Podcast
Questions and Answers
Which of the following best describes the role of coagulation inhibitors in hemostasis?
Which of the following best describes the role of coagulation inhibitors in hemostasis?
- They dissolve fibrin threads to form blood clots.
- They activate the blood coagulation mechanism to stop bleeding.
- They promote widespread clotting within blood vessels.
- They counterbalance coagulation factors and restrict the clotting process to a limited area. (correct)
How does antithrombin contribute to the regulation of blood coagulation?
How does antithrombin contribute to the regulation of blood coagulation?
- By inhibiting the activity of thrombin and other coagulation factors. (correct)
- By initiating the extrinsic pathway of coagulation.
- By activating plasminogen to form plasmin.
- By promoting the formation of fibrin threads.
A patient presents with small, red spots on their skin. This is most indicative of which condition?
A patient presents with small, red spots on their skin. This is most indicative of which condition?
- Intravascular coagulation.
- Thrombocytopenia. (correct)
- Hematoma.
- Von Willebrand disease.
A patient is diagnosed with Von Willebrand disease. Which of the following is a key characteristic of this condition?
A patient is diagnosed with Von Willebrand disease. Which of the following is a key characteristic of this condition?
What is the primary role of platelets in the process of hemostasis?
What is the primary role of platelets in the process of hemostasis?
Which of the following accurately describes the extrinsic pathway of blood coagulation?
Which of the following accurately describes the extrinsic pathway of blood coagulation?
If a patient is experiencing a disturbance in Phase 2 of blood coagulation, what is the most likely underlying issue?
If a patient is experiencing a disturbance in Phase 2 of blood coagulation, what is the most likely underlying issue?
Inadequate synthesis of vitamin K can lead to a disturbance in blood coagulation. What is the MOST likely reason for this?
Inadequate synthesis of vitamin K can lead to a disturbance in blood coagulation. What is the MOST likely reason for this?
Which of the following is the MOST likely cause of an arterial thrombus?
Which of the following is the MOST likely cause of an arterial thrombus?
What is the potential consequence of a thrombus forming in a coronary artery?
What is the potential consequence of a thrombus forming in a coronary artery?
What is the underlying mechanism by which increased coagulability can lead to thrombosis?
What is the underlying mechanism by which increased coagulability can lead to thrombosis?
How do tumors contribute to hypercoagulability and increase the risk of thrombosis?
How do tumors contribute to hypercoagulability and increase the risk of thrombosis?
What is the MAIN underlying cause of edema?
What is the MAIN underlying cause of edema?
Increased capillary permeability is a potential cause of edema. Which of the following conditions BEST exemplifies this mechanism?
Increased capillary permeability is a potential cause of edema. Which of the following conditions BEST exemplifies this mechanism?
What is the MOST direct effect of decreased cardiac output in cardiogenic shock?
What is the MOST direct effect of decreased cardiac output in cardiogenic shock?
A patient in shock presents with cool, clammy skin, rapid heart rate and low blood pressure. What is the MOST likely underlying mechanism causing these signs?
A patient in shock presents with cool, clammy skin, rapid heart rate and low blood pressure. What is the MOST likely underlying mechanism causing these signs?
A patient is diagnosed with ischemia. What is the underlying problem?
A patient is diagnosed with ischemia. What is the underlying problem?
During ventricular systole, what is the state of the atrioventricular (AV) valves and semilunar (SL) valves?
During ventricular systole, what is the state of the atrioventricular (AV) valves and semilunar (SL) valves?
What is the PRIMARY function of the coronary circulation?
What is the PRIMARY function of the coronary circulation?
What is the correct sequence of the cardiac conduction system?
What is the correct sequence of the cardiac conduction system?
Which factor primarily determines systolic blood pressure?
Which factor primarily determines systolic blood pressure?
An ECG is used to identify which of the following?
An ECG is used to identify which of the following?
What is the key difference between atrial fibrillation and atrial flutter on an ECG?
What is the key difference between atrial fibrillation and atrial flutter on an ECG?
Which treatment strategies aim to reduce the risk of thrombus formation in patients with atrial fibrillation?
Which treatment strategies aim to reduce the risk of thrombus formation in patients with atrial fibrillation?
