Podcast
Questions and Answers
What is the initial phase of haemostasis that occurs at the site of vascular endothelial damage?
What is the initial phase of haemostasis that occurs at the site of vascular endothelial damage?
- Coagulation cascade
- Platelet adhesion (correct)
- Clot retraction
- Fibrinolysis
Which component plays a key role in the secondary haemostasis pathway?
Which component plays a key role in the secondary haemostasis pathway?
- Tissue factor (correct)
- Prothrombin
- Fibrinogen
- Platelet factor 3
Which factor is NOT a part of the clotting cascade?
Which factor is NOT a part of the clotting cascade?
- Calcium ions
- Factor VIII
- Factor XIII
- Thrombin inhibitor (correct)
Which mechanism is used in dentistry to manage bleeding during procedures?
Which mechanism is used in dentistry to manage bleeding during procedures?
What is a potential consequence of significant blood loss during dental procedures?
What is a potential consequence of significant blood loss during dental procedures?
What is the primary function of adenosine diphosphate (ADP) in the process of haemostasis?
What is the primary function of adenosine diphosphate (ADP) in the process of haemostasis?
During which phase of haemostasis does the fibrin mesh formation occur?
During which phase of haemostasis does the fibrin mesh formation occur?
What is the main initiator of the extrinsic pathway in the clotting cascade?
What is the main initiator of the extrinsic pathway in the clotting cascade?
What condition might lead to prolonged bleeding time due to disruption in primary haemostasis?
What condition might lead to prolonged bleeding time due to disruption in primary haemostasis?
Which of the following accurately describes the normal range for Prothrombin Time (PT)?
Which of the following accurately describes the normal range for Prothrombin Time (PT)?
What is the first stage of haemostasis?
What is the first stage of haemostasis?
Which component is primarily responsible for stabilizing the platelet plug during primary haemostasis?
Which component is primarily responsible for stabilizing the platelet plug during primary haemostasis?
Which symptom is NOT associated with severe blood loss?
Which symptom is NOT associated with severe blood loss?
During primary haemostasis, which substances are released by platelets to facilitate vasoconstriction?
During primary haemostasis, which substances are released by platelets to facilitate vasoconstriction?
What is the primary function of secondary haemostasis?
What is the primary function of secondary haemostasis?
What is a potential consequence of moderate blood loss?
What is a potential consequence of moderate blood loss?
What defines the role of fibrin in coagulation during secondary haemostasis?
What defines the role of fibrin in coagulation during secondary haemostasis?
Which statement accurately describes homeostatic response to blood loss?
Which statement accurately describes homeostatic response to blood loss?
What occurs during the vasoconstriction phase of haemostasis?
What occurs during the vasoconstriction phase of haemostasis?
Which factor initiates the extrinsic pathway in the clotting cascade?
Which factor initiates the extrinsic pathway in the clotting cascade?
What role does thrombin play in the clotting cascade?
What role does thrombin play in the clotting cascade?
What is the main purpose of the platelet plug formation during primary haemostasis?
What is the main purpose of the platelet plug formation during primary haemostasis?
Which statement is true about clot retraction?
Which statement is true about clot retraction?
What is the significance of understanding clotting disorders for dental hygienists?
What is the significance of understanding clotting disorders for dental hygienists?
What is fibrinolysis?
What is fibrinolysis?
What generally happens to typical bleeding after dental procedures?
What generally happens to typical bleeding after dental procedures?
What role does TAFI play in the process of coagulation?
What role does TAFI play in the process of coagulation?
Which anticoagulant specifically inhibits Vitamin K-dependent clotting factors?
Which anticoagulant specifically inhibits Vitamin K-dependent clotting factors?
What is the typical bleeding time for primary haemostasis?
What is the typical bleeding time for primary haemostasis?
What can be a consequence of enhanced fibrinolysis?
What can be a consequence of enhanced fibrinolysis?
Which medical condition is characterized by deficiencies in clotting factors?
Which medical condition is characterized by deficiencies in clotting factors?
