Podcast
Questions and Answers
Which clinical presentation is most indicative of acute DIC?
Which clinical presentation is most indicative of acute DIC?
- Bleeding diathesis (correct)
- Cyanosis and respiratory failure
- Oliguria and acute renal failure
- Thrombotic events
What laboratory study is essential for diagnosing DIC?
What laboratory study is essential for diagnosing DIC?
- Platelet count
- Complete blood count
- D-dimer levels (correct)
- Liver function tests
What is the main focus of treatment in cases of DIC?
What is the main focus of treatment in cases of DIC?
- To provide constant monitoring without intervention
- To administer high doses of anticoagulants
- To treat or remove the underlying cause (correct)
- To increase platelet levels through transfusion
What is a potential outcome of poor management in DIC treatment?
What is a potential outcome of poor management in DIC treatment?
Chronic DIC is most commonly associated with which condition?
Chronic DIC is most commonly associated with which condition?
Which glycoprotein is responsible for binding collagen during platelet adhesion?
Which glycoprotein is responsible for binding collagen during platelet adhesion?
What role do glycoprotein IIb/IIIa play in platelet aggregation?
What role do glycoprotein IIb/IIIa play in platelet aggregation?
Which pathway of the coagulation cascade is assessed by prothrombin time (PT) assay?
Which pathway of the coagulation cascade is assessed by prothrombin time (PT) assay?
Which factors are involved in the coagulation cascade as cofactors?
Which factors are involved in the coagulation cascade as cofactors?
What initiates the secretion of granule contents in platelets?
What initiates the secretion of granule contents in platelets?
Which factor is considered a key component in both intrinsic and extrinsic pathways of the coagulation cascade?
Which factor is considered a key component in both intrinsic and extrinsic pathways of the coagulation cascade?
In which component of secondary hemostasis do enzymes, substrates, and cofactors play a role?
In which component of secondary hemostasis do enzymes, substrates, and cofactors play a role?
Which substance is characterized as a potent aggregator of platelets?
Which substance is characterized as a potent aggregator of platelets?
Which type of cancer is most frequently associated with disseminated intravascular coagulation (DIC)?
Which type of cancer is most frequently associated with disseminated intravascular coagulation (DIC)?
What is a major consequence of widespread fibrin deposition in DIC?
What is a major consequence of widespread fibrin deposition in DIC?
What triggers DIC in the context of massive trauma?
What triggers DIC in the context of massive trauma?
Which organ is characterized by microinfarcts and haemorrhage in DIC?
Which organ is characterized by microinfarcts and haemorrhage in DIC?
Plasmin contributes to which of the following conditions in DIC?
Plasmin contributes to which of the following conditions in DIC?
What morphological change occurs in the lungs due to DIC?
What morphological change occurs in the lungs due to DIC?
In which context can DIC onset be described as fulminant?
In which context can DIC onset be described as fulminant?
Which of the following statements about organ changes in DIC is accurate?
Which of the following statements about organ changes in DIC is accurate?
What is the primary function of haemostasis?
What is the primary function of haemostasis?
Which factor activates the coagulation cascade in secondary haemostasis?
Which factor activates the coagulation cascade in secondary haemostasis?
What is the role of thrombin in secondary haemostasis?
What is the role of thrombin in secondary haemostasis?
What is the immediate response to vascular injury in haemostasis?
What is the immediate response to vascular injury in haemostasis?
How do normal endothelial cells contribute to haemostasis?
How do normal endothelial cells contribute to haemostasis?
Which of the following is a characteristic of primary haemostasis?
Which of the following is a characteristic of primary haemostasis?
What leads to the eventual resorption of a clot?
What leads to the eventual resorption of a clot?
What is released from activated endothelial cells that promote thrombosis?
What is released from activated endothelial cells that promote thrombosis?
What is a common presentation of Disseminated Intravascular Coagulation (DIC)?
What is a common presentation of Disseminated Intravascular Coagulation (DIC)?
Which of the following conditions may lead to the activation of DIC?
Which of the following conditions may lead to the activation of DIC?
Which factor does TNF promote that contributes to DIC?
Which factor does TNF promote that contributes to DIC?
How does DIC affect hemostasis?
How does DIC affect hemostasis?
What type of hemorrhages can be associated with generalized defects in small vessels?
What type of hemorrhages can be associated with generalized defects in small vessels?
