Podcast
Questions and Answers
What is heart failure primarily characterized by?
What is heart failure primarily characterized by?
- Increased heart rate at rest
- Inability to absorb oxygen from the lungs
- Inability to pump sufficient blood to meet the body's needs (correct)
- Dilation of the heart chambers without any dysfunction
Which type of heart failure is associated with impaired ventricular contraction?
Which type of heart failure is associated with impaired ventricular contraction?
- Uncomplicated heart failure
- Heart failure with preserved ejection fraction (HFpEF)
- Acute heart failure
- Heart failure with reduced ejection fraction (HFrEF) (correct)
What does an increased ventricular volume indicate in heart failure?
What does an increased ventricular volume indicate in heart failure?
- Normal ejection fraction
- Efficient heart function
- Improved oxygen delivery to the body
- Impaired ventricular contraction (correct)
Which compensatory mechanism is NOT typically involved in heart failure?
Which compensatory mechanism is NOT typically involved in heart failure?
Which of these is a characteristic feature of heart failure?
Which of these is a characteristic feature of heart failure?
What does heart failure with reduced ejection fraction (HFrEF) primarily indicate about ventricular function?
What does heart failure with reduced ejection fraction (HFrEF) primarily indicate about ventricular function?
Which of the following describes a condition where the heart cannot supply adequate oxygen to the body?
Which of the following describes a condition where the heart cannot supply adequate oxygen to the body?
Which compensatory mechanism is most likely to be activated during heart failure?
Which compensatory mechanism is most likely to be activated during heart failure?
Which of the following best explains the significance of ejection fraction in heart failure?
Which of the following best explains the significance of ejection fraction in heart failure?
Which type of dysfunction is primarily associated with heart failure that leads to chronic progressive symptoms?
Which type of dysfunction is primarily associated with heart failure that leads to chronic progressive symptoms?
What does the term 'ejection fraction' specifically relate to in heart failure?
What does the term 'ejection fraction' specifically relate to in heart failure?
Which of the following best describes systolic dysfunction in heart failure?
Which of the following best describes systolic dysfunction in heart failure?
Which of the following statements is true regarding diastolic dysfunction?
Which of the following statements is true regarding diastolic dysfunction?
What characterizes heart failure with reduced ejection fraction (HFrEF)?
What characterizes heart failure with reduced ejection fraction (HFrEF)?
Which compensatory mechanism might the body activate to manage heart failure?
Which compensatory mechanism might the body activate to manage heart failure?
What is the primary characteristic of heart failure with reduced ejection fraction (HFrEF)?
What is the primary characteristic of heart failure with reduced ejection fraction (HFrEF)?
Which statement accurately describes the condition of heart failure?
Which statement accurately describes the condition of heart failure?
What role do compensatory mechanisms play in heart failure?
What role do compensatory mechanisms play in heart failure?
Which of the following describes a potential consequence of diastolic dysfunction in heart failure?
Which of the following describes a potential consequence of diastolic dysfunction in heart failure?
Which statement is true regarding the basic mechanisms associated with heart failure?
Which statement is true regarding the basic mechanisms associated with heart failure?
Flashcards
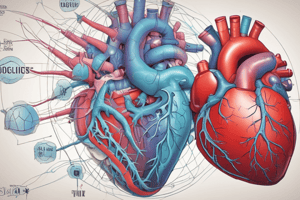
Heart Failure Definition
Heart Failure Definition
Chronic, progressive, incurable condition where the heart can't pump enough blood to supply the body with enough oxygen.
Systolic Dysfunction
Systolic Dysfunction
A heart problem where the heart's squeezing isn't strong enough to pump effectively.
Diastolic Dysfunction
Diastolic Dysfunction
A heart problem where the heart's relaxing isn't strong enough to fill with blood.
HFrEF definition
HFrEF definition
Signup and view all the flashcards
Ejection Fraction
Ejection Fraction
Signup and view all the flashcards
Heart Failure
Heart Failure
Signup and view all the flashcards
HFrEF
HFrEF
Signup and view all the flashcards
HFrEF (Heart Failure with Reduced Ejection Fraction)
HFrEF (Heart Failure with Reduced Ejection Fraction)
Signup and view all the flashcards
Study Notes
Drugs for Heart Failure
- Heart failure is a chronic, progressive, and incurable condition where the heart struggles to pump enough blood to provide adequate oxygen supply to the body.
