Podcast
Questions and Answers
What is the mechanism of action of digoxin?
What is the mechanism of action of digoxin?
- Blocks both activated and inactivated L-type calcium channels
- Inhibits Ca2+ channels
- Activates inward rectifier K+ current
- Inhibits Na+/K+-ATPase (correct)
Which antiarrhythmic agent is the drug of choice for paroxysmal supraventricular tachycardia?
Which antiarrhythmic agent is the drug of choice for paroxysmal supraventricular tachycardia?
- Magnesium
- Verapamil
- Diltiazem
- Adenosine (correct)
What effect does verapamil have on the heart?
What effect does verapamil have on the heart?
- Increases blood pressure
- Increases cardiac contractility
- Slows SA node automaticity (correct)
- Enhances AV nodal conduction velocity
What is a possible toxicity associated with potassium administration?
What is a possible toxicity associated with potassium administration?
What clinical condition is magnesium commonly used to treat?
What clinical condition is magnesium commonly used to treat?
What is characterized by the absence of visible P waves and irregular R-R intervals?
What is characterized by the absence of visible P waves and irregular R-R intervals?
What condition results from the interaction of three specific criteria involving conduction and obstacles?
What condition results from the interaction of three specific criteria involving conduction and obstacles?
Which class of antiarrhythmic drugs primarily works by sodium channel blockade?
Which class of antiarrhythmic drugs primarily works by sodium channel blockade?
Which of the following is not a common trigger for arrhythmia?
Which of the following is not a common trigger for arrhythmia?
What is the primary effect of Procainamide?
What is the primary effect of Procainamide?
Which of the following is a side effect of Quinidine?
Which of the following is a side effect of Quinidine?
What type of tachycardia is defined as having a heart rate of 180 bpm or more?
What type of tachycardia is defined as having a heart rate of 180 bpm or more?
What is the pharmacological aim when treating arrhythmias?
What is the pharmacological aim when treating arrhythmias?
Which arrhythmia is characterized by a gradual change in the amplitude and twisting of the QRS complexes?
Which arrhythmia is characterized by a gradual change in the amplitude and twisting of the QRS complexes?
What is the significance of calcium channel blockade in antiarrhythmic therapy?
What is the significance of calcium channel blockade in antiarrhythmic therapy?
Which adverse effect is associated with disopyramide?
Which adverse effect is associated with disopyramide?
What is a characteristic of class IB antiarrhythmic agents?
What is a characteristic of class IB antiarrhythmic agents?
Which class of antiarrhythmic drugs is primarily used for atrial arrhythmias?
Which class of antiarrhythmic drugs is primarily used for atrial arrhythmias?
What is the mechanism of toxicity in Flecainide?
What is the mechanism of toxicity in Flecainide?
Which statement about Amiodarone is false?
Which statement about Amiodarone is false?
What effect does Dronedarone lack compared to Amiodarone?
What effect does Dronedarone lack compared to Amiodarone?
Which antiarrhythmic drug is indicated for the maintenance of normal sinus rhythm in atrial fibrillation?
Which antiarrhythmic drug is indicated for the maintenance of normal sinus rhythm in atrial fibrillation?
Which class of drugs does Verapamil belong to?
Which class of drugs does Verapamil belong to?
What is a common side effect of Sotalol?
What is a common side effect of Sotalol?
Which antiarrhythmic drug is effective in relieving chronic pain due to diabetic neuropathy?
Which antiarrhythmic drug is effective in relieving chronic pain due to diabetic neuropathy?