How does Rivaroxaban function in the clotting cascade?
How does Rivaroxaban function in the clotting cascade?
What is a major symptom associated with severe blood loss?
What is a major symptom associated with severe blood loss?
Which pathway is triggered by tissue damage and measured by Prothrombin Time (PT)?
Which pathway is triggered by tissue damage and measured by Prothrombin Time (PT)?
What can cause prolonged bleeding time?
What can cause prolonged bleeding time?
Which dental management technique aids in blood clotting when pressure and sutures are insufficient?
Which dental management technique aids in blood clotting when pressure and sutures are insufficient?
Activated partial thromboplastin time test is used to measure the intrinsic clotting pathway
Activated partial thromboplastin time test is used to measure the intrinsic clotting pathway
What are common anticoagulants that affect haemostasis
What are common anticoagulants that affect haemostasis
The extrinsic pathway is triggered by tissue factor (tissue factor III) released by damaged endoothelial cells which activates VII
The extrinsic pathway is triggered by tissue factor (tissue factor III) released by damaged endoothelial cells which activates VII
Clotting factors are produced mainly in the liver, they help convert fibrinogen to fibrin, stabilising the clot
Clotting factors are produced mainly in the liver, they help convert fibrinogen to fibrin, stabilising the clot
Fibrinolysis is the process where plasmid breaks down fibrin, dissolving the clot
Fibrinolysis is the process where plasmid breaks down fibrin, dissolving the clot
Activated partial thromboplastin (APTT) time is the test used too measure intrinsic pathway
Activated partial thromboplastin (APTT) time is the test used too measure intrinsic pathway
Prothrombin time is the test used for extrinsic pathway
Prothrombin time is the test used for extrinsic pathway
Extrinsic pathway is triggered by blood contact with collagen
Extrinsic pathway is triggered by blood contact with collagen
Extrinsic pathway is triggered by tissue damage
Extrinsic pathway is triggered by tissue damage
Intrinsic pathway is triggered by blood contact with collage
Intrinsic pathway is triggered by blood contact with collage
The intrinsic clotting pathway is activated by blood coming into contacts with collagen fibers in the broken wall of a blood vessel
The intrinsic clotting pathway is activated by blood coming into contacts with collagen fibers in the broken wall of a blood vessel
Flashcards
What is Haemostasis?
What is Haemostasis?
The process of stopping bleeding involving vasoconstriction, platelet plug formation, and coagulation.
Vasoconstriction
Vasoconstriction
Blood vessels constrict to reduce blood flow, and platelets release substances to promote further constriction.
Platelet Plug Formation
Platelet Plug Formation
Platelets adhere to the damaged vessel wall, forming a plug stabilized by von Willebrand factor.
Coagulation
Coagulation
Signup and view all the flashcards
Extrinsic Pathway
Extrinsic Pathway
Signup and view all the flashcards
Intrinsic Pathway
Intrinsic Pathway
Signup and view all the flashcards
Dental Procedures & Bleeding
Dental Procedures & Bleeding
Signup and view all the flashcards
Bleeding Time
Bleeding Time
Signup and view all the flashcards
Fibrin Formation
Fibrin Formation
Signup and view all the flashcards
Fibrin Mesh
Fibrin Mesh
Signup and view all the flashcards
Extrinsic Pathway (Tissue Factor)
Extrinsic Pathway (Tissue Factor)
Signup and view all the flashcards
Intrinsic Pathway (Contact)
Intrinsic Pathway (Contact)
Signup and view all the flashcards
What does bleeding time measure?
What does bleeding time measure?
Signup and view all the flashcards
What forms the fibrin mesh?
What forms the fibrin mesh?
Signup and view all the flashcards
Stages of Haemostasis
Stages of Haemostasis
Signup and view all the flashcards
What is vasoconstriction?
What is vasoconstriction?
