Podcast
Questions and Answers
What is the most serious form of head injury?
What is the most serious form of head injury?
- Traumatic Brain Injury (TBI) (correct)
- Mild Concussion
- Skull Fracture
- Scalp Avulsion
A patient has sustained a primary head injury. Which of the following mechanisms could be the cause?
A patient has sustained a primary head injury. Which of the following mechanisms could be the cause?
- Cerebral edema causing increased intracranial pressure
- Hypotension leading to decreased cerebral perfusion
- Inadequate oxygen delivery to brain cells
- Contusions from impact (correct)
Which of the following assessment findings is MOST indicative of a basilar skull fracture?
Which of the following assessment findings is MOST indicative of a basilar skull fracture?
- Persistent localized pain
- Cerebrospinal fluid (CSF) leaking from the ears or nose (correct)
- Presence of a comminuted fracture on X-ray
- Depressed level of consciousness
A patient with a non-depressed skull fracture is being discharged. What key teaching point should the nurse emphasize to the patient and their family?
A patient with a non-depressed skull fracture is being discharged. What key teaching point should the nurse emphasize to the patient and their family?
Which of the following best describes a 'closed' or 'blunt' brain injury?
Which of the following best describes a 'closed' or 'blunt' brain injury?
A patient is diagnosed with a mild concussion. What characteristics are associated with this type of injury?
A patient is diagnosed with a mild concussion. What characteristics are associated with this type of injury?
What is the primary difference between a concussion and a contusion?
What is the primary difference between a concussion and a contusion?
Diffuse Axonal Injury (DAI) is associated with which of the following conditions?
Diffuse Axonal Injury (DAI) is associated with which of the following conditions?
Major symptoms of intracranial hemorrhage are frequently delayed until the hematoma is large enough to cause which of the following?
Major symptoms of intracranial hemorrhage are frequently delayed until the hematoma is large enough to cause which of the following?
A patient who has sustained a head injury exhibits an altered respiratory pattern, widened pulse pressure, and bradycardia. What condition is indicated by these signs?
A patient who has sustained a head injury exhibits an altered respiratory pattern, widened pulse pressure, and bradycardia. What condition is indicated by these signs?
When managing a patient with a head injury, why is it crucial to prevent secondary injury?
When managing a patient with a head injury, why is it crucial to prevent secondary injury?
A patient with a head injury has a GCS score of 8. What nursing intervention is a priority?
A patient with a head injury has a GCS score of 8. What nursing intervention is a priority?
What nursing intervention is important for preventing injury in a patient with a head injury?
What nursing intervention is important for preventing injury in a patient with a head injury?
What is an important nursing intervention for maintaining skin integrity in a patient with a head injury that has limited mobility?
What is an important nursing intervention for maintaining skin integrity in a patient with a head injury that has limited mobility?
Which of the following statements accurately reflects the epidemiology of spinal cord injuries (SCI)?
Which of the following statements accurately reflects the epidemiology of spinal cord injuries (SCI)?
Which anatomical locations are most vulnerable to spinal cord injuries due to their greater range of mobility?
Which anatomical locations are most vulnerable to spinal cord injuries due to their greater range of mobility?
An individual with an incomplete spinal cord lesion exhibits preservation of some motor and/or sensory function below the level of the injury. What additional manifestation is likely?
An individual with an incomplete spinal cord lesion exhibits preservation of some motor and/or sensory function below the level of the injury. What additional manifestation is likely?
A patient presents with acute pain in the neck after a motor vehicle accident and expresses fear that their neck is broken. What is the MOST appropriate immediate nursing action?
A patient presents with acute pain in the neck after a motor vehicle accident and expresses fear that their neck is broken. What is the MOST appropriate immediate nursing action?
What is the PRIMARY goal of medical management in the acute phase of a spinal cord injury?
What is the PRIMARY goal of medical management in the acute phase of a spinal cord injury?
Which of the following is a sign or symptom specific to neurogenic shock (as opposed to spinal shock) that requires close monitoring?
Which of the following is a sign or symptom specific to neurogenic shock (as opposed to spinal shock) that requires close monitoring?
Why is it important to avoid massaging the calves or thighs of a patient at risk for Deep Vein Thrombosis (DVT) after a spinal cord injury?
Why is it important to avoid massaging the calves or thighs of a patient at risk for Deep Vein Thrombosis (DVT) after a spinal cord injury?