Flashcards are hidden until you start studying
Study Notes
Heart Conduction
- Heart conduction involves four steps
- Pacemaker impulse generation
- AV node impulse conduction
- AV bundle impulse conduction
- Purkinje fibers impulse conduction
Action Potential Phases
- 0 = Upstroke/Depolarization
- 1 = Early Fast Repolarization
- 2 = Plateau
- 3 = Repolarization
- 4 = Diastole
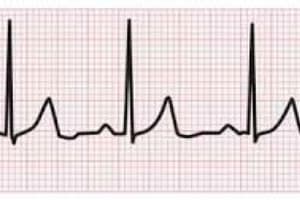
ECG
- The ECG reflects the depolarization and repolarization waves of the heart
Normal ECG
- P wave: generated by atrial depolarization
- QRS wave: generated by ventricular muscle depolarization
- T wave: generated by ventricular repolarization
Arrhythmia
- Also known as dysrrhythmia
- Describes irregular heartbeats
- Tachycardia: heart beats too fast
- Bradycardia: heart beats too slowly
- Premature contraction: heart beats too early
- Fibrillation: heart beats irregularly
Factors that trigger arrhythmia
- Ischemia
- Hypoxia
- Acidosis or Alkalosis
- Electrolyte Abnormalities
- Excessive catecholamine exposure
- Autonomic influences
- Drug toxicity (e.g., Digitalis)
- Overstretching of cardiac fibers
- Presence of scarred/diseased tissues
Causes of Arrhythmia
- Abnormal automaticity
- Disturbances in impulse conduction
Abnormal Automaticity
- Hypokalemia
- Beta-Adrenoceptor Stimulation
- Positive Chronotropic Drugs
- Fiber Stretch
- Acidosis
Disturbances in Impulse Conduction
- AV nodal block
- Bundle Branch Block
Reentry or "Circus Movement"
- Requires three conditions:
- Presence of obstacle (anatomic or physiologic)
- Unidirectional block at some point in the circuit; conduction must die out in one direction
- Conduction time around the circuit must be long enough that the retrograde impulse does not enter refractory tissue as it travels around the obstacle
Atrial Fibrillation (AFib)
- No visible P waves
- Irregular R-R intervals
Problems with AFib
- Anxiety
- Palpitations
- Risk of heart failure symptoms
- Risk of cardiac thrombus & embolism (stroke)
Supraventricular Tachycardia (SVT)
- Heart rate ≥ 180 bpm
Ventricular Tachycardia (VT)
- Monomorphic
- Polymorphic (e.g., Torsades de Pointes)
Basic Pharmacology of Antiarrhythmic Agents
Aim of Therapy
- Reduce ectopic pacemaker activity
- Modify conduction or refractoriness in reentry circuits to disable "circus movement"
Major Mechanisms of Action
- Sodium channel blockade
- Blockade of sympathetic autonomic effects in the heart
- Prolongation of the effective refractory period
- Calcium channel blockade
Specific Antiarrhythmic Agents
Class I: Sodium Channel Blockers
Class IA
- Prolongs the action potential
- Procainamide
- Quinidine
- Disopyramide
Procainamide
- Slows conduction velocity and pacemaker rate
- Prolongs action potential duration
- Dissociates from sodium channel with intermediate kinetics
- Direct depressant effects on SA and AV nodes
Clinical Applications:
- Most atrial and ventricular arrhythmias
- Second-line drug for most sustained ventricular arrhythmias associated with acute MI
Procainamide Toxicity
- Hypotension
- QT interval prolongation
- Induction of Torsade de Pointes
- Long-term therapy produces reversible lupus-related symptoms
Quinidine
- Similar to Procainamide but more toxic
Quinidine Toxicity
- Torsade de Pointes
- Cinchonism (headache, dizziness, and tinnitus)
Class IB
- Shortens action potential
- Lidocaine
- Phenytoin
- Tocainide
- Mexiletine
Lidocaine
- Xylocaine®
- Low incidence of toxicity and high effectiveness against arrhythmias during myocardial infarction
- Given intravenously
Clinical Applications
- Terminate ventricular tachycardia
- Prevent ventricular fibrillation after cardioversion
Lidocaine Toxicity
- Neurologic symptoms: Nystagmus, paresthesia, tremor, nausea, lightheadedness, hearing disturbances, slurred speech, convulsions
Mexiletine
- Mexitil®
- Orally active congener of Lidocaine
Clinical Applications
- Similar to Lidocaine
- Significant efficacy in relieving chronic pain (especially diabetic neuropathy and nerve injury)
Mexiletine Toxicity
- Neurologic: Tremor, blurred vision, lethargy
Class IC
- No effect on action potential
- Flecainide
- Encainide
- Moricizine
- Propafenone
Flecainide
- Tambocor®
- Potent blocker of sodium and potassium channels with slow unblocking kinetics