Signup and view all the flashcards
Platelet plug formation
Platelet plug formation
Signup and view all the flashcards
Coagulation
Coagulation
Signup and view all the flashcards
Extrinsic Pathway
Extrinsic Pathway
Signup and view all the flashcards
Intrinsic pathway
Intrinsic pathway
Signup and view all the flashcards
How does vasoconstriction occur?
How does vasoconstriction occur?
Signup and view all the flashcards
What helps platelets adhere?
What helps platelets adhere?
Signup and view all the flashcards
What happens in the Common pathway?
What happens in the Common pathway?
Signup and view all the flashcards
Clot retraction
Clot retraction
Signup and view all the flashcards
What breaks down a clot?
What breaks down a clot?
Signup and view all the flashcards
Study Notes
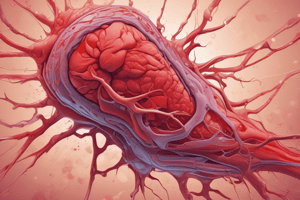
What is Haemostasis?
- The process of stopping bleeding
- Multiple processes occur when a blood vessel is damaged
- Important because blood is essential for organ nourishment and rapid blood loss can be life-threatening
Why is Haemostasis Important?
- When injured, rapid blood loss must be stopped
- Blood is a connective tissue essential for nourishing organs
Consequences of Rapid Blood Loss
- Minor Loss: Homeostatic mechanisms maintain blood volume and cell count
- Moderate Loss: Symptoms include headache, fatigue, nausea, sweating, and dizziness
- Severe Loss: Symptoms include clammy, cold, pale skin, rapid, shallow breathing, rapid heart rate, weakness, confusion, weak pulse, little or no urine output, blue lips and fingernails, light-headedness, loss of consciousness, and death
Stages of Haemostasis
- Primary Haemostasis: Includes vasoconstriction and platelet plug formation
- Secondary Haemostasis: Includes coagulation - the formation of a fibrin mesh
Primary Haemostasis
- Vasoconstriction: Blood vessels constrict, reducing blood flow. Platelets adhere to the damaged vessel wall and release serotonin (5-HT) and thromboxanes, which cause smooth muscle contraction.
- Platelet Plug Formation: Platelets clump around exposed collagen fibers, forming a plug. von Willebrand factor stabilizes the plug.
- Platelets release adenosine diphosphate (ADP), attracting other platelets to the site.
Bleeding Time
- Measures the time required for primary haemostasis (vessel constriction and platelet plug formation)
- Normal range is 2-7 minutes
- Prolonged bleeding time can be caused by thrombocytopenia, severe anemia, collagen disorders (e.g., Ehlers-Danlos syndrome), von Willebrand’s disease, or antiplatelet drugs (e.g., aspirin, clopidogrel).
Secondary Haemostasis
- Coagulation: A complex process involving the clotting cascade, which results in the formation of insoluble fibrin strands that stabilize the platelet plug.
- Fibrin Formation: Soluble fibrinogen is converted to insoluble fibrin through the clotting cascade.
- Fibrin Mesh: The fibrin mesh traps red and white blood cells, forming a clot.
Coagulation Cascade
- Extrinsic Pathway (Tissue Factor Pathway): triggered by tissue factor (factor III) released from damaged endothelial cells. Tissue factor converts factor VII to VIIa, which activates factor X to factor Xa, leading to the common pathway. Measured by Prothrombin Time (PT), with a normal value of 11-16 seconds.
- Intrinsic Pathway (Contact Pathway): triggered by exposure of blood to collagen fibers in the damaged vessel. Starts with activation of factor XII, which, upon exposure to collagen, becomes factor XIIa and initiates the clotting cascade. Measured by Activated Partial Thromboplastin Time (aPTT), with a normal value of 25-35 seconds.
Dental Relevance
- Dental procedures can cause bleeding
- Bleeding should stop naturally within 4-10 minutes depending on the wound.
- There are many causes of prolonged bleeding, which are addressed in a separate lecture
- Bleeding in dentistry can be controlled by applying pressure, sutures, packing with hemostatic agents (e.g., Surgicel), electrosurgery units, or lasers.
