Podcast
Questions and Answers
In the context of cardiac electrophysiology, which statement best describes the functional hierarchy between the sinoatrial (SA) node, atrioventricular (AV) node, and the bundle of His?
In the context of cardiac electrophysiology, which statement best describes the functional hierarchy between the sinoatrial (SA) node, atrioventricular (AV) node, and the bundle of His?
- The SA node, AV node and Bundle of His fire independently, only coordinating through extra-cardiac signalling mechanisms.
- The bundle of His modulates the rate established by the SA node, while the AV node provides backup pacing in cases of SA node failure.
- The AV node initiates the cardiac impulse, which is then refined by the SA node before being distributed by the bundle of His.
- The SA node serves as the primary pacemaker, the AV node introduces a critical delay, and the bundle of His facilitates rapid ventricular conduction. (correct)
Considering the biophysical properties of cardiac tissue, what accurately describes the propagation of the depolarization wave initiated by the SA node?
Considering the biophysical properties of cardiac tissue, what accurately describes the propagation of the depolarization wave initiated by the SA node?
- It propagates uniformly through the myocardium via gap junctions and is unaffected by tissue anisotropy.
- It is characterized by anisotropic conduction, with faster spread along the longitudinal axis of myocardial fibers due to enhanced gap junction coupling. (correct)
- It follows a path of least resistance, preferentially spreading through tissues with lower capacitance and high sodium channel density.
- It relies solely on the diffusion of ions across the extracellular space, making it highly susceptible to changes in extracellular fluid composition.
Under what circumstances would an artificial cardiac pacemaker set to VVI mode be most appropriate, considering both the patient's condition and the pacemaker's functional limitations?
Under what circumstances would an artificial cardiac pacemaker set to VVI mode be most appropriate, considering both the patient's condition and the pacemaker's functional limitations?
- For a patient with persistent atrial standstill and intact sinus node function, providing coordinated atrial and ventricular contractions.
- For a patient with paroxysmal atrial flutter and intermittent AV block, allowing for atrial tracking during normal sinus rhythm.
- For a patient with third-degree AV block and a history of paroxysmal supraventricular tachycardia, ensuring reliable ventricular pacing while minimizing the risk of retrograde conduction. (correct)
- For a patient with both atrial fibrillation and complete heart block, ensuring consistent ventricular pacing regardless of atrial activity.
When designing a rate-responsive pacemaker, which physiological parameter provides the most direct and reliable indication of exertion, facilitating appropriate adjustments in pacing rate?
When designing a rate-responsive pacemaker, which physiological parameter provides the most direct and reliable indication of exertion, facilitating appropriate adjustments in pacing rate?
Within the operational context of an atrial-synchronous pacemaker, what mechanisms prevent the occurrence of pacemaker-mediated tachycardia (PMT) due to retrograde VA conduction?
Within the operational context of an atrial-synchronous pacemaker, what mechanisms prevent the occurrence of pacemaker-mediated tachycardia (PMT) due to retrograde VA conduction?
In the event of a 'crosstalk' issue in a dual-chamber pacemaker, what immediate adjustments can one implement through external programming to mitigate ventricular inhibition due to atrial oversensing?
In the event of a 'crosstalk' issue in a dual-chamber pacemaker, what immediate adjustments can one implement through external programming to mitigate ventricular inhibition due to atrial oversensing?
When evaluating a patient with a newly implanted dual-chamber pacemaker who presents with symptoms of pacemaker syndrome (characterized by fatigue, dyspnea, and hypotension), what is the most appropriate initial diagnostic step?
When evaluating a patient with a newly implanted dual-chamber pacemaker who presents with symptoms of pacemaker syndrome (characterized by fatigue, dyspnea, and hypotension), what is the most appropriate initial diagnostic step?
What criteria serve as the most definitive indicators of lead perforation following implantation of a ventricular pacing lead, as distinguished from other complications like lead dislodgement or exit block?
What criteria serve as the most definitive indicators of lead perforation following implantation of a ventricular pacing lead, as distinguished from other complications like lead dislodgement or exit block?
In the management of a patient with a permanent pacemaker who requires Magnetic Resonance Imaging (MRI), what specific programming adjustments and safety protocols must be meticulously implemented to minimize the risk of device malfunction or patient injury?
In the management of a patient with a permanent pacemaker who requires Magnetic Resonance Imaging (MRI), what specific programming adjustments and safety protocols must be meticulously implemented to minimize the risk of device malfunction or patient injury?