Clinical Applications
- Supraventricular Arrhythmias in patients with normal hearts
- DO NOT USE in ischemic conditions (Post-Myocardial Infarction)
Flecainide Toxicity
- Proarrhythmic
Propafenone
- Rhythmol®
- Primarily used for supraventricular arrhythmias
- Adverse Drug Reactions (ADRs): Metallic taste, constipation, arrhythmia exacerbation
Moricizine
- Phenothiazine derivative used for the treatment of ventricular arrhythmias
Class II: Beta-Adrenoceptor Blocking Agents
- Clinical Applications
- Atrial arrhythmias
- Prevention of recurrent infarction and sudden death
Class II Toxicity
-
Asthma
-
AV Blockade
-
Acute Heart Failure
-
Propanolol (Inderal®)
-
Esmolol (Brevibloc®) - a short-acting β-blocker, primarily used as an antiarrhythmic drug for intraoperative and other acute arrhythmias
-
Sotalol - non-selective β-blocking drug that prolongs the action potential
Class III: Drugs that Prolong Effective Refractory Period by Prolonging Action Potential: Potassium Channel Blockers
- Amiodarone
- Sotalol
- Bretylium
- Dofetilide
- Ibutilide
Amiodarone
- Cordarone
- Given IV or PO
Clinical Applications
- Serious ventricular arrhythmias
- Supraventricular arrhythmias
Amiodarone Toxicity
- Bradycardia
- Heart block in diseased hearts
- Peripheral vasodilation
- Pulmonary & hepatic toxicity
- Hyper- or hypothyroidism
- Photodermatitis
- Gray-blue discoloration in exposed areas of the skin
- Asymptomatic corneal microdeposits
- Blocks the peripheral conversion of thyroxine (T4) and triiodothyronine (T3)
- Potential source of large amounts of inorganic iodine
Dronedaron
- Structural analog of Amiodarone but lacks iodine atoms
- First antiarrhythmic drug shown to reduce mortality or hospitalization in patients with atrial fibrillation
Vernakalant
- Investigational multichannel blocker developed for the treatment of atrial fibrillation
Vernakalant Toxicity
- Dysgeusia (disturbance of taste)
- Sneezing
- Paresthesia
- Cough
- Hypotension
Sotalol
- Betapace®
- Has both β-adrenergic blocking (Class II) and action potential-prolonging actions (Class III)
Dofetilide
- Tikosyn
- Approved for the maintenance of normal sinus rhythm in patients with atrial fibrillation
- S/E: Torsades de Pointes
Ibutilide
- Corvert®
- IV is used for the acute conversion of atrial flutter and atrial fibrillation to normal sinus rhythm
- S/E: Torsades de Pointes, QT interval prolongation
Class IV: Calcium Channel Blocking Drugs
- Verapamil - prototype
- First introduced as antianginal agents
- Dihydropyridines do not share antiarrhythmic efficacy and may precipitate arrhythmias
Verapamil
- Isoptin®
- Blocks both activated and inactivated L-type calcium channels
Effects
- Slows SA node automaticity and AV nodal conduction velocity
- Decreases cardiac contractility
- Reduces blood pressure
Clinical Applications
- Supraventricular tachycardia
Diltiazem
- Cardizem®
- Similar efficacy to verapamil in the management of supraventricular arrhythmias, including rate control in atrial fibrillation
Miscellaneous Antiarrhythmic Agents
Digoxin
- MOA: Inhibits Na+/K+-ATPase
- Uses:
- 1-2 ng/mL (for atrial fibrillation or flutter)
- 0.5-0.8 ng/mL (for systolic heart failure)
Adenosine
- Adenocard®
- Nucleoside that occurs naturally throughout the body
- Half-life: < 10 seconds
Mechanism of Action
- Activation of inward rectifier K+ current and inhibition of Ca2+ current
Clinical Applications
- Currently, the drug of choice (DOC) for paroxysmal supraventricular tachycardia
Adenosine Toxicity
- Flushing
- Chest tightness
- Dizziness
Magnesium
- MOA: Poorly understood; interacts with Na+/K+ ATPase, K+, and Ca2+ channels
Clinical Applications
- Torsades de Pointes
- Digitalis-induced arrhythmias
Magnesium Toxicity
- Muscle weakness with overdose
Potassium
- MOA: Increases K+ permeability, K+ current
Effects of Increasing K+ Serum
- A resting potential depolarizing action
- A membrane potential stabilizing action
- Slows ectopic pacemakers
- Slows conduction velocity in the heart
Clinical Applications
- Digitalis-induced arrhythmias
- Arrhythmias associated with hypokalemia
Potassium Toxicity
- Reentrant arrhythmias
- Fibrillation
- Cardiac arrest with overdose
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.