Podcast
Questions and Answers
What is the primary mechanism by which the body prevents widespread coagulation during hemostasis?
What is the primary mechanism by which the body prevents widespread coagulation during hemostasis?
- Activating clotting factors at the site of injury.
- Increasing blood flow to dilute clotting factors.
- Inactivating clotting factors that stray from the vessel injury. (correct)
- Releasing tissue plasminogen activator (tPA) to initiate fibrinolysis.
How does antithrombin contribute to the regulation of hemostasis?
How does antithrombin contribute to the regulation of hemostasis?
- By promoting the aggregation of platelets to form a plug.
- By activating the coagulation cascade.
- By inactivating clotting factors. (correct)
- By enhancing the production of fibrin.
What is the role of tissue plasminogen activator (tPA) in fibrinolysis?
What is the role of tissue plasminogen activator (tPA) in fibrinolysis?
- It inhibits the formation of plasmin.
- It activates plasminogen to form plasmin. (correct)
- It stabilizes the fibrin meshwork.
- It promotes platelet aggregation.
What does an elevated concentration of plasma D-dimer typically indicate?
What does an elevated concentration of plasma D-dimer typically indicate?
What is the primary difference between a thrombus and an embolus?
What is the primary difference between a thrombus and an embolus?
What characteristics are associated with a white thrombus?
What characteristics are associated with a white thrombus?
How is Prothrombin Time (PT) used in hemostasis measurement?
How is Prothrombin Time (PT) used in hemostasis measurement?
What is the clinical significance of the International Normalized Ratio (INR) in hemostasis?
What is the clinical significance of the International Normalized Ratio (INR) in hemostasis?
How does Anti-Factor Xa activity testing aid in hemostasis management?
How does Anti-Factor Xa activity testing aid in hemostasis management?
Which condition is characterized by a decreased number of platelets?
Which condition is characterized by a decreased number of platelets?
What deficiency primarily characterizes Hemophilia A?
What deficiency primarily characterizes Hemophilia A?
What critical factor differentiates the manifestations of hemophilia?
What critical factor differentiates the manifestations of hemophilia?
What are the three key components that contribute to the etiology of Deep Vein Thrombosis (DVT)?
What are the three key components that contribute to the etiology of Deep Vein Thrombosis (DVT)?
Which clinical manifestation is commonly associated with Deep Vein Thrombosis (DVT)?
Which clinical manifestation is commonly associated with Deep Vein Thrombosis (DVT)?
Which of the following is a serious complication of DVT (Deep Vein Thrombosis)?
Which of the following is a serious complication of DVT (Deep Vein Thrombosis)?
What are the primary clinical manifestations associated with Pulmonary Embolism (PE)?
What are the primary clinical manifestations associated with Pulmonary Embolism (PE)?
A patient with a history of myocardial infarctions is prescribed an antiplatelet. What is the primary goal of antiplatelet therapy in this context?
A patient with a history of myocardial infarctions is prescribed an antiplatelet. What is the primary goal of antiplatelet therapy in this context?
How do anticoagulant medications primarily function to prevent clot formation?
How do anticoagulant medications primarily function to prevent clot formation?
What is a critical consideration when administering medications that alter the hemostasis process before a surgical procedure?
What is a critical consideration when administering medications that alter the hemostasis process before a surgical procedure?
What advice should healthcare providers give patients at risk of bleeding who are considering taking over-the-counter (OTC) medications?
What advice should healthcare providers give patients at risk of bleeding who are considering taking over-the-counter (OTC) medications?
What is the mechanism of action for aspirin as an antiplatelet drug?
What is the mechanism of action for aspirin as an antiplatelet drug?
Why should aspirin be avoided in children and teenagers with viral infections?
Why should aspirin be avoided in children and teenagers with viral infections?
After the discontinuation of Aspirin, how long does it take for the effects to subside?
After the discontinuation of Aspirin, how long does it take for the effects to subside?
