Podcast
Questions and Answers
What is the primary characteristic of heart failure with reduced ejection fraction (HFrEF)?
What is the primary characteristic of heart failure with reduced ejection fraction (HFrEF)?
- Increased ventricular contraction
- Normal ventricular sizes with high ejection fraction
- Impaired ventricular contraction with increased ventricular volumes (correct)
- Absent compensatory mechanisms
Which of the following statements best describes heart failure?
Which of the following statements best describes heart failure?
- It is characterized solely by diastolic dysfunction.
- It is a chronic and progressive condition resulting in inadequate blood pumping. (correct)
- It is a temporary condition that can be easily cured.
- It affects only elderly individuals.
What is one of the basic mechanisms involved in heart failure?
What is one of the basic mechanisms involved in heart failure?
- Systolic dysfunction (correct)
- Complete resolution of symptoms
- Isolation of the heart from systemic circulation
- Continuous increase in ejection fraction
Which of the following does NOT characterize heart failure?
Which of the following does NOT characterize heart failure?
In heart failure with reduced ejection fraction, how is the ejection fraction typically affected?
In heart failure with reduced ejection fraction, how is the ejection fraction typically affected?
What is a consequence of systolic dysfunction in heart failure?
What is a consequence of systolic dysfunction in heart failure?
In heart failure with reduced ejection fraction (HFrEF), what happens to the ventricular volumes?
In heart failure with reduced ejection fraction (HFrEF), what happens to the ventricular volumes?
Which of the following best describes the nature of heart failure?
Which of the following best describes the nature of heart failure?
Which mechanism contributes to the development of heart failure?
Which mechanism contributes to the development of heart failure?
What is the primary challenge associated with treating heart failure?
What is the primary challenge associated with treating heart failure?
What defines the condition of heart failure?
What defines the condition of heart failure?
What is the result of systolic dysfunction in heart failure?
What is the result of systolic dysfunction in heart failure?
Which mechanism is considered a compensatory response in heart failure?
Which mechanism is considered a compensatory response in heart failure?
Which statement is true regarding heart failure with reduced ejection fraction (HFrEF)?
Which statement is true regarding heart failure with reduced ejection fraction (HFrEF)?
What is primarily affected in patients with heart failure?
What is primarily affected in patients with heart failure?
Flashcards
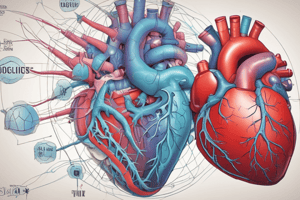
Heart Failure
Heart Failure
A chronic, progressive condition where the heart can't pump enough blood for normal body function.
Systolic Dysfunction
Systolic Dysfunction
Impaired heart contraction during pumping.
Heart Failure with Reduced Ejection Fraction (HFrEF)
Heart Failure with Reduced Ejection Fraction (HFrEF)
The heart's pumping is weak, leading to a reduced blood ejection.
Ejection Fraction
Ejection Fraction
Signup and view all the flashcards
Diastolic Dysfunction
Diastolic Dysfunction
Signup and view all the flashcards
HFrEF
HFrEF
Signup and view all the flashcards
What is heart failure?
What is heart failure?
Signup and view all the flashcards
What is systolic dysfunction?
What is systolic dysfunction?
Signup and view all the flashcards
What is diastolic dysfunction?
What is diastolic dysfunction?
Signup and view all the flashcards
What is ejection fraction?
What is ejection fraction?
Signup and view all the flashcards
What is HFrEF?
What is HFrEF?
Signup and view all the flashcards
Study Notes
Drugs for Heart Failure
- Heart failure is a chronic, progressive, and incurable condition where the heart struggles to pump enough blood to supply the body with sufficient oxygen.
- Basic mechanisms include systolic dysfunction, diastolic dysfunction, and compensatory mechanisms.
- Systolic dysfunction (HFrEF): Impaired ventricular contraction, with increased ventricular volumes, and ejection fraction below 40%.
- Causes include coronary artery disease, myocardial infarction, and dilated cardiomyopathy.
- Clinical features include fatigue, dyspnea (shortness of breath), and reduced exercise tolerance.
- Diastolic dysfunction (HFpEF): Impaired ventricular relaxation and filling, with increased filling pressures.
- Ejection fraction is 50% or greater
- Causes include hypertension, hypertrophic cardiomyopathy, and aging.
- Clinical features include dyspnea, orthopnea (difficulty breathing while lying down), and fluid retention.
- Compensatory mechanisms involve the heart trying to maintain cardiac output:
- Increased sympathetic nervous system activity
- Renin-angiotensin-aldosterone system (RAAS) activation
- Atrial natriuretic peptides
Congestive Heart Failure
- Signs and symptoms often associated with congestive heart failure include raised jugular venous pressure, pulmonary edema, cardiomegaly, pleural effusions, hepatomegaly, ascites, and peripheral pitting edema.
NYHA Functional Classification
- This system classifies heart failure severity by functional limitations. The classes range from no limitations (Class 1) to severe limitations with symptoms even at rest (Class 4).