A patient with a reported spinal cord injury is being cared for by the nursing staff. What is a key nursing intervention to promote adequate breathing and airway clearance?
A patient with a reported spinal cord injury is being cared for by the nursing staff. What is a key nursing intervention to promote adequate breathing and airway clearance?
The nurse is caring for a patient with a spinal cord injury who is at risk for sensory deprivation. Which of the following nursing interventions is MOST appropriate to address this risk?
The nurse is caring for a patient with a spinal cord injury who is at risk for sensory deprivation. Which of the following nursing interventions is MOST appropriate to address this risk?
Which of the following findings would suggest the patient is experiencing a secondary head injury?
Which of the following findings would suggest the patient is experiencing a secondary head injury?
In the context of head injuries, what does the term 'avulsion' refer to?
In the context of head injuries, what does the term 'avulsion' refer to?
After a head injury, the nurse monitors for signs of increased intracranial pressure (ICP). Which of the following vital sign changes would MOST strongly suggest rising ICP?
After a head injury, the nurse monitors for signs of increased intracranial pressure (ICP). Which of the following vital sign changes would MOST strongly suggest rising ICP?
A patient who sustained a head injury is undergoing a Computed Tomography (CT) scan. What is the PRIMARY reason CT scans are favored in the acute setting of head trauma?
A patient who sustained a head injury is undergoing a Computed Tomography (CT) scan. What is the PRIMARY reason CT scans are favored in the acute setting of head trauma?
A patient with a spinal cord injury is on bed rest. The nurse implements measures to prevent deep vein thrombosis (DVT). Which action would be CONTRAINDICATED?
A patient with a spinal cord injury is on bed rest. The nurse implements measures to prevent deep vein thrombosis (DVT). Which action would be CONTRAINDICATED?
The nurse is providing discharge teaching to a patient with a mild traumatic brain injury (TBI). Which instruction is MOST important for the nurse to include?
The nurse is providing discharge teaching to a patient with a mild traumatic brain injury (TBI). Which instruction is MOST important for the nurse to include?
In a patient with a head injury, which assessment finding is MOST indicative of increased intracranial pressure (ICP)?
In a patient with a head injury, which assessment finding is MOST indicative of increased intracranial pressure (ICP)?
A patient has a complete spinal cord lesion at the level of T10. Which of the following clinical manifestations would the nurse expect to find?
A patient has a complete spinal cord lesion at the level of T10. Which of the following clinical manifestations would the nurse expect to find?
What is the rationale for maintaining proper body alignment in a patient with a spinal cord injury? Select the BEST option.
What is the rationale for maintaining proper body alignment in a patient with a spinal cord injury? Select the BEST option.
When caring for a patient with a spinal cord injury, what is the priority nursing intervention to prevent complications related to skin integrity?
When caring for a patient with a spinal cord injury, what is the priority nursing intervention to prevent complications related to skin integrity?
Continuous electrocardiographic monitoring is especially important in patients with acute spinal cord injuries for which reason?
Continuous electrocardiographic monitoring is especially important in patients with acute spinal cord injuries for which reason?
A patient with which type of skull fracture generally does not require surgical treatment but requires close observation?
A patient with which type of skull fracture generally does not require surgical treatment but requires close observation?
For a patient who has sustained a spinal cord injury (SCI), which nursing intervention helps reduce the risk of DVT (deep vein thrombosis)?
For a patient who has sustained a spinal cord injury (SCI), which nursing intervention helps reduce the risk of DVT (deep vein thrombosis)?
Which assessment result suggests a complication specific to spinal cord injury rather than head injury?
Which assessment result suggests a complication specific to spinal cord injury rather than head injury?
Flashcards
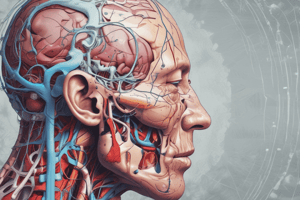
Head Injuries
Head Injuries
A broad classification that includes injury to the scalp, skull, or brain.
Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI)
The most serious form of head injury that may lead to conditions ranging from mild concussion to coma and death.
Primary Injury
Primary Injury
May include contusions, lacerations, and torn blood vessels due to impact, acceleration/deceleration, or foreign object penetration.