- Key mechanisms include systolic and diastolic dysfunction, along with compensatory mechanisms.
Heart Failure: Systolic Dysfunction
- Systolic dysfunction (HFrEF) involves impaired ventricular contraction, leading to increased ventricular volumes and ejection fraction below 40%.
- Related causes include coronary artery disease, myocardial infarction, and dilated cardiomyopathy.
- Common clinical features include fatigue, dyspnea (shortness of breath), and reduced exercise tolerance.
Heart Failure: Diastolic Dysfunction
- Diastolic dysfunction (HFpEF) involves impaired ventricular relaxation and filling, leading to increased filling pressures.
- Ejection fraction is typically 50% or higher.
- Causes include hypertension, hypertrophic cardiomyopathy, and aging.
- Clinical features often include dyspnea, orthopnea (difficulty breathing when lying down), and fluid retention.
Congestive Heart Failure
- Congestive heart failure presents with signs and symptoms like raised jugular venous pressure (JVP), pulmonary edema, cardiomegaly, pleural effusions, hepatomegaly, ascites, and pitting edema in various locations.
NYHA Functional Classification
- The New York Heart Association (NYHA) classifies heart failure severity into four classes (I-IV) based on limitations in physical activity.
- Class I: No limitation in physical activity.
- Class II: Slight limitation in physical activity, but ordinary physical activity causes symptoms.
- Class III: Marked limitation in physical activity, but less than ordinary physical activity causes symptoms.
- Class IV: Severe limitation in physical activity, even ordinary physical activity causes symptoms.
AHA/ACC Stages
- AHA/ACC staging categorizes patients into four stages based on risk factors, symptoms, and structural heart disease regarding heart failure.
- Stage A: At-risk for heart failure, no current symptoms/signs and no structural/functional abnormalities or biomarkers.
- Stage B: Pre-heart failure, no current symptoms/signs but evidence of structural disease or increased filling pressures.
- Stage C: Symptomatic heart failure with current symptoms/signs, structural heart disease .
- Stage D: Advanced heart failure, severe symptoms that interfere with daily life and recurrent hospitalizations despite optimum treatment.
Heart Failure: Compensatory Mechanisms
- The body employs compensatory mechanisms to maintain cardiac output, including increased sympathetic nervous system activity, activation of the renin-angiotensin-aldosterone system (RAAS), and release of atrial natriuretic peptide (ANP).
Heart Failure: Pathophysiology
- The primary pathophysiological feature of heart failure is an inability of the heart to pump enough blood to meet the demands of the body, leading to fluid buildup in the lungs and other organs (congestion).
- This results from increased sympathetic nervous system activity, activation of the renin-angiotensin-aldosterone system (RAAS), and secretion of antidiuretic hormone (ADH).
Goal of Treatment in Heart Failure
- Symptom relief encompasses alleviating shortness of breath, reducing edema, and improving exercise tolerance .
- Disease progression prevention aids in slowing ventricular remodeling and worsening of heart function.
- Reduction of hospitalizations aims to minimize acute exacerbations and enhance outpatient management.
- Enhancement of quality of life and prolongation of survival are critical goals. Includes daily activity levels, enhanced well-being, reduced mortality, and optimized long-term outcomes .
Pre- and Afterload
- Preload refers to the volume of blood in the ventricles at the end of diastole. An increased preload can be caused by conditions like hypervolemia or regurgitation of cardiac valves.
- Afterload refers to the resistance left ventricle must overcome to circulate blood. Hypertension and vasoconstriction increase afterload.
Treatment of Heart Failure: Beta-Blockers
- Beta-blockers reduce heart rate and myocardial contractility, decreasing myocardial oxygen demand and increasing mortality.
- They are used for heart failure, hypertension, and post-myocardial infarction.