A patient is prescribed clopidogrel (Plavix) after a stent placement. What is the primary mechanism of action of this drug?
A patient is prescribed clopidogrel (Plavix) after a stent placement. What is the primary mechanism of action of this drug?
What is a BBW (Black Box Warning) associated with the use of clopidogrel?
What is a BBW (Black Box Warning) associated with the use of clopidogrel?
What lab value should be monitored in a patient taking clopidogrel?
What lab value should be monitored in a patient taking clopidogrel?
How does eptifibatide (Integrilin) inhibit platelet aggregation?
How does eptifibatide (Integrilin) inhibit platelet aggregation?
What route of administration is used for eptifibatide (Integrilin)?
What route of administration is used for eptifibatide (Integrilin)?
What is the primary mechanism of action of unfractionated heparin (UFH)?
What is the primary mechanism of action of unfractionated heparin (UFH)?
What is a potential hypersensitivity reaction with UFH?
What is a potential hypersensitivity reaction with UFH?
What monitoring is essential when administering unfractionated heparin (UFH)?
What monitoring is essential when administering unfractionated heparin (UFH)?
How does low molecular weight heparin (LMWH) such as enoxaparin, work in the body?
How does low molecular weight heparin (LMWH) such as enoxaparin, work in the body?
Compared to unfractionated heparin (UFH), what is a key advantage of using low molecular weight heparin (LMWH)?
Compared to unfractionated heparin (UFH), what is a key advantage of using low molecular weight heparin (LMWH)?
What is the primary mechanism through which Warfarin exerts its anticoagulant effects?
What is the primary mechanism through which Warfarin exerts its anticoagulant effects?
Which laboratory test is essential for monitoring warfarin therapy?
Which laboratory test is essential for monitoring warfarin therapy?
What dietary advice should be given to a patient newly prescribed warfarin?
What dietary advice should be given to a patient newly prescribed warfarin?
What is a key advantage of using direct-acting oral anticoagulants (DOACs) over warfarin?
What is a key advantage of using direct-acting oral anticoagulants (DOACs) over warfarin?
What is the primary mechanism of action of thrombolytic drugs like alteplase (tPA)?
What is the primary mechanism of action of thrombolytic drugs like alteplase (tPA)?
What is an important consideration when administering thrombolytic medications?
What is an important consideration when administering thrombolytic medications?
What makes the timing of the administration important when dealing with thrombolytics?
What makes the timing of the administration important when dealing with thrombolytics?
What initiates the process of primary hemostasis following an injury to a blood vessel?
What initiates the process of primary hemostasis following an injury to a blood vessel?
How do clotting factors contribute to secondary hemostasis?
How do clotting factors contribute to secondary hemostasis?
What is the role of fibrin in the context of secondary hemostasis?
What is the role of fibrin in the context of secondary hemostasis?
What is the primary function of plasmin during fibrinolysis?
What is the primary function of plasmin during fibrinolysis?
How does the formation of a thrombus differ from the formation of an embolus?
How does the formation of a thrombus differ from the formation of an embolus?
Which of the following characterizes a white thrombus compared to a red thrombus?
Which of the following characterizes a white thrombus compared to a red thrombus?
What information does the activated partial thromboplastin time (aPTT) provide about hemostasis?
What information does the activated partial thromboplastin time (aPTT) provide about hemostasis?
Why is it essential to calibrate Anti-Factor Xa activity testing for the specific anticoagulant used?
Why is it essential to calibrate Anti-Factor Xa activity testing for the specific anticoagulant used?
What is the underlying issue in hemophilia that leads to increased bleeding?
What is the underlying issue in hemophilia that leads to increased bleeding?
Which combination of factors primarily contributes to the development of Deep Vein Thrombosis (DVT)?
Which combination of factors primarily contributes to the development of Deep Vein Thrombosis (DVT)?
What physiological processes are affected by antiplatelet drugs?
What physiological processes are affected by antiplatelet drugs?