Secondary Injury
Secondary Injury
Evolves over hours and days after initial injury due to inadequate nutrient and oxygen delivery to cells.
Signup and view all the flashcards
Skull Fractures
Skull Fractures
A skull fracture is a break in the continuity of the skull caused by forceful trauma.
Signup and view all the flashcards
Pathophysiology of Head Injury
Pathophysiology of Head Injury
Brain suffers traumatic injury, swelling/bleeding increases volume, intracranial pressure increases, blood flow decreases, hypoxia/ischemia occur, brain herniates, and blood flow ceases.
Signup and view all the flashcards
Fractures of the Base of the Skull: Clinical Manifestations
Fractures of the Base of the Skull: Clinical Manifestations
Hemorrhage from nose/ears, blood under conjunctiva, bruising over mastoid (Battle's sign), CSF leaks from ears/nose.
Signup and view all the flashcards
Computed tomography (CT) scan
Computed tomography (CT) scan
Fast, accurate, and safe diagnostic procedure that shows the presence, nature, location, and extent of acute lesions.
Signup and view all the flashcards
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI)
Used to evaluate patients with head injury when a more accurate picture of the anatomic structure of the injury is warranted and when the patient is stable enough to undergo this longer diagnostic procedure.
Signup and view all the flashcards
Brain Injury Severity
Brain Injury Severity
Minor injury can cause significant brain damage due to obstructed blood flow and decreased tissue perfusion.
Signup and view all the flashcards
Closed (blunt) Brain Injury
Closed (blunt) Brain Injury
Head accelerates and then rapidly decelerates, brain tissue is damaged, no opening through skull and dura.
Signup and view all the flashcards
Open Brain Injury
Open Brain Injury
Object penetrates the skull, enters brain, damages soft brain tissue, trauma to head opens scalp, skull, dura to expose brain.
Signup and view all the flashcards
Concussion
Concussion
A temporary loss of neurologic function with no apparent structural damage.
Signup and view all the flashcards
Mild Concussion
Mild Concussion
Period of confusion, disorientation, memory lapse, loss of consciousness less than 30 minutes.
Signup and view all the flashcards
Classic Concussion
Classic Concussion
Injury results in loss of consciousness lasting less than 6 hours, and a degree of posttraumatic amnesia
Signup and view all the flashcards
Contusion
Contusion
A moderate to severe head injury where the brain is bruised and damaged in a selected area of the brain.
Signup and view all the flashcards
Diffuse Axonal Injury (DAI)
Diffuse Axonal Injury (DAI)
DAI is associated with prolonged traumatic coma; it is more serious and is associated with a poorer prognosis than a focal lesion or ischemia.
Signup and view all the flashcards
Intracranial Hemorrhage
Intracranial Hemorrhage
Symptoms are frequently delayed until the hematoma is large enough to cause distortion of the brain and increased ICP.
Signup and view all the flashcards
Epidural Hematoma
Epidural Hematoma
Collection of blood in the epidural space between the skull and the dura mater.
Signup and view all the flashcards
Subdural Hematoma
Subdural Hematoma
Collection of blood between the dura and the brain, a space normally occupied by a thin cushion of fluid.
Signup and view all the flashcards
Intracerebral Hemorrhage and Hematoma
Intracerebral Hemorrhage and Hematoma
Bleeding into the substance of the brain/within the brain.
Signup and view all the flashcards
Clinical Manifestations of Brain Injury
Clinical Manifestations of Brain Injury
Altered consciousness, confusion, pupillary abnormalities, altered gag reflex, sensory dysfunction, headache, seizures, changes in vital signs, vision/hearing impairment
Signup and view all the flashcards
Head Injury Presumption
Head Injury Presumption
Any patient with a head injury needs to be presumed to have a cervical spine injury until proven otherwise.
Signup and view all the flashcards
Managing Head Injury
Managing Head Injury
Transportation on a board with head/neck aligned, cervical collar applied, prevention of secondary injury and treatment of increased intracranial pressure.
Signup and view all the flashcards
Potential Problems/Complications
Potential Problems/Complications
Decreased cerebral perfusion, cerebral edema and herniation, impaired oxygenation and ventilation, and risk of posttraumatic seizures.
Signup and view all the flashcards
Nursing Interventions for Head Injury
Nursing Interventions for Head Injury
Monitor neurologic function, vital signs, motor function, and the size and equality of the pupils.