- Common side effects include bradycardia, hypotension, fatigue, and depression.
Treatment of Heart Failure: ACE Inhibitors (ACEIs)
- ACE inhibitors (ACEIs) block angiotensin-converting enzyme, reducing the formation of angiotensin II. This decreases preload and afterload, reducing ventricular remodeling.
- Indications include heart failure and hypertension
- Common side effects include cough, hyperkalemia, hypotension, and renal dysfunction.
Treatment of Heart Failure: Angiotensin II Receptor Blockers (ARBs)
- ARBs block angiotensin II receptors, preventing vasoconstriction and aldosterone release, reducing ventricular remodeling.
- Indications include heart failure, and hypertension.
- Common side effects of ARBs may include hyperkalemia, hypotension and renal dysfunction.
Treatment of Heart Failure: Angiotensin Receptor-Neprilysin Inhibitors (ARNIs)
- ARNIs inhibit neprilysin, increasing natriuretic peptides, leading to vasodilation, natriuresis, and diuresis.
- Indications include heart failure with reduced ejection faction.
- Common side effects include angioedema, hyperkalemia, hypotension, and renal dysfunction.
Treatment of Heart Failure: Sodium-Glucose Co-Transporter 2 (SGLT2i) Inhibitors
- SGLT2 inhibitors block sodium-glucose cotransporter 2, reducing glucose reabsorption, promoting natriuresis and osmotic diuresis.
- Benefits include reduced preload/afterload, improved glycemic control, body weight reduction, improved cardiac function, reduced cardiac workload, and reduced risk of hospitalization and cardiovascular death.
- Indications include heart failure with reduced or preserved ejection fraction, and type 2 diabetes with cardiovascular disease.
- Common side effects include genital mycotic infections, urinary tract infections, volume depletion, and hypotension. Potential risk for ketoacidosis in type 1 diabetics.
Treatment of Heart Failure: Mineralocorticoid Receptor Antagonists (MRAs)
- MRAs block mineralocorticoid receptors, reducing sodium and water retention, blood pressure and cardiac workload.
- They inhibit cardiac fibrosis and remodeling, improving symptoms, exercise tolerance and reduce risk of mortality and hospitalizations in heart failure.
- Indications include heart failure with reduced or preserved ejection fraction.
- Common side effects include hyperkalemia, gynecomastia (in some cases), and renal dysfunction.
Treatment of Heart Failure: Hydralazine/Isosorbide Dinitrate (BiDil)
- Hydralazine is a vasodilator primarily for arterioles, reducing afterload and cardiac output.
- Isosorbide dinitrate dilates veins, reducing preload and decreasing myocardial oxygen demand.
- Indications include heart failure in African American patients as an adjunct, heart failure in patients unable to tolerate ACE inhibitors, or ARBs.
- Side effects include headache, dizziness, hypotension, and gastrointestinal disturbances.
Treatment of Heart Failure: Diuretics
- Diuretics increase the excretion of sodium and water by kidneys, reducing blood volume, preload and afterload and alleviating fluid retention symptoms.
- Common side effects encompass electrolyte imbalances (hypokalemia and hyponatremia), dehydration, hypotension, renal dysfunction, and ototoxicity. Potentially increase the risk of dehydration, interact with other diuretics, and reduce efficacy of antihypertensive agents.
- Indications include relieving congestion, improving symptoms, preventing worsening HF in patients with HF and congestive symptoms.
Treatment of Heart Failure: Digoxin
- Digoxin inhibits sodium-potassium ATPase pump, increasing intracellular calcium, enhancing cardiac contractility, and reducing heart rate.
- Indications include heart failure with or without atrial fibrillation. Benefits include symptom improvements, increased exercise tolerance and reduced hospitalization rates for patients with heart failure.
- Potential side effects include digoxin toxicity, bradycardia, electrolyte imbalances, drug interactions with other medications, and cautions for patients with specific conditions.
Treatment of Heart Failure: Combined Therapy
- Combined therapies such as ACE inhibitors, ARBS, beta-blockers, and/or diuretics are often employed to optimize patient outcomes in heart failure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.