When assessing a patient with a dual-chamber pacemaker who exhibits Wenckebach periodicity on the atrial channel during device interrogation, which intervention is most appropriate?
When assessing a patient with a dual-chamber pacemaker who exhibits Wenckebach periodicity on the atrial channel during device interrogation, which intervention is most appropriate?
When dealing with pacemaker-mediated tachycardia (PMT), what is the electrophysiological rationale behind prolonging the post-ventricular atrial refractory period (PVARP)?
When dealing with pacemaker-mediated tachycardia (PMT), what is the electrophysiological rationale behind prolonging the post-ventricular atrial refractory period (PVARP)?
A patient with a dual-chamber pacemaker implanted for sick sinus syndrome presents with 'pacemaker wenckebach.' Which adjustment would most effectively address this issue?
A patient with a dual-chamber pacemaker implanted for sick sinus syndrome presents with 'pacemaker wenckebach.' Which adjustment would most effectively address this issue?
What is the most critical consideration when programming a rate-adaptive pacemaker for a patient with chronotropic incompetence and frequent atrial fibrillation?
What is the most critical consideration when programming a rate-adaptive pacemaker for a patient with chronotropic incompetence and frequent atrial fibrillation?
Which of the following best describes the primary advantage of using a bipolar pacing lead over a unipolar lead in the context of a permanent pacemaker system?
Which of the following best describes the primary advantage of using a bipolar pacing lead over a unipolar lead in the context of a permanent pacemaker system?
In a patient with a dual-chamber pacemaker, what programming change would be most effective in preventing pacemaker-mediated tachycardia (PMT)?
In a patient with a dual-chamber pacemaker, what programming change would be most effective in preventing pacemaker-mediated tachycardia (PMT)?
Which sensor is best suited for rate-responsive pacing in a patient who is highly active and whose heart rate response to exercise is primarily driven by increased sympathetic tone?
Which sensor is best suited for rate-responsive pacing in a patient who is highly active and whose heart rate response to exercise is primarily driven by increased sympathetic tone?
In the context of pacemaker implantation, which strategy best minimizes the risk of subclavian crush syndrome?
In the context of pacemaker implantation, which strategy best minimizes the risk of subclavian crush syndrome?
What programming adjustment is best for a patient with a dual-chamber pacemaker who develops symptomatic ventricular ectopy primarily during periods of atrial pacing?
What programming adjustment is best for a patient with a dual-chamber pacemaker who develops symptomatic ventricular ectopy primarily during periods of atrial pacing?
In what scenario is His-bundle pacing most physiologically advantageous compared to right ventricular apical pacing?
In what scenario is His-bundle pacing most physiologically advantageous compared to right ventricular apical pacing?
What safety measure is the MOST critical when managing a patient with a non-MRI-conditional pacemaker that requires an essential MRI scan?
What safety measure is the MOST critical when managing a patient with a non-MRI-conditional pacemaker that requires an essential MRI scan?
Which strategy is most effective in preventing 'crosstalk' in a dual-chamber pacemaker immediately post-implantation without requiring lead revision?
Which strategy is most effective in preventing 'crosstalk' in a dual-chamber pacemaker immediately post-implantation without requiring lead revision?
A patient with a pacemaker presents with diaphragmatic stimulation. Which of the following lead-related strategies is most effective in resolving this issue without a complete lead extraction?
A patient with a pacemaker presents with diaphragmatic stimulation. Which of the following lead-related strategies is most effective in resolving this issue without a complete lead extraction?
What is the MOST crucial step to take immediately after noticing a rapid decline in a pacemaker's battery voltage during a routine device check?
What is the MOST crucial step to take immediately after noticing a rapid decline in a pacemaker's battery voltage during a routine device check?
Which factor is MOST important in determining the longevity of a pacemaker's battery?
Which factor is MOST important in determining the longevity of a pacemaker's battery?
What is the MOST likely cause of a sudden increase in pacing threshold observed during the first few weeks after permanent pacemaker implantation?
What is the MOST likely cause of a sudden increase in pacing threshold observed during the first few weeks after permanent pacemaker implantation?
What physiological characteristic will be MOST affected in a patient who has undergone AV node ablation and is now reliant on ventricular pacing at a fixed rate?
What physiological characteristic will be MOST affected in a patient who has undergone AV node ablation and is now reliant on ventricular pacing at a fixed rate?
What is the MOST likely sign observed on an ECG tracing that would suggest electrical lead perforation?