Signup and view all the flashcards
Supporting Head Injury Recovery
Supporting Head Injury Recovery
Elevate head of bed, monitor fluid/electrolyte balance, promote nutrition, pad side rails, avoid opioids, and minimize environmental stimuli
Signup and view all the flashcards
Spinal Cord Injury (SCI)
Spinal Cord Injury (SCI)
An injury that primarily impacts young adult males(age 16 to 30) and is often caused by risk factors, such as drug abuse.
Signup and view all the flashcards
Pathophysiology of SCI
Pathophysiology of SCI
Damage ranges from concussion, contusion, laceration to complete transection; vertebrae involved are C5-C7 and L1.
Signup and view all the flashcards
Clinical Manifestations of SCI
Clinical Manifestations of SCI
Acute pain, fear of broken neck/back, incomplete SCI lesions, loss of bowel and bladder control.
Signup and view all the flashcards
SCI Assessment Tests
SCI Assessment Tests
X-rays, CT scans, MRI, and electrocardiographic monitoring.
Signup and view all the flashcards
SCI Emergency Management
SCI Emergency Management
Considered for any patients involved in motor vehicle crash, or diving or contact sports injuries.
Signup and view all the flashcards
Acute Phase Medical Management
Acute Phase Medical Management
Prevent secondary injury, observe for symptoms, and pharmacological respiratory therapy.
Signup and view all the flashcards
Surgical Management Indications
Surgical Management Indications
Compression of the cord is evident, results in fragmention, involves a lesion.
Signup and view all the flashcards
Management of Acute Complications
Management of Acute Complications
Spinal and neurogenic shock. Deep Vein thrombosis is a big concern. Watch out for: Respiratory failure, Pneumonia, Autonomic dysreflexia, Pressure ulcers
Signup and view all the flashcards
Nursing Interventions
Nursing Interventions
Monitor O2, maintain body alignment, promote sense alterations, maintain skin integrity and promote urination
Signup and view all the flashcardsStudy Notes
- Lesson Title: Head Injuries, Brain Injury, and Spinal Cord Injury
Head Injuries
- Head injuries are broad classifications that include injury to the scalp, skull, or brain.
- Head injuries range from mild concussion to death, with the most serious form known as a traumatic brain injury (TBI).
- Common causes of TBIs include falls (28%), motor vehicle crashes (20%), being struck by objects (19%), and assaults (11%).
- The highest-risk group for TBI are individuals 15-19 years of age.
- Males are twice as likely as females to sustain a TBI.
Forms of Head Injury
- Primary injury involves contusions, lacerations, and torn blood vessels due to impact, acceleration/deceleration, or foreign object penetration.
- Secondary injury evolves over hours and days after the initial injury due to inadequate nutrient and oxygen delivery to cells.
Scalp Injury
- A large avulsion (tearing away) of the scalp may be life-threatening.
Skull Fractures
- Skull fractures are a break in the continuity caused by trauma.
- Skull fractures may occur with or without brain damage.
- Skull fractures are classified: simple, comminuted, depressed, or basilar.
Head Injury Pathophysiology
- The brain suffers traumatic injury.
- Brain swelling or bleeding increases intracranial volume (ICV).
- The rigid cranium doesn't allow for expansion, which increases intracranial pressure (ICP).
- Pressure on blood vessels slows blood flow to the brain.
- Cerebral hypoxia and ischemia occur.
- Intracranial pressure rises, potentially causing brain herniation.
- Cerebral blood flow ceases.
Head Injury Clinical Manifestations
- Persistent, localized pain.
- Fractures of the skull base cause hemorrhage from the nose, pharynx, or ears; blood under the conjunctiva; and ecchymosis over the mastoid (Battle's sign).
- Basilar skull fractures result in cerebrospinal fluid (CSF) escaping from the ears (CSF otorrhea) and nose (CSF rhinorrhea).
Head Injury Assessment and Diagnostics
- Physical and neurological examinations detect obvious brain injuries.
- X-rays confirm the presence and extent of skull fracture.
- Computed tomography (CT) scans show acute lesions; it assists in managing head injuries by disclosing edema, contusion, hematoma, hemorrhage, and late changes such as infarction or hydrocephalus..
- Magnetic resonance imaging (MRI) evaluates patients with head injuries when a more accurate picture of the injury's anatomic nature is needed and the patient is stable enough for the longer procedure.