What is a critical step in the immediate management of cardiac arrest?
What is a critical step in the immediate management of cardiac arrest?
If a patient is experiencing stenosis of a heart valve, what is the MOST direct hemodynamic consequence?
If a patient is experiencing stenosis of a heart valve, what is the MOST direct hemodynamic consequence?
What is the underlying mechanism in rheumatic fever that leads to heart valve damage?
What is the underlying mechanism in rheumatic fever that leads to heart valve damage?
Increased peripheral resistance leads to increased workload on the heart resulting in what condition?
Increased peripheral resistance leads to increased workload on the heart resulting in what condition?
High cholesterol, diabetes, hypertension and smoking are considered what in regards to hypertension?
High cholesterol, diabetes, hypertension and smoking are considered what in regards to hypertension?
Flashcards
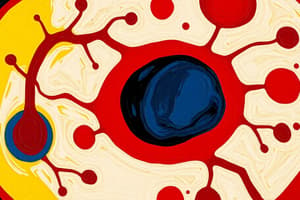
Hemostasis
Hemostasis
Arrest of bleeding caused by activation of the blood coagulation mechanism.
Blood Clot
Blood Clot
Interlacing meshwork of fibrin threads with plasma, red cells, white cells, and platelets.
Coagulation Inhibitors
Coagulation Inhibitors
Coagulation factors counterbalanced by coagulation inhibitors.
Plasmin
Plasmin
Signup and view all the flashcards
Thrombocytopenia
Thrombocytopenia
Signup and view all the flashcards
Petechiae
Petechiae
Signup and view all the flashcards
Von Willebrand Disease
Von Willebrand Disease
Signup and view all the flashcards
Hematoma
Hematoma
Signup and view all the flashcards
Intravascular
Intravascular
Signup and view all the flashcards
Virchow's Triad
Virchow's Triad
Signup and view all the flashcards
Embolus
Embolus
Signup and view all the flashcards
Infarct
Infarct
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Shock
Shock
Signup and view all the flashcards
Ischemia
Ischemia
Signup and view all the flashcards
Cardiomyopathies
Cardiomyopathies
Signup and view all the flashcards
Stenosis
Stenosis
Signup and view all the flashcards
Insufficiency (Regurgitation)
Insufficiency (Regurgitation)
Signup and view all the flashcards
Thrombophlebitis
Thrombophlebitis
Signup and view all the flashcards
Myocardial Infarction
Myocardial Infarction
Signup and view all the flashcards
Cardiac arrest
Cardiac arrest
Signup and view all the flashcards
Chronic heart failure
Chronic heart failure
Signup and view all the flashcards
Rapidly failing heart
Rapidly failing heart
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Less likely to rupture
Less likely to rupture
Signup and view all the flashcards
Carry cholesterol to tissues for utilization, BAD
Carry cholesterol to tissues for utilization, BAD
Signup and view all the flashcards
Carry cholesterol not used by the tissues back to the liver for metabolism or excretion in bile, GOOD
Carry cholesterol not used by the tissues back to the liver for metabolism or excretion in bile, GOOD
Signup and view all the flashcards
Angina pectoris
Angina pectoris
Signup and view all the flashcards
Study Notes
Chapter 14: Hemostasis
- Hemostasis is the process of stopping bleeding through blood coagulation.
- Hemostasis can occur via blood clot, vessel spasm, or physical means like compression/bandage.
- A blood clot is a meshwork of fibrin threads, plasma, and blood cells.
- Coagulation inhibitors are coagulation factors that restrict clotting.
- Plasmin dissolves fibrin and is formed when plasminogen is activated into plasmin (fibrinolysin).
- Thrombocytopenia means having a deficiency in platelets.
- Petechiae are small spots, indicating defective platelets, or a capillary defect.
- Von Willebrand disease is an autosomal dominant bleeding disorder caused by inadequate protein.
- Hematoma: Large hemorrhage that results from a deficiency of plasma coagulation factors.
- Intravascular means inside blood vessels and disseminated means widespread.
Factors Concerned with Hemostasis
- Key factors include small blood vessel integrity, which is the body's first defense.
- Also important are having enough platelets.
