalcification?
What is the primary reason for rinsing decalcified specimens with running tap water?
What is the primary reason for rinsing decalcified specimens with running tap water?
How does suspending the tissue in decalcifying solution affect the decalcification process?
How does suspending the tissue in decalcifying solution affect the decalcification process?
What is the recommended duration for water rinsing of small tissue samples?
What is the recommended duration for water rinsing of small tissue samples?
What is the relationship between the density of bone and decalcification time?
What is the relationship between the density of bone and decalcification time?
How can the rate of decalcification be increased?
How can the rate of decalcification be increased?
Flashcards
Neutral EDTA
Neutral EDTA
A weak organic acid used for decalcification in histology.
Ion exchange resin
Ion exchange resin
Material that moves calcium into decalcifying solution, forming soluble calcium salts.
Decalcification process
Decalcification process
The procedure to remove calcium from specimens after fixation and before embedding.
Factors affecting decalcification
Factors affecting decalcification
Signup and view all the flashcards
Cartilage and decalcification
Cartilage and decalcification
Signup and view all the flashcards
Decalcification
Decalcification
Signup and view all the flashcards
Decalcifying agents
Decalcifying agents
Signup and view all the flashcards
Types of decalcifying agents
Types of decalcifying agents
Signup and view all the flashcards
Strong mineral acids
Strong mineral acids
Signup and view all the flashcards
Weak organic acids
Weak organic acids
Signup and view all the flashcards
Chelating agents
Chelating agents
Signup and view all the flashcards
Purpose of decalcification
Purpose of decalcification
Signup and view all the flashcards
Choosing a decalcifying agent
Choosing a decalcifying agent
Signup and view all the flashcards
EDTA formula
EDTA formula
Signup and view all the flashcards
Advantages of Neutral EDTA
Advantages of Neutral EDTA
Signup and view all the flashcards
Disadvantage of Neutral EDTA
Disadvantage of Neutral EDTA
Signup and view all the flashcards
Decalcification period for EDTA
Decalcification period for EDTA
Signup and view all the flashcards
Chromic acid formula
Chromic acid formula
Signup and view all the flashcards
Use of Chromic acid
Use of Chromic acid
Signup and view all the flashcards
Hydrochloric Acid
Hydrochloric Acid
Signup and view all the flashcards
Disadvantage of Chromic acid
Disadvantage of Chromic acid
Signup and view all the flashcards
Measurement of decalcification
Measurement of decalcification
Signup and view all the flashcards
Decalcification Time
Decalcification Time
Signup and view all the flashcards
Advantages of HCl
Advantages of HCl
Signup and view all the flashcards
Disadvantages of HCl
Disadvantages of HCl
Signup and view all the flashcards
Von Ebner’s Fluid
Von Ebner’s Fluid
Signup and view all the flashcards
Formol-Nitric Acid
Formol-Nitric Acid
Signup and view all the flashcards
Moderately Rapid Decalcifier
Moderately Rapid Decalcifier
Signup and view all the flashcards
Cytologic Staining
Cytologic Staining
Signup and view all the flashcards
Electrophoresis
Electrophoresis
Signup and view all the flashcards
Chromic acid risk
Chromic acid risk
Signup and view all the flashcards
Concentration impact
Concentration impact
Signup and view all the flashcards
Calcium Oxalate Test
Calcium Oxalate Test
Signup and view all the flashcards
Decalcification details
Decalcification details
Signup and view all the flashcards
Post-decalcification
Post-decalcification
Signup and view all the flashcards
Fluid to tissue ratio
Fluid to tissue ratio
Signup and view all the flashcards
Fluid access
Fluid access
Signup and view all the flashcards
Size and consistency
Size and consistency
Signup and view all the flashcards
Concentration of solutions
Concentration of solutions
Signup and view all the flashcards
Rinsing decalcified specimens
Rinsing decalcified specimens
Signup and view all the flashcards
Access increase
Access increase
Signup and view all the flashcards
Study Notes
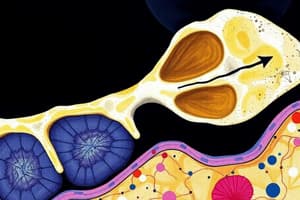
Decalcification
- Decalcification is the removal of calcium ions from bone or calcified tissue, making it easier to cut for histological processes
- It allows histotechnologists to prepare thin sections of bone for microscopic examination
- This crucial process happens after fixation and before embedding in paraffin
- Bone needs to be soft and flexible to be sectioned properly, and this can be achieved via decalcification
- Poorly fixed specimens may be macerated during the process, making staining difficult, particularly in bone marrow areas
Acid Decalcifying Agents
- Commonly used for routine decalcification of bone
- They are stable, readily available, and inexpensive
- Three main types: based on strong mineral acids, weak organic acids, or chelating agents
Strong Mineral Acids
- Nitric acid: Most common, fast-acting
- Hydrochloric acid: Slower than nitric acid, but better for nuclear staining
Weak Organic Acids
- Formic acid: Best all-around decalcifying agent, with good nuclear staining and less tissue distortion
- Trichloroacetic acid: Used for very small bone pieces; weaker acid.
Chelating Agents
- EDTA: Slow but effective, better for nucleic acids and enzymes; more time-consuming process
- Widely used for details requiring good nuclear staining
Factors Affecting Decalcification
- Concentration: Higher concentration increases the rate, but can harm tissues
- Fluid access: Increased access to decalcifying solution speeds up the process
- Size and consistency: Larger or denser tissues require more time
- Agitation: Gentle agitation aids in the process
- Temperature: Higher temperature increases rate, but also increases tissue damage risk
- Proper preservation is imperative before, during, and after decalcification to prevent damage to the specimen
Measuring the Extent of Decalcification
- Physical/Mechanical testing: Assessing tissue consistency by touching or bending; can cause damage if not done correctly
- X-ray/Radiological testing: Useful, but can be hindered by previous tissue fixation
Additional Notes
- Decalcification is a lengthy process, requiring days or even weeks, depending on the specimen's size and density
- Different decalcifying agents have varying effects on tissue structure and staining, influencing choice and duration
- Care should be taken when working with decalcifying agents, as they can be corrosive, hazardous, or carcinogenic
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.