- Cerebral angiography identifies supratentorial, extracerebral, and intracerebral hematomas and cerebral contusions.
Head Injury Medical Management
- Nondepressed skull fractures generally do not need surgery, but need close observation.
- Patients with no underlying brain injury may return home.
- Depressed skull fractures require surgery with elevation of the skull and debridement, usually within 24 hours of injury.
Brain Injury
- Minor brain injury can lead to significant damage due to obstructed blood flow and decreased tissue perfusion.
- Closed (blunt) brain injury is where the head accelerates, then rapidly decelerates or collides with another object. Brain tissue is damaged, but there is no opening through the skull and dura.
- Open brain injury occurs when an object penetrates the skull, enters the brain, and damages soft brain tissue is damaged or when severe blunt trauma opens the scalp, skull, and dura to expose the brain.
Concussion
- Concussion is a temporary loss of neurologic function with no apparent structural damage.
- Concussions are referred to as a mild TBI, and may or may not produce a brief loss of consciousness.
- Brain injury is commonly caused by blunt trauma from an acceleration-deceleration force, direct blow, or blast injury.
- Frontal lobe injuries may cause bizarre/irrational behavior, while temporal lobe injuries cause temporary amnesia or disorientation.
Types of Concussion
- Mild concussion can lead to a period of transient confusion, disorientation, or impaired consciousness.
- Memory lapse is common at the time of injury and loss of consciousness lasts less than 30 minutes.
- Classic concussion results in a loss of consciousness that lasts for less than 6 hours.
- Loss of consciousness is always accompanied by some degree of posttraumatic amnesia.
- Diagnostic studies show no structural injury with concussion, but the duration of unconsciousness indicates its severity.
Contusion
- Contusion is a moderate to severe head injury, where the brain is bruised and damaged because of severe acceleration-deceleration force or blunt trauma.
- Contusions can be identified by loss of consciousness associated with stupor and confusion.
Diffuse Axonal Injury (DAI)
- DAI results from widespread shearing and rotational forces that produce damage throughout the brain.
- Axons of the cerebral hemispheres, corpus callosum, and brain stem may be affected.
- The injured area may be diffuse, with no identifiable focal lesion.
- DAI is associated with prolonged traumatic coma; it is more serious and associated with a poorer prognosis than a focal lesion or ischemia.
Intracranial Hemorrhage
- Symptoms are frequently delayed until hematomas are large enough to cause distortion of the brain and increased ICP.
- Epidural hematoma is a collection of blood in the epidural space between the skull and dural mater.
- Subdural hematoma is a collection of blood between the dura and the brain, a space normally occupied by a thin cushion of fluid.
- Intracerebral hemorrhage and hematoma is the bleeding into the substance of the brain/within the brain.
Brain Injury Clinical Manifestations
- Altered level of consciousness
- Confusion
- Pupillary abnormalities (changes in shape, size, and response to light)
- Altered or absent gag reflex
- Absent corneal reflex
- Sudden onset of neurologic deficits
- Changes in vital signs (altered respiratory pattern, widened pulse pressure, bradycardia, tachycardia, hypothermia, or hyperthermia)
- Vision and hearing impairment
- Sensory dysfunction
- Headache
- Seizures
Brain Injury Assessment and Diagnostic Findings
- Physical and neurologic examinations
- CT and MRI scans for evaluating the brain structure
Brain Injury Management
- Any patient with a head injury is presumed to have a cervical spine injury until proven otherwise.
- Patients should be transported on a board with their head and neck aligned with the axis of the body.
- Apply a cervical collar.
- Prevent secondary injury.
- Treat increased intracranial pressure.
- Provide supportive measures.
- Provide end-of-life care to patients with brain death.
Brain Injury Collaborative Problems and Potential Complications
- Decreased cerebral perfusion
- Cerebral edema and herniation
- Impaired oxygenation and ventilation
- Impaired fluid, electrolyte, and nutritional balance
- Risk of posttraumatic seizures
Brain Injury Nursing Interventions
- Monitor neurologic function, including Level of Consciousness (LOC) and Vital Signs (Signs of increasing ICP: Cushing's triad).
- Glascow Coma Scale (GCS) is used to assess LOC at regular intervals.
- Motor function assessment.
- Pupillary Assessment (size and equality of the pupils).