- Normal levels of coagulation factors and inhibitors and calcium are also required.
Important Platelet Functions
- Platelets plug defects in vessel walls.
- Platelets liberate vasoconstrictors and compounds, causing platelet aggregation.
- Platelets initiate coagulation by releasing necessary substances.
Blood Coagulation Process
- Phase 1: Prothrombin activator is generated through intrinsic (blood-derived) and extrinsic (tissue injury) systems.
- Both pathways activate simultaneously and interact to initiate the clotting process.
- Both pathways generate thromboplastin to form prothrombin activator.
- Phase 2: Prothrombin converts to thrombin.
- Phase 3: Fibrinogen converts into fibrin by thrombin.
- A blood clot forms at the end of Phase 3.
Coagulation Inhibitor Example
- Antithrombin is an example of a coagulation inhibitor.
Four Categories of Coagulation Disturbances
- Abnormalities include small blood vessel issues, abnormal bleeding, and abnormal vessel formation.
- Disturbances may also arise from platelet formation abnormalities.
- Deficiencies can occur in plasma coagulation factors.
- Thromboplastic material can liberate into circulation.
Causes of Thrombocytopenia
- Injury or disease of the bone marrow can damage megakaryocytes, the precursors of platelets.
- Bone marrow infiltration by leukemic/cancer cells crowds out megakaryocytes.
- Antiplatelet antibodies can destroy platelets in peripheral blood, resulting in an autoimmune disease.
- Abnormal platelet function despite normal platelet count can cause thrombocytopenia.
Phase 1 Disturbance: Hemophilia
- Hemophilia is an X-linked hereditary disease primarily affecting males, characterized by hemorrhage episodes in joints and internal organs after minor injuries.
- Hemophilia A is classic hemophilia, involving Factor VIII (antihemophilic factor).
- Hemophilia B, or Christmas disease, involves Factor IX (Christmas factor).
Phase 2 Disturbance
- Phase 2 disturbance arises from a deficiency of prothrombin or factors required for prothrombin to convert into thrombin.
- Factors necessary for Phase 2 are produced in the liver.
- Vitamin K is crucial for their synthesis.
- Vitamin K is synthesized by intestinal bacteria or obtained from food.
- Bile is needed for Vitamin K absorption.
Prothrombin Deficiency Indicators
- Anticoagulant drugs inhibit active clotting factors.
- Inadequate vitamin K synthesis occurs due to intestinal bacteria death from antibiotic use.
- Bile duct blockage inhibits vitamin K absorption.
- Impaired liver synthesis leads to inadequate coagulation factors.
Thromboplastic Activity
- Events with thromboplastic activity, liberating into circulation, result in intravascular coagulation.
- These events include diseases linked to shock, tissue necrosis, and overwhelming bacterial infections
Disseminated Intravascular Syndrome
- Disseminated Intravascular Syndrome is a rare clotting disorder leading to abnormal bleeding, preventing deadly clot formation.
Chapter 12: Diseases of Blood Circulation
- Virchow's triad refers to the three categories of factors contributing to thromboses.
- A thrombus is an intravascular clot.
- Thrombi usually form in the deep veins of the legs, known as deep venous thrombosis (DVT).
- An embolus is a detached clot blocking smaller blood canals, leading to necrosis.
- An infarct is tissue necrosis caused by blocked blood flow.
- Edema is a fluid accumulation in tissues, commonly presented as swelling.
- Shock is when the circulatory system fails to deliver enough blood to body parts and causes organ failure.
- Shock is always life-threatening.
Virchow's Triad Factors
- Slowing or stasis of blood flow.
- Blood vessel wall damage.
- Increased blood coagulability.
Predisposing Factors for Venous Thrombosis
- Prolonged bed rest or cramped positions.
- Impaired leg muscle "milking action" hinders venous return.
- Other factors include varicose veins and increased blood coagulability.
- Possible outcomes are pulmonary embolism and leg swelling from venous return blockage.
- In pulmonary embolism, a clot detaches and lodges inside the pulmonary artery.
Clinical Manifestation Dependence
- Clinical manifestations depend on the embolus size and location within the pulmonary artery.