How does Aspirin exert its antiplatelet effects?
How does Aspirin exert its antiplatelet effects?
For which condition is aspirin use specifically contraindicated in children and teenagers?
For which condition is aspirin use specifically contraindicated in children and teenagers?
By what mechanism does clopidogrel inhibit platelet aggregation?
By what mechanism does clopidogrel inhibit platelet aggregation?
How does Eptifibatide inhibit platelet aggregation?
How does Eptifibatide inhibit platelet aggregation?
Which property is unique to low molecular weight heparins (LMWH) like enoxaparin, differing from unfractionated heparin (UFH)?
Which property is unique to low molecular weight heparins (LMWH) like enoxaparin, differing from unfractionated heparin (UFH)?
How does warfarin reduce the synthesis of Vitamin K-dependent clotting factors?
How does warfarin reduce the synthesis of Vitamin K-dependent clotting factors?
What is a critical consideration for patients regarding their diet when they are prescribed warfarin?
What is a critical consideration for patients regarding their diet when they are prescribed warfarin?
What is the primary strategy employed during a 'bridging therapy' when initiating warfarin treatment?
What is the primary strategy employed during a 'bridging therapy' when initiating warfarin treatment?
Which best describes how thrombolytic medications function to remove existing clots?
Which best describes how thrombolytic medications function to remove existing clots?
Following an injury to a blood vessel, what is the immediate response of the vessel to reduce blood flow?
Following an injury to a blood vessel, what is the immediate response of the vessel to reduce blood flow?
How are clotting factors generally synthesized and maintained in the body?
How are clotting factors generally synthesized and maintained in the body?
What is the primary role of antithrombin in the coagulation process?
What is the primary role of antithrombin in the coagulation process?
Which of the following laboratory results indicates a normal range for platelet count in adults?
Which of the following laboratory results indicates a normal range for platelet count in adults?
What is the common treatment for hemophilia A?
What is the common treatment for hemophilia A?
Which condition is NOT typically categorized under 'Clots are the problem' in hemostasis disorders?
Which condition is NOT typically categorized under 'Clots are the problem' in hemostasis disorders?
What adverse effect is most concerning with antiplatelet, anticoagulants, and thrombolytic mediations?
What adverse effect is most concerning with antiplatelet, anticoagulants, and thrombolytic mediations?
What is the primary goal of anticoagulant medications?
What is the primary goal of anticoagulant medications?
When should the administration of thrombolytics be avoided?
When should the administration of thrombolytics be avoided?
Flashcards
Hemostasis
Hemostasis
The process by which bleeding is stopped, leading to the formation of a clot.
Vascular Spasm
Vascular Spasm
A process initiated by blood vessel injury, leading to reduced blood flow through vasoconstriction.
Primary Hemostasis
Primary Hemostasis
The initial phase of hemostasis where platelets adhere, activate, and aggregate to form a temporary plug at the injury site.