- Maintain airway with elevation of head of the bead; suction.
- Monitor fluid and electrolyte balance.
- Promote adequate nutrition.
- Increase calorie consumption.
- Pad siderails to prevent injuries, avoid opioids, and reduce environmental stimuli.
- Maintain body temperature (give Acetaminophen, use cooling blankets, and culture for potential sites of infection).
- Maintain skin integrity, Turning and positioning; check skin integrity.
- Improve Cognitive Function.
- Monitor and Manage Potential Complications.
- Promote Home and Community-Based Care.
Spinal Cord Injury
- Spinal cord injury (SCI) is primarily an injury of young adult males, with 50% of those injured between 16 and 30 years of age.
- Predominant risk factors include young age, male gender, alcohol and drug use.
- Most spinal cord injuries (~80%) occur in men.
- Major causes of death due to SCI are pneumonia, pulmonary emboli (PE), and septicemia.
Spinal Cord Injury Pathophysiology
- Spinal cord injury ranges from transient concussion to contusion, laceration, and compression of spinal cord substance.
- Complete transection (severing) of the spinal cord results in paralysis below the injury level.
- The 5th, 6th, and 7th cervical vertebrae (C5 to C7), the 12th thoracic vertebra (T12), and the 1st lumbar vertebra (L1) are most commonly involved, due to a greater range of motion within the vertebral column.
- Primary injuries and secondary injuries are two categories.
Spinal Cord Injury Clinical Manifestations
- Acute pain in the back or neck, which may radiate along the involved nerve.
- Fear that the neck or back is broken.
- Incomplete spinal cord lesions affects sensory or motor fibers, or both, are preserved below the lesion.
- This consists of (a) total sensory and motor paralysis, (b) loss of bladder and bowel control (usually with urinary retention and bladder distention), and (c) loss of sweating and vasomotor tone, and marked reduction of blood pressure.
- A complete spinal cord lesion results in total loss of sensation and voluntary muscle control below the lesion, which results in paraplegia or tetraplegia.
Spinal Cord Injury Assessment and Diagnostic Tests
- X-rays (lateral cervical spine x-rays) and CT scan.
- MRI (myelogram if MRI is contraindicated).
- Continuous electrocardiographic monitoring is a diagnostic tool due to bradycardia (slow heart rate) and asystole (cardiac standstill).
Spinal Cord Injury Emergency Management
- All patients with a motor vehicle crash, a diving/contact sports injury, a fall, or any direct trauma the head and neck must be considered to have SCI.
- Rapid assessment, immobilization, stabilization of life-threatening injuries, and transportation must occur.
- If SCI and bone instability have been ruled out, the patient may be moved to a conventional bed or the collar may be removed.
Spinal Cord Injury Medical Management - Acute Phase
- Management goals are to prevent secondary injury, observe progressive neurologic deficits symptoms, and prevent complications. Involves:
- Pharmacologic intervention with high-dose IV corticosteroids.
- Respiratory therapy.
- Skeletal fracture reduction and traction.
Spinal Cord Injury Surgical Management Indicatons
- Compression of the cord.
- A fragmented or unstable vertebral body.
- A wound that penetrates the cord.
- Bony fragments in the spinal canal.
- A patient's deteriorating neurologic status.
Management of Acute Complications of Spinal Cord Injury
- Spinal and neurogenic shock.
- Spinal shock: use intestinal decompression through the insertion of a nasogastric tube.
- Neurogenic shock: close observation is needed for early detection as shown by abrupt onset of fever.
- Deep Vein Thrombosis (DVT) prevention with low-dose anticoagulation therapy and use of anti-embolism stockings/pneumatic compression devices.
- Calves or thighs should never be massaged.
- Other complications: respiratory failure, pneumonia, autonomic dysreflexia, pressure ulcers, and infections.
Spinal Cord Injury Nursing Interventions
- Promote adequate breathing & airway clearance with oxygenation monitoring; and suctioning of secretions.
- Improve mobility by maintaining proper body alignment and ROM exercises.
- Promote adaptation to sensory and perceptual alterations through the stimulation of senses.
- Maintain skin integrity.
- Maintain urinary elimination.
- Improve bowel function.
- Provide comfort measures.
- Monitor and manage potential complications (thrombophlebitis, orthostatic hypotension, and autonomic dysreflexia)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.