What is the MOST likely sign observed on an ECG tracing that would suggest electrical lead perforation?
In the context of leadless pacemakers, what is the primary advantage regarding infection risk compared to traditional transvenous pacemakers?
In the context of leadless pacemakers, what is the primary advantage regarding infection risk compared to traditional transvenous pacemakers?
Flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
The heart's natural pacemaker, initiating electrical signals for heart contraction. It is located at the top of the right atrium.
Atrioventricular (AV) node
Atrioventricular (AV) node
A node that receives and checks the electrical impulse from the SA node, delaying it slightly before sending it to the ventricles.
Bundle of His
Bundle of His
A track that carries the electrical impulse from the AV node down to the ventricles.
Bundle Branches
Bundle Branches
Signup and view all the flashcards
Electrocardiogram (ECG or EKG)
Electrocardiogram (ECG or EKG)
Signup and view all the flashcards
P Wave
P Wave
Signup and view all the flashcards
QRS Complex
QRS Complex
Signup and view all the flashcards
T Wave
T Wave
Signup and view all the flashcards
Artificial Cardiac Pacemaker
Artificial Cardiac Pacemaker
Signup and view all the flashcards
Pulse Generator
Pulse Generator
Signup and view all the flashcards
Leads
Leads
Signup and view all the flashcards
Battery system
Battery system
Signup and view all the flashcards
Programmable timing circuit
Programmable timing circuit
Signup and view all the flashcards
Asynchronous Pacemaker
Asynchronous Pacemaker
Signup and view all the flashcards
Power Supply (in Pacemaker)
Power Supply (in Pacemaker)
Signup and view all the flashcards
Oscillator
Oscillator
Signup and view all the flashcards
Output Circuit
Output Circuit
Signup and view all the flashcards
Lead Wires
Lead Wires
Signup and view all the flashcards
Asynchronous Pacemaker
Asynchronous Pacemaker
Signup and view all the flashcards
Demand Pacemaker
Demand Pacemaker
Signup and view all the flashcards
Feedback Circuit
Feedback Circuit
Signup and view all the flashcards
Timing Circuit
Timing Circuit
Signup and view all the flashcards
Atrial-Synchronous Pacemaker
Atrial-Synchronous Pacemaker
Signup and view all the flashcards
Atrial Electrode
Atrial Electrode
Signup and view all the flashcards
Rate-Responsive Pacing
Rate-Responsive Pacing
Signup and view all the flashcards
Sensor (in Rate-Responsive Pacing)
Sensor (in Rate-Responsive Pacing)
Signup and view all the flashcards
Accelerometer
Accelerometer
Signup and view all the flashcards
Study Notes
The Conduction System
- Electrical impulses from the myocardium cause the heart to beat (contract)
- The electrical signal starts in the sinoatrial (SA) node, which sits at the top of the right atrium
- The SA node is the heart's "natural pacemaker."
- When the natural pacemaker emits an electrical impulse, the atria contract
- The signal then goes through the atrioventricular (AV) node
- The AV node assesses the impulse and sends it down the bundle of His after a short transmission delay
- The bundle of His divides into right and left bundle branches, leading to the ventricles
- Heart rate varies depending on physical demands, stress, or hormonal factors, even though the SA node sends electrical impulses at a certain rate
- An impulse being blocked as it travels through the bundle branches results in bundle branch block
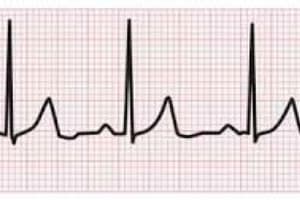
The Electrocardiogram
- During each cardiac cycle, the waves of depolarization moving through the heart produce electrical currents
- These currents spread through the body's interstitial fluids and up to the body's surface
- Recording electrodes on the skin's surface, on opposite sides of the heart, detect such electrical potentials
- Signals are filtered, amplified, and registered as a measure of the heart's electrical activity
- The resulting record from the procedure is an electrocardiogram (ECG or EKG)
- An ECG helps determine if any cardiac malfunction has an electrical cause
- A typical ECG has a P wave, a QRS complex, and a T wave
- Electrical currents from atrial muscle cells depolarizing before contraction result in the P wave
- The QRS complex follows as currents from the ventricles depolarize prior to their contraction
- After ventricular contraction, ventricle muscle cells repolarize and reversing electrical currents produce the T wave
- The T wave typically happens 0.25–0.35 s after ventricular depolarization
Cardiac Pacemaker Components
- An artificial cardiac pacemaker is an implanted device generating an excitatory wave at a heart site
- Pacemakers can be placed:
- At the SA node to replace a failing node and establish a normal sinus rhythm