Secondary Hemostasis (Coagulation)
Secondary Hemostasis (Coagulation)
Signup and view all the flashcards
Clotting Factors
Clotting Factors
Signup and view all the flashcards
Antithrombin
Antithrombin
Signup and view all the flashcards
Fibrinolysis
Fibrinolysis
Signup and view all the flashcards
D-dimer
D-dimer
Signup and view all the flashcards
Thrombus
Thrombus
Signup and view all the flashcards
Embolus
Embolus
Signup and view all the flashcards
White Thrombus
White Thrombus
Signup and view all the flashcards
Red Thrombus
Red Thrombus
Signup and view all the flashcards
Prothrombin Time (PT)
Prothrombin Time (PT)
Signup and view all the flashcards
INR (International Normalized Ratio)
INR (International Normalized Ratio)
Signup and view all the flashcards
Activated Partial Thromboplastin Time (aPTT)
Activated Partial Thromboplastin Time (aPTT)
Signup and view all the flashcards
Complete Blood Count (CBC)
Complete Blood Count (CBC)
Signup and view all the flashcards
Thrombocytopenia
Thrombocytopenia
Signup and view all the flashcards
Hemophilia
Hemophilia
Signup and view all the flashcards
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT)
Signup and view all the flashcards
Pulmonary Embolism (PE)
Pulmonary Embolism (PE)
Signup and view all the flashcards
Antiplatelets
Antiplatelets
Signup and view all the flashcards
Prevention of clot formation
Prevention of clot formation
Signup and view all the flashcards
Anticoagulants
Anticoagulants
Signup and view all the flashcards
Thrombolytics (Fibrinolytics)
Thrombolytics (Fibrinolytics)
Signup and view all the flashcards
Aspirin
Aspirin
Signup and view all the flashcards
Clopidogrel
Clopidogrel
Signup and view all the flashcards
Eptifibatide
Eptifibatide
Signup and view all the flashcards
Anticoagulants
Anticoagulants
Signup and view all the flashcards
Unfractionated Heparin (UFH)
Unfractionated Heparin (UFH)
Signup and view all the flashcards
Low Molecular Weight Heparin (LMWH)
Low Molecular Weight Heparin (LMWH)
Signup and view all the flashcards
Warfarin
Warfarin
Signup and view all the flashcards
The mechanism of action for Warfarin
The mechanism of action for Warfarin
Signup and view all the flashcards
Why would time to be considered when using Thrombolytics?
Why would time to be considered when using Thrombolytics?
Signup and view all the flashcards
Study Notes
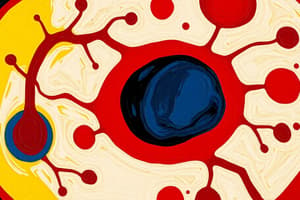
Hemostasis
- The process of stopping bleeding and forming a clot.
- Operates through positive feedback mechanisms.
- Injury to a blood vessel causes blood leakage, vasospasm, and exposure of collagen and other chemicals.
Clotting Processes
- Primary hemostasis involves platelet plug formation.
- Secondary hemostasis involves coagulation.
Primary Hemostasis: Platelet Plug Formation
- A damaged blood vessel exposes collagen.
- Chemicals cause platelets to adhere to the injury site, activate surrounding platelets, and aggregate to form a plug.
Secondary Hemostasis: Coagulation
- Coagulation forms fibrin through enzymatic reactions via clotting factors.
- Fibrin creates a meshwork to stabilize the platelet plug.
- Clotting factors are proteins made in the liver, circulating inactive until coagulation is activated.
- These factors instigate enzymatic reactions that result in fibrin formation.
- Fibrin threads create a meshwork, trapping blood constituents of the platelet plug, forming a clot.
Control of Coagulation
- The body inactivates stray clotting factors to prevent widespread coagulation.
- Antithrombin is a protein that inactivates clotting factors.
Fibrinolysis
- This is the clot removal process essential for healing.
- Fibrinolysis initiates within 24-48 hours after clot formation and continues until the clot dissolves.
- Plasmin is the main enzyme responsible for fibrinolysis.
- Plasmin starts dissolving the fibrin meshwork when blood vessel cells secrete tissue plasminogen activator (tPA).
D-dimer
- This is a major fibrin degradation product.
- Elevated plasma D-dimer concentrations indicate recent or ongoing intravascular coagulation and fibrinolysis.
Types of Hemostasis
- Primary hemostasis: Platelets adhere at the trauma site where they aggregate to create a blockage.
- Secondary hemostasis: Insoluble fibrin strands produce coagulation to reinforce this blockage.
Types of Thrombi
- A thrombus is a stationary clot within a blood vessel.
- An embolus is a thrombus fragment that breaks off and travels through the bloodstream.
- White thrombi (white clots) typically occur in arteries with fast blood flow, made mostly of platelets and fibrin.