What role do procoagulants from adenocarcinomas play in relation to DIC?
What role do procoagulants from adenocarcinomas play in relation to DIC?
What can the presence of microthrombi in DIC lead to?
What can the presence of microthrombi in DIC lead to?
Which statement is true regarding the size of ecchymosis?
Which statement is true regarding the size of ecchymosis?
Study Notes
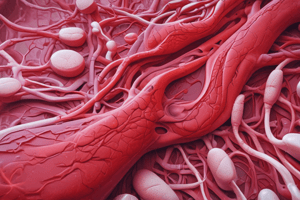
Haemostasis
- Maintains blood in a fluid, clot-free state, crucial for vascular integrity.
- Involves blood clot formation at injury sites; balances clotting and bleeding.
- Imbalance leads to haemorrhagic disorders (excessive bleeding) or thrombotic disorders (excessive clotting).
Steps in Haemostasis
- Vasoconstriction: Immediate response to injury; mediated by neurogenic mechanisms and endothelin; transient effect.
- Primary Haemostasis: Formation of a platelet plug after vascular injury:
- Exposure of von-Willebrand factor and collagen activates platelets.
- Activated platelets transform and recruit more platelets, forming a plug.
- Secondary Haemostasis: Involves fibrin deposition:
- Tissue factor (TF) released from subendothelial cells activates coagulation cascade.
- Thrombin activation converts fibrinogen to insoluble fibrin, stabilizing the platelet plug.
Clot Stabilization and Resorption
- Platelet plug and fibrin contract to form a permanent clot.
- Tissue plasminogen activator (t-PA) initiates fibrinolysis, limiting clot formation and promoting tissue repair.
Role of Endothelial Cells
- Central to maintaining haemostasis balance between thrombosis and antithrombosis.
- Normal endothelial cells produce anticoagulants; become prothrombotic after injury.
- Factors triggering endothelial activation include trauma, infections, inflammation, and toxins.
Platelet Function
- Derived from megakaryocytes; shape changes upon activation.
- Activation sequence:
- Adhesion facilitated by Gp1a/IIa binding to collagen.
- Shape change allows GpIIb/IIIa to bind fibrinogen; phospholipids bind calcium.
- Secretion of granule contents (thrombin and ADP) enhances aggregation via thromboxane A2.
Coagulation Cascade
- Central to secondary haemostasis; drives formation of thrombin.
- Series of enzymatic reactions involving activated coagulation factors, proenzymes, and cofactors, some requiring calcium ions and Vitamin K.
- Divided into extrinsic and intrinsic pathways, defined by laboratory tests.
Clinical Applications of Coagulation Cascade
- Prothrombin time (PT) assay evaluates extrinsic pathway function; identifies defects causing purpura and ecchymosis.
Disseminated Intravascular Coagulation (DIC)
- Acute or chronic thrombohemorrhagic disorder with excessive coagulation leading to microvascular thrombi.
- Secondary complication of conditions like sepsis, trauma, and certain cancers, causing tissue hypoxia and hemorrhage.
Mechanisms Triggering DIC
- Release of procoagulants (placenta in obstetric complications, tissue injury, certain adenocarcinomas).
- Endothelial injury forces expression of tissue factor, pushing hemostatic balance to favor coagulation.
Consequences of DIC
- Widespread fibrin deposition leads to organ ischemia and microangiopathic hemolytic anemia.
- Consumption of platelets and clotting factors leads to a bleeding tendency.
- Fibrin degradation products inhibit platelet aggregation and coagulation.
Diagnosis and Clinical Features of DIC
- Diagnosis involves clinical assessment and laboratory tests measuring fibrinogen, platelets, PT, PTT, and D-dimers.
- Symptoms range from anemia and respiratory failure to acute renal failure and circulatory shock.
Prognosis and Treatment of DIC
- Prognosis varies; depends on the underlying cause.
- Definitive treatment focuses on addressing the inciting disorder.
- Management balances concerns of thrombosis and bleeding; controversial use of anticoagulants/procoagulants in specific cases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the crucial mechanisms of haemostasis, the process that keeps blood in a fluid state and prevents excessive bleeding. This quiz covers the balance between clotting and bleeding, as well as the steps in haemostasis and associated disorders. Understand the importance of thrombosis and haemorrhage in clinical settings.