Summary
- Haemostasis is a vital process that stops bleeding and involves primary (vasoconstriction and platelet plug formation) and secondary (coagulation) phases
- The clotting cascade is critical for fibrin formation and clot stabilization
- Understanding haemostasis is important for dental hygienists and therapists who need to manage bleeding during dental procedures
Haemostasis
- The process of stopping bleeding
- Involves three stages: vasoconstriction, platelet plug formation, and coagulation
Vasoconstriction
- Blood vessels constrict to reduce blood loss
- Mediated by factors like serotonin and thromboxanes released by platelets
Platelet Plug Formation
- Platelets adhere to exposed collagen in damaged vessel walls
- Von Willebrand factor facilitates platelet adhesion
- Platelets release ADP and other factors to attract more platelets, forming a temporary plug
Coagulation
- A complex cascade of events leading to fibrin formation
- Fibrin strengthens the platelet plug, forming a stable clot
Clotting Cascade
- Two pathways converge to form a common pathway:
- Extrinsic pathway: Triggered by tissue factor (Factor III)
- Measured by Prothrombin Time (PT)
- Intrinsic pathway: Triggered by blood exposure to collagen
- Measured by Activated Partial Thromboplastin Time (aPTT)
- Extrinsic pathway: Triggered by tissue factor (Factor III)
- Common pathway:
- Prothrombin is converted to thrombin
- Thrombin converts fibrinogen to fibrin
- Fibrin forms a mesh, stabilizing the clot
Clot Retraction
- Occurs within 24 hours
- Clot shrinks by about 90%
- Pulls the edges of the wound together
Clot Breakdown (Fibrinolysis)
- Plasminogen, a precursor trapped in the clot, is converted to plasmin
- Plasmin breaks down fibrin
- Thrombin-activated fibrinolysis inhibitor (TAFI) stabilizes clots by inhibiting fibrinolysis
Dental Relevance
- Dental procedures often cause minor hemorrhage
- Knowledge of haemostasis is crucial for managing bleeding effectively
- Typical bleeding stops within 4-10 minutes
- Dental tools like pressure, sutures, haemostatic agents, electrosurgery, and lasers can be used to control bleeding
Clotting Disorders
- Haemophilia (A, B, C) causes deficiencies in clotting factors like Factor VIII, IX, and XI.
Anticoagulants
- Medications like Warfarin, Heparin, and Rivaroxaban interfere with the clotting cascade.
- Their use in dental patients requires careful management to prevent excessive bleeding
Bleeding Time
- Time taken for primary haemostasis (vasoconstriction and platelet plug formation)
- Normally 2-7 minutes
- Prolonged in conditions like thrombocytopenia, von Willebrand disease, and anti-platelet drug use
Fibrinolysis Abnormalities
- Enhanced fibrinolysis: Seen in conditions like DIC and metastatic prostate cancer
- Depressed fibrinolysis: Occurs in conditions like alcoholic liver disease, antiphospholipid syndrome, hypothyroidism, chronic renal disease, and pregnancy
Thrombosis
- Formation of a blood clot (thrombus) within a blood vessel
- Caused by overactive coagulation or underactive fibrinolysis
- Most often begins at sites of endothelial damage
Haemorrhage in Dentistry
- Usually managed with:
- Pressure
- Sutures
- Haemostatic agents
- Less common methods include electrosurgery and lasers
Coagulation Factors and Vitamin K
- Most clotting factors are synthesized in the liver
- Vitamin K is essential for the formation of several clotting factors (Factors II, VII, IX, and X)
- Liver disease can impair clotting factor production, leading to bleeding disorders
Summary of the Coagulation Cascade
- Extrinsic and intrinsic pathways converge on the common pathway
- Prothrombin is converted to thrombin
- Fibrinogen is converted to fibrin, forming a stable clot
- Extrinsic pathway is triggered by tissue damage and measured by PT
- Intrinsic pathway is triggered by blood exposure to collagen and measured by aPTT
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.