Lung Damage from Pulmonary Emboli
- Large pulmonary emboli block blood flow, causing severe dyspnea, cyanosis, shock, and sudden death.
- Small pulmonary emboli block pulmonary arteries, leading to wedge-shaped pulmonary infarcts.
- If infarcts develop, symptoms are dyspnea, pleuritic chest pain, cough, and hemoptysis.
Diagnosis and Treatment of Pulmonary Emboli
- Chest X-rays detect infarct but not the embolus itself.
- Radioisotope lung scans detect abnormal pulmonary blood flow caused by embolism.
- Pulmonary angiograms are the gold standard for detecting blocked pulmonary arteries.
- Computed tomography (CT) detects pulmonary embolism by showing obstructed contrast medium flow.
- Treatment includes general supportive care, anticoagulation, thrombolytic drugs, and surgery for large embolisms.
Main Cause of Arterial Thrombus
- Arterial thrombus formation is mainly caused by arteriosclerosis, through injury to the vessel wall.
Types & Effects of Arterial Thrombus
- Coronary artery thrombus leads to myocardial infarction.
- Major leg artery thrombus leads to gangrene.
- Cerebral artery thrombus leads to stroke.
What is Gangrene
- Gangrene is tissue death caused by blood flow loss due to illness, injury, or infection.
- It typically affects fingers, toes, and limbs but can also affect other body art.
Causes & Results of Intracardiac Thrombi
- Clots form within atrial appendages, heart valve surfaces, or the ventricular wall.
- Portions may dislodge into systemic circulation and lead to infarction in the spleen, kidneys, or brain.
Factors Increasing Thrombosis Risk
- Raised levels of coagulation factors follow surgery or injury due to thromboplastin release.
- Estrogen in contraceptive pills or pregnancy stimulates clotting factor synthesis.
- Hereditary gene mutations can cause abnormal factor V Leiden.
Genetic Factors Increasing Thrombosis Risk
- Factor V Leiden mutation results in factor V resistance and increased coagulability.
- Mutation of genes regulating prothrombin synthesis also increases the risk.
- A raised prothrombin level leads to greater venous thrombosis.
Thrombosis in Cancer Patients
- Higher levels of coagulation factors and platelets in cancer patients lead to risk.
- It predisposes patients to both arterial and venous thrombosis.
- The hypercoagulability comes from tumor deposits releasing thromboplastic materials.
- Tumors release thromboplastic material continuously, causing production of coagulation factors to exceed destruction.
Causes of Edema
- Edema disturbances arise from the extracellular fluid circulation between capillaries and interstitial fluid.
Factors Regulating Fluid Flow
- Capillary hydrostatic pressure pushes fluid into the extracellular space.
- Capillary permeability dictates fluid flow through the endothelium.
- Osmotic pressure attracts water exerted by blood proteins, drawing fluid from the interstitial back into capillaries.
- Open lymphatic channels collect fluid and return it to circulation.
Types of Edema
- Pitting edema leaves an indentation upon fingertip compression.
- Pleural effusion (hydrothorax) involves fluid accumulation in the pleural cavity.
- Ascites is fluid accumulation in the peritoneal cavity.
Four Causes of Edema
- Increased capillary permeability can cause swelling of tissues.
- EX: Acute inflammation or systemic disease
- Low plasma proteins causes excess protein loss or inadequate synthesis.
- EX: Kidney disease, malnutrition, or liver failure
- Increased hydrostatic pressure may arise from heart failure or localized venous obstruction.
- Lymphatic obstruction blocks fluid return from the interstitial space.
- EX:
Categories, Causes and Shock
- Shock results from low blood pressure.
- Its result is inadequate organ/tissue perfusion.
Hypovolemic Shock
- Hypovolemic shock is caused by low blood volume, which leads from hemorrhage, dehydration, severe burns, diarrhea and diuretic use.
Cardiogenic Shock
- Cardiogenic shock is inadequate cardiac output when the heart cannot effectively pump blood.
- It is caused by myocardial infarction (reducing pumping function) and pericardial effusion (prevents heart filling).
Septic Shock
- Septic shock is excessive vasodilation from release of microbial toxins and inflammatory mediators.