- At the AV node if there is a malfunction
- Within one or both ventricles for excitation beyond a partial or total heart block
- A cardiac pacemaker consists of a pulse generator, leads, a battery system, and a programmable timing circuit
- Leads are wires connecting the pulse generator to cardiac tissues
- The insertion site of the device is in the upper chest, just under the skin
- The pacing lead, connecting to the pulse generator header, includes a flexible insulated wire
Cardiac Pacemaker Electrodes
- The tip that can be inserted through a vein into the heart delivers impulses from the pulse generator for stimulating the heart to beat
- Leads inserted via a vein into the heart feature tines or a screw end for threading into the cardiac muscle
Asynchronous Pacemaker
- The electric stimulus of an asynchronous pacemaker appears at a uniform rate, independent of the body
- It provides a fixed heart rate
- It was the first type of pacemaker, developed in the mid-twentieth century
- The power supply sends energy to the pacemaker circuit, and uses primary battery sources
- The oscillator sets the pulse rate for the pacemaker
- This controls the pulse output circuit, which provides the stimulating pulse to the heart
- The pulse is conducted along wires to the cardiac electrodes
- Every block is important in pacemaker construction, so each must be highly reliably
- Constant-voltage or constant-current amplitude pulses are the usual types of output stimuli
- Constant-voltage amplitude pulses have a range of 5 to 5.5 V and a duration of 500 to 600 μs
- Constant-current amplitude pulses range from 8 to 10 mA and last 1 to 1.2 ms
- Asynchronous pacemakers range from 70 to 90 beats/min
- Lead wires, must be mechanically strong and electrically conductive, since their distal ends must withstand heart beats
- Another must is to be well insulated
- Lead wires consist of interwound helical coils of spring-wire alloy molded in silicone rubber
- The helical coiling of the wire minimizes stress on it
- Multiple strands insure against failure following rupture of a single wire
Synchronous – Demand Pacemaker
- Often patients require cardiac pacing intermittently and can establish a normal cardiac rhythm between period of block
- The demand pacemaker consists of a timing circuit, an output circuit, electrodes, and a feedback loop
- The timing circuit runs at a fixed rate, usually 60 to 80 beats/min
- After each stimulus, the timing circuit resets, waits, and generates the next pulse.
- However if a natural beat occurs in the ventricle, the feedback circuit detects and amplifies the ECG signal
- This signal then resets the timing circuit to await before producing the next stimulus
- The timing circuit resets and the process repeats if the heart beats before a stimulus
- With a normal heart rate exceeding the timing circuit rate, the pacemaker is in standby, while the heart operates on its own
- If temporary heart block happens, the pacemaker takes over at the timing circuit's fixed rate.
Atrial-Synchronous Pacemaker
- The atrial-synchronous pacemaker has a circuit to replace a blocked conduction system
- The pacemaker detects electric signal (P wave of the ECG) by an atrial electrode and uses delays to activate a stimulus pulse
- Voltage v1 detected by the atrial electrodes is a pulse
- The atrial signal is amplified and passed through a gate to a monostable multivibrator, pulse v2 of 120 ms
- Another monostable multivibrator creates pulse duration of 500 ms
- V4 blocks signals from the atrial electrodes for a period of 500 ms
- This eliminates any artifact caused by ventricular contractions
- The falling edge of the 120 ms pulse triggers a monostable multivibrator of 2 ms
- Pulse v₂ acts as a delay, so ventricular stimulus happens 120 ms after atrial contraction
- Then v3 controls an output circuit applying stimulus to ventricular electrodes
Rate-Responsive Pacing
- Synchronous pacemakers can meet rate and cardiac output demands, but don't function for a physiologically intact individual
- The demands of stressful activities like exercise cannot be fully met
- A sensor is used to convert a physiological variable to an electric signal as input to the timing circuit
- This part of the pacemaker controls the heart rate based on a sensed physiological variable
- The sensor may be located within the pacemaker, or at some other point in the body
- Many variables can control rate responsive pacemakers
- An accelerometer is an example of sensor to control the pacing rate depending on patient activity
- The signal from the accelerometer is bandpass filtered and integrated for activity estimate
- A control algorithm for the timing circuit later determines pacing rate based on activity
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.