Podcast
Questions and Answers
What is the primary focus of haemodynamics?
What is the primary focus of haemodynamics?
- Study of blood circulation and properties of blood and vessels (correct)
- Study of respiratory rate
- Study of nutrient absorption
- Study of heart rhythm
What percentage of total blood volume is found within the veins in systemic circulation?
What percentage of total blood volume is found within the veins in systemic circulation?
- 64% (correct)
- 84%
- 16%
- 7%
Which mechanism of capillary exchange involves the movement of oxygen and carbon dioxide from areas of high concentration to low concentration?
Which mechanism of capillary exchange involves the movement of oxygen and carbon dioxide from areas of high concentration to low concentration?
- Bulk flow
- Diffusion (correct)
- Filtration
- Transcytosis
What role do arterioles play in the vascular system?
What role do arterioles play in the vascular system?
What is the name of the mechanisms through which hormones like insulin are transported across capillaries?
What is the name of the mechanisms through which hormones like insulin are transported across capillaries?
Which force primarily drives the movement of fluid from blood into interstitial fluid?
Which force primarily drives the movement of fluid from blood into interstitial fluid?
What percentage of the total blood volume is represented by pulmonary circulation?
What percentage of the total blood volume is represented by pulmonary circulation?
What term describes the movement of fluid from blood capillaries into interstitial fluid?
What term describes the movement of fluid from blood capillaries into interstitial fluid?
Which pressure is associated with forcing fluid inward through the capillary membrane?
Which pressure is associated with forcing fluid inward through the capillary membrane?
What physiological phenomenon is defined by a systolic blood pressure of 200/100 mmHg during resting conditions?
What physiological phenomenon is defined by a systolic blood pressure of 200/100 mmHg during resting conditions?
What is the normal range for diastolic blood pressure?
What is the normal range for diastolic blood pressure?
In terms of blood pressure regulation, which factor is NOT directly mentioned as affecting blood pressure?
In terms of blood pressure regulation, which factor is NOT directly mentioned as affecting blood pressure?
Which pressure directly opposes the capillary pressure in fluid exchange?
Which pressure directly opposes the capillary pressure in fluid exchange?
Which of the following best represents what MAP stands for?
Which of the following best represents what MAP stands for?
What is the characteristic of malignant hypertension?
What is the characteristic of malignant hypertension?
What does an increase in total peripheral resistance (TPR) result from?
What does an increase in total peripheral resistance (TPR) result from?
What is the mean pressure combining arterial, capillary, and venous readings?
What is the mean pressure combining arterial, capillary, and venous readings?
Which of the following factors is NOT involved in regulating blood pressure?
Which of the following factors is NOT involved in regulating blood pressure?
What type of regulation is primarily involved in short-term blood pressure control?
What type of regulation is primarily involved in short-term blood pressure control?
Which chemoreceptor responds primarily to low oxygen levels?
Which chemoreceptor responds primarily to low oxygen levels?
During the auscultatory method of measuring blood pressure, what causes the sounds known as Korotkoff sounds?
During the auscultatory method of measuring blood pressure, what causes the sounds known as Korotkoff sounds?
What role do baroreceptors play in blood pressure regulation?
What role do baroreceptors play in blood pressure regulation?
What is the primary effect of inhalation on venous pressure?
What is the primary effect of inhalation on venous pressure?
Which of the following hormones is involved in long-term regulation of blood pressure?