Anaphylactic Shock
- Anaphylactic shock is excessive vasodilation from release of inflammatory mediators caused by an allergic reaction.
Shock Signs & Symptoms
- Skin is cool, clammy, and pale.
- Weakness, dizziness, thirst and nausea are common.
- Breathing may be shallow and rapid, with a weak, rapid pulse.
- Blood pressure is low, and lips/fingernails can be cyanotic.
- Patients may be confused or suddenly unconscious
- Drugs like vasoconstrictors are used to help symptoms.
- Prognosis relies on early recognition and treatment.
- Treatments include fluids/blood and treatment of the underlying cause.
Chapter 11 Diseases of the Heart and Circulation
- Diastole is when the heart muscle relaxes.
- Systole is when the heart muscle contracts.
- Ischemia occurs when a body part gets insufficient blood.
- Dr. Bernard Lown invented the defibrillator and was a 1985 Nobel laureate.
- Cardiomyopathies causes mechanical and/or electrical dysfunction often causing ventricular hypertrophy/dilation and can stem from genetics, etc.
Heart Function
- The heart's primary function is to pump blood through the lungs and to the rest of the body.
Heart Layers
- Epicardium: outer connective tissue layer with coronary arteries.
- Myocardium: middle, muscular layer, workhorse of the heart.
- Endocardium: innermost, smooth layer that lines chambers and heart valves.
- Pericardium surrounds the heart in a double-walled sac reducing friction.
Right vs Left Circulations
- Right side: Pulmonary circulation
- Left side: Systemic circulation
Heart Valves
- Atrioventricular valves: tricuspid (RA to RV) and bicuspid/mitral (LA to LV).
- Semilunar valves: pulmonary (RV to pulmonary trunk) and aortic (LV to aorta).
Blood Flow Through the Heart
- Blood flows from the superior/inferior vena cava to the right atrium (RA).
- Then it goes through the tricuspid valve to the right ventricle (RV).
- From the RV, it passes through the pulmonary valve to the lungs.
- Next, it enters the left atrium (LA) and goes through the bicuspid/mitral valve to the left ventricle (LV).
- Finally, it goes through the aortic valve to the aorta.
Coronary Circulation
- Coronary circulation provides the heart its own blood supply.
- The right coronary artery (RCA) supplies the posterior wall and interventricular septum.
- The left coronary artery (LCA) branches.
- LCA supplies to the anterior wall and anterior interventricular septum . : LCA supplies to the lateral wall
Cardiac Conduction System
- Cardiac conduction consists of events associated with one complete heartbeat.
- Atrial systole atrial diastole ventricular systole ventricular diastole.
- Key components are SA node, AV node, bundle of HIS, and Purkinje fibers.
Phases of the Cardiac Cycle
- Diastole: Chambers relax, blood flows through open AV valves; SL valves are closed.
- Atrial Systole: Additional blood flows into ventricles.
- Ventricular Systole: Ventricles contract, AV valves close, SL valves open when pressure builds.
- Diastole: Chambers relax, SL valves close, AV valves open, and blood flows into chambers.
Types of Blood Vessels
- Large elastic arteries carry blood throughout the body.
- Arterioles regulate flow from arteries to capillaries.
- Capillaries deliver nutrients and remove waste with their endothelium.
- Veins return blood to the heart under low pressure.
Systolic vs. Diastolic Blood Pressure
- Blood flow in the arteries results from ventricular contractions.
- Systolic pressure is the highest when ventricles contract.
- Diastolic pressure is lowest when ventricles relax.
Electrocardiogram (ECG/EKG)
- Electrocardiograms measure the heart's electrical activity and identify disturbances in rate, conduction, rhythm, injury, and extent of muscle damage.
- The deflections of the ECG are labeled P, Q, R, S, and T.
Arrhythmias: Signs, Symptoms & Etiology
- Arrhythmias are any deviation from the normal sinus rhythm (heartbeat).
- Symptoms: palpitations, tachycardia, bradycardia, syncope, fatigue, skipped heartbeats.
- Etiology: interference within the conduction system of the heart, ischemia and drugs.
Normal Sinus Rhythm
- An electrocardiogram (ECG) reads within normal limits with a heart rate between 60-100 bpm.