- Red thrombi (red clots) typically occur in veins with slower blood flow, made mostly of RBCs and fibrin.
Hemostasis Measurement
- Complete Blood Count (CBC) measures platelet value.
- Prothrombin Time (PT) measures how long blood takes to clot, evaluating the extrinsic/common coagulation pathway, with a normal PT of 12 seconds.
- INR (International Normalized Ratio) is a PT ratio calculation to compare values across facilities, where Normal INR is 1.0; values presented as PT/INR.
- Activated Partial Thromboplastin Time (aPTT) measures how long blood takes to clot, evaluating intrinsic/common coagulation pathways, with normal aPTT at ~40 seconds.
- Anti-Factor Xa activity measures the effect of anticoagulants indirectly, and is calibrated for each specific anticoagulant.
Hemostasis Disorders
- Inability to Make Clots: Decreased platelets (thrombocytopenia) or clotting factor deficiencies from severe liver impairment/hemophilia.
- Clotting Problem: Deep Vein Thrombosis (DVT), Pulmonary Embolism (PE), Myocardial Infarction, Ischemic Strokes.
Coagulation Disorders: Hemophilia
- It is a rare, inherited disorder where blood does not clot properly.
- It can result in spontaneous bleeding, severe bleeding after injury/surgery, or life-threatening internal bleeding.
- Hemophilia A (Classic) involves a lack/decrease in clotting factor VIII in 80% of cases.
- Treatment involves infusing the missing clotting factor.
Coagulation Disorders: Deep Vein Thrombosis (DVT)
- DVT: Thrombus in a major vein.
- Its Etiology: Venous stasis, endothelial damage, hypercoagulability of blood.
- Clinical Manifestations: Unilateral edema, warmth, redness, and tenderness.
- Treatment: Anticoagulation, prevent emboli formation/movement.
- Serious Complication: DVT leading to life-threatening Pulmonary Embolism (PE).
Pulmonary Embolism (PE) Clinical Manifestations
- Dyspnea
- Chest pain
- Sudden shortness of breath
- Tachycardia
- Tachypnea
- Hypotension
- Hemoptysis, cough
- Syncope
Overview of Hemostasis Modifiers
- Prevention of Clot Formation: Antiplatelets inhibit platelet action which decreases arterial thrombi (white clots), and Anticoagulants inhibit specific clotting factors to decrease arterial/venous thrombi (white/red clots).
- Removal of an Existing Clot: Thrombolytics (fibrinolytics) dissolve preexisting clots, and are fast-acting "clot busters" used in emergencies.
Rules of Thumb for Hemostasis Modifiers
- Medications prevent clot formation or dissolve existing clots by interfering with normal hemostasis processes.
- Contraindications: Avoid medications for patients with bleeding disorders or at risk of bleeding.
- Major Complication: Hemorrhage.
- Observe for bleeding gums, bruises, petechiae, epistaxis, tarry stools, hematuria, hematemesis, hematomas
- Increased heart rate, decreased blood pressure, abdominal pain
- Any multiple meds given with meds that increase bleeding (NSAIDs, steroids immunosuppressants, certain herbs, etc.), increases probability of hemorrhage.
- Medications altering hemostasis should be addressed before surgery/procedures.
- Any patient at risk of bleeding (disorder or taking medications) should be told to: avoid alcohol/OTC nonprescription medications (NSAIDs, aspirin), wear a medical alert bracelet, use a soft-bristled toothbrush/electric razor, and monitor clotting appropriately.
- Bleeding Herbs: Garlic Ginseng, Gingko biloba, Ginger Fish oil, St. John’s Wort, Dong Quai
Antiplatelet Medications
- These work on primary hemostasis to prevent platelet plug formation via Aspirin, ADP Receptor Antagonists, and GP IIb/IIIa Receptor Antagonists.
- It is used for acute treatment and/or prophylaxis of white clots for ischemic strokes, myocardial infarctions, peripheral atherosclerotic disease, cath lab procedures, and intermittent claudication.
Drug Class: Antiplatelet, Prototype: Aspirin
- Mechanism: Irreversibly inhibits cyclooxygenase 1 and 2 (COX-1, COX-2), decreasing platelet aggregation ("less sticky").
- Adverse: Hemorrhage, renal dysfunction, GI distress (use proton pump inhibitors or enteric-coated tablets), tinnitus.
- Contraindications: Hypersensitivity to NSAIDs, bleeding disorders/thrombocytopenia, viral infections in children/teenagers (<18 years), may be Reyes syndrome if fever is present.
- Route: Oral (immediate or enteric-coated).
- Clinical Considerations: Antipyretic, anti-inflammatory, analgesic properties, some platelet effects lasting 7 days. Administer immediate-release with food/water to minimize GI distress (do not crush enteric coated) and/or use DAPT = increased chances of bleeding.
Drug Class: Antiplatelet, Prototype: Clopidogrel
- The Mechanism is an irreversible blockade of platelet aggregation through ADP receptors.
- Adverse Effects: Hemorrhage, dyspepsia, BBW (reduced effect in CYP2C19 poor metabolizers), use CBC monitoring.
- Route: Oral.
- Clinical Considerations: Monitor CBC/signs of bleeding, where platelets gradually return to baseline at ~5-7 days after stopping.
Drug Class: Antiplatelet, Prototype: Eptifibatide
- The MOA is a reversible blockade of platelet GP IIb/IIIa receptors, via a glycoprotein inhibitor (most complete anti-platelet effect).
- Adverse Effects: Hemorrhage, hypotension and bradycardia.
- Clinical Considerations: Intravenous infusion, >90% inhibition attained within 10 mins, reversible effect, monitor vitals/CBC/bleeding.
Anticoagulant Medications
- These work by altering secondary hemostasis via decreasing the production of fibrin by interfering with the coagulation cascade.
- It is used for acute treatment and/or prophylaxis of red/white clots associated with Deep Vein Thrombosis (DVT), Pulmonary Embolism (PE), Atrial Fibrillation, Acute Angina, Myocardial Infarctions, and Ischemic Strokes.
Parenteral Anticoagulants vs Oral Anticoagulants
- Parenteral Drugs: Unfractionated Heparin (UFH) enhances antithrombin which inactivates thrombin (IIa) and other clotting factors, and Low Molecular Weight Heparin (LMWH) inactivates thrombin (IIa) and Factor Xa.
- Oral Drugs: Warfarin reduces Vitamin-K dependent clotting factors (II, VII, IX, X) and Dabigatran is a direct thrombin inhibitor (IIa), and “-Xabans” (Apixaban, Betrixaban, Edoxaban, Rivaroxaban) are factor Xa inhibitors.
Drug Class: Parenteral Anticoagulant, Prototype: Unfractionated Heparin (UFH)
- Mechanism: Enhances antithrombin, inactivating thrombin (IIa) and other clotting factors.
- Adverse Effects: Hemorrhage; Heparin-induced thrombocytopenia (HIT).
- Contraindications: Thrombocytopenia, bleeding, lumbar puncture, regional anesthesia and/or following eye/brain/spinal surgery, do not administer IM because it could cause hematoma.
- Route: Intravenous infusion (acute) and Subcutaneous injection (DVT prophylaxis).
Key Details for Heparin
- Not absorbed orally, use parenteral administration, and is safe to use in breast feeding.
- Administer bolus, then adjust dose based on lab results.
- Confirm dose; distribution binds variability in plasma levels.
- Monitor aPTT (60-80 seconds) or Anti-Factor Xa levels (0.3-0.7 unit/ml); CBC daily (platelet count held if <100,000/mm3), and for hypersensitivity, hemorrhage, and renal/hepatic function.
- Reversal agent: protamine sulfate by slow IV injection, used for active bleeding or aPTT >150.
Heparin Induced Thrombocytopenia (HIT)
- It is a potentially fatal immune-mediated disorder (1-3% when heparin is used for 4+ days) where antibodies are developed against heparin-platelet complexes, activating platelets and damaging endothelium.
- Platelet counts rapidly and Thrombosis occurs despite adequate anticoagulation. STOP Heparin and give something other than heparin.
Drug Class: Parenteral Anticoagulant, Prototype: LMWH (Enoxaparin)
- Inactivates Factor Xa and thrombin.
- Lower incidence of hemorrhage and HIT than UFH.
- Contraindicated for active major bleeding and history of HIT.
- Route: Subcutaneous or IV.
- Monitor vitals and CBC (hold if platelets
- Advantages over UFH: it's as effective/easier to use, and does not require coagulation monitoring. Fixed-doses are given based on weight and renal function and can be administered at home. Disadvantages: cannot be quickly reversed or "turned off". It is partially reversed with protamine.
Key steps for LMWH (Enoxaparin) administration
- Subcutaneous administration; insert needle and do not expel air bubble; do not rub or aspirate; and carefully rotate injection sites.
Oral Anticoagulants
- Warfarin acts by altering secondary hemostasis to decreases production of fibrin.
- The direct-acting alternatives (DOACs) act through direct thrombin (Factor IIa) inhibitors (Dabigatran) or direct Factor Xa inhibitors "-Xabans".
Drug Class: Oral Anticoagulant, Prototype: Warfarin
- Mechanism of Action: Antagonizes Vitamin K (inhibits Vitamin K epoxide reductase), which reduces synthesis of clotting factors synthesized in the liver.
- At therapeutic warfarin inhibits vitamin K reduction, decreasing clotting factors by 30-50%. Therapeutic levels are only achieved after 3-5 days.
- Adverse Effects: Hemorrhage, fetal hemorrhage/teratogenesis discoloration of urine.
- Liver and Renal disease
- Contraindication: Uncontrolled bleeding, Thrombocytopenia
- The dose must be monitored by testing the INR.
- There are many Drug and Food interactions.
- Route: Oral.
- Monitor INR regularly for proper dosing compliance
Bridging Warfarin Therapy
- Warfarin as a delayed onset which requires consistent monitoring.
- Bridging is required with a short acting anticoagulant until INR is at the appropriate level.
- Monitor INR during therapy for compliance and appropriate dosing
Warfarin Counseling Points
- Carry alert card or bracelet, keep track of INR goal.
- Monitor for bleeding.
- Follow-up care with all health providers for warfarin administration.
- Only take recommended OTC medications.
- Strictly follow the pharmacy and dietary guidelines.
- Do not use Alcohol.
DOAC Drugs
- Direct acting oral anticoagulants (DOACs) can eliminate Vitamin K inhibitors
- Monitor for Hemorrhage, watch for renal dysfunction
- There are some reversal agents
Warfarin vs DOAC drugs
- Warfarin requires frequent INR monitoring vs the DOAC options.
- DOAC has to be accounted with renal or hepatic dysfuntion.
- Vitamin K is very important vs very little food consideration for the drug
- DOAC causes fewer interactions vs that MANY drug interaction
Fibrinolytics
- Function as Agents that break up the clot
Drugs Class and prototype, Thrombolytic and Alteplase (tPa)
- Should only be used severely by Restoring Patency ( opening blockage) by Ischemic type issues like ACS, PE and Strokes.
- Dissolves clots that degrades the fibrin matrix
- Super cautious with risk because you can cause risk of serious bleeding
Contradictions with thromboembolisms
- Recent Strokes must be accounted for.
- Time dependent
- Vitals signs could be an emergency.
- Reverse using an aminocaproic acid
Clinical Pearls
- All anticoagulants come with risk of Hemorrhage.
- INR will come in handy
- Clopidogrel should only be administered to a CYPC19 metabolism.
- Warfarin is great to use is the is no time sensitivity issues
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.