AHA/ACC Stages
- Stages of heart failure risk:
- Stage A: At-risk for heart failure
- Stage B: Pre-heart failure
- Stage C: Symptomatic heart failure
- Stage D: Advanced heart failure
Treatment of Heart Failure-Beta Blockers
- Beta-blockers (e.g., Metoprolol, Carvedilol, Bisoprolol) are used to manage heart failure.
- They block beta-adrenergic receptors, lowering heart rate and myocardial contractility
- This can lower myocardial oxygen demand and reduce mortality.
- Common indications include heart failure, hypertension, and post-myocardial infarction.
- Potential adverse effects: bradycardia, hypotension, fatigue, depression.
- Drug interactions include calcium channel blockers, and antiarrhythmics.
Treatment of Heart Failure-ACE Inhibitors
- ACE inhibitors (e.g., Enalapril, Lisinopril) are indicated to manage heart failure by suppressing angiotensin II formation.
- Reduced preload and afterload, decreased ventricular remodeling.
- Indications include heart failure and hypertension.
- Potential adverse effects include: cough, hyperkalemia, hypotension, and renal dysfunction.
- NSAIDs can reduce their anti-hypertensive effects and increase the risk of renal dysfunction.
Treatment of Heart Failure-Angiotensin II Receptor Blockers (ARBs)
- Angiotensin II Receptor Blockers (ARBs) (e.g., Losartan, Valsartan) help by blocking angiotensin II receptors.
- Prevent vasoconstriction, aldosterone release.
- Indications include heart failure and hypertension.
- Potential adverse effects include hyperkalemia, hypotension, and renal dysfunction.
Treatment of Heart Failure-Angiotensin Receptor-Neprilysin Inhibitors (ARNIs)
- ARNIs (e.g., Sacubitril/Valsartan) are used to improve symptoms and reduce hospitalizations in heart failure.
- By inhibiting neprilysin, this increases natriuretic peptides and reduces cardiac workload
- Indications include heart failure with reduced ejection fraction (HFrEF)
- Potential adverse effects may include angioedema, hyperkalemia, hypotension, and renal dysfunction.
Treatment of Heart Failure-Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors
- SGLT2 Inhibitors (e.g., Dapagliflozin, Empagliflozin) are used to treat heart failure.
- Inhibit sodium-glucose transporter 2 (SGLT2) in the kidneys, enhancing glucose excretion.
- This reduces preload and afterload, improves glycemic control, and reduces body weight.
- Indications include heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF), type 2 diabetes with cardiovascular disease.
- Adverse effects include genital mycotic infections, urinary tract infections and potential hypoglycemia/dehydration.
Treatment of Heart Failure- Mineralocorticoid Receptor Antagonists (MRAs)
- Mineralocorticoid receptor antagonists (MRAs) (e.g., Spironolactone, Eplerenone) are used to manage heart failure. - Block mineralocorticoid receptors (in the kidney, heart and vasculature) to reduce sodium/water retention, decreasing blood pressure and cardiac workload. - Reduce mortality and hospitalizations and improve symptoms. - Indications include heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). - Adverse effects include hyperkalemia, gynecomastia (spironolactone), and renal dysfunction. - Interactions with ACEis, ARBs, potassium supplements, NSAIDs.
Treatment of Heart Failure-Hydralazine/Isosorbide Dinitrate (BiDil)
- Hydralazine and isosorbide dinitrate (BiDil) are used as an adjunct therapy in African American patients with heart failure.
- Hydralazine lowers afterload by dilating arterioles.
- Isosorbide dinitrate reduces preload by dilating veins.
- Improves symptoms, enhances quality of life, and reduces hospitalizations. Considered in patients unable to tolerate ACEi or ARBs.
Treatment of Heart Failure - Diuretics
- Diuretics (e.g., furosemide, hydrochlorothiazide, spironolactone, eplerenone) are often used to manage heart failure.
- Increase sodium and water excretion by the kidneys, leading to reduced blood volume.
- Results in decreased preload and afterload, reducing edema and pulmonary congestion
- Aids in managing fluid overload and symptoms of congestion.
- May include adverse effects such as electrolyte imbalances, dehydration, hypotension, and renal dysfunction, Drug interactions common, including potassium-sparing diuretics, NSAIDs, and antihypertensive drugs.
Treatment of Heart Failure - Digoxin
- Digoxin is a medication used to treat heart failure.
- Enhances cardiac contractility and reduces heart rate, decreasing workload.
- Indications include heart failure and atrial fibrillation.
- Potential adverse effects include digoxin toxicity, various arrhythmias, visual disturbances, and electrolyte imbalances (hypokalemia).
- Drug interactions include diuretics, amiodarone, verapamil and quinidine.
- Contraindicated in ventricular fibrillation, hypersensitivity or severe renal impairment.
Combined Therapy
- Combining different drugs may offer synergistic effects and improved outcomes compared to individual medications alone. Possible examples include ACE inhibitors with beta-blockers, and others (e.g. MRA, diuretics) depending on the clinical need
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.