- Sinus bradycardia causes a regular rhythm with a heart rate of <60 bpm.
- Sinus tachycardia causes a heart rate of >100 bpm.
Atrial Fibrillation
- Atrial fibrillation is seen in older persons, and patients with CVD, COPD, hyperthyroidism and causes rapid atrial contractions and atrial "quivering".
- An electrocardiogram shows small, irregular, disorganized P waves.
- Ventricles beat irregularly at 140-160 bpm during atrial fibrillation, leading to shortened filling time.
- The goal of treatment of arrythmia is to decrease heart rate and restore normal rhythm.
- A watchman device may be used for treatment.
PVCs and Cardiac Arrest
- Extrasystole characterized by a beat early in time, missing p wave.
- Is considered normal and is caused by stress, diet.
- Ventricular contraction characterized by 3 or more PVCs- can be life threatening.
- Rapid hearbeat is called cardiac arrest.
Medical Interventions
- Stoppage of drugs with the adverse affect drug induced arrhythmias.
- Electrical countershock- cardioversion- delivers electrical pulses in order to convert heartbeat.
Valvular Malfunction
- 2 types of valvular malfunction Stenosis: hardening of cusp and insufficiency (incompetence, regurgitation): valve not close.
- Rheumatic fever: antigen-antibody react injures connectivity in tissue, can cause inflammation/clinical outcomes and prevented with the right treatment.
Causes of Rheumatic heart Disease
- The rheumatic heart disease has valves become red then swollen- leads to stress on heart failure.
- It it prevented beta strep infection from occurring (leads to valve damage).
Types of non Rheumatic aortic
- Non-rheumatic: occurs if the heart has 2 valves instead of 3: this can lead to further complications such as heart stress failure.
- Mitral valve prolaspe : abnormal chord length that causes regurgitation.
Infective endocarditis
- Vegetations builds up in heart: bacterial is most relevant.
- Causes leaflet erosion and infection in blood.
Interventions for Sub endocarditis
- Those at high risk should receive sub acute for protection.
- Acute endocarditis is where the affecter is highly pathogenic- such as a drug users.
Hypertension
- High vascular and excessive amounts of smooth muscle from constrictive arterioles.
- Asymptomatic if occurs from genetic disease: risk include sedentary diseases.
Diagnosing elevated high pressure
- elevated BP> changes needed, with high BP risk comes 1-= year heart disease.
- Primary elevated pressure cause be a result of a BP control mechanism.
- The main BP control mechanisms are kidney, hormone control and thyroid.
Main points of hypotension
- Increased heart rate puts higher strain, leads to heart failure.
- Atherosclerosis increased, which then weakens area to the degree of potential harm.
- Goal through medication is dilation to ensure blood can move freely.
- Myocarditis: occurs from direct muscle inflammation, viral trigger and can lead to failure.
Types of cardiomyopathies:
- Muscle disease to the point of heart failure and hypertension on a number of issues.
- Hypertrophic cardiomyopathy: increases size can obstruct flow and cause block- usually asymptomatic.
Types of cardiac diseases;
- Ventricular failure- blood failure with systematic complications- causes lung blockage.
- The 4 main causes of congenital heart disease are: block age of flow.
- Causes a mixing and failure to close/complete- resulting in need for surgery with a heart replacement.
- There are 2 types of aneurysm: one side is not formed properly- need for drugs (smoking/stress).
- Thrombosis occurs in all vascular- can cause a dissecting damage leading to stroke.
Types of vessels disease: cause and how can we maintain.
- Vein have low pressure that can result in venous damages which can be treated through the intervention.
- Atherosclerosis is build pressure on walls arteries: this can lead to ruptures.
- Stable plaques do not rupture as often and can result in a high amounts of strokes.
Case Notes
- Angina is the first stage of cardiovascular disease.
- The goal of an interventions is for decrease the prelaod/afterload which overall reduces workload of heart.
- CHF or congestive heart failure has to do with stress on organ/organ failures.
- Pleural effusion: is caused from adima/liver problems.
- Anuria's is the increase is blood output with lack blood in blood.
- CHF occurs when heat isn't working right- one has high output during this instance, this can be reduced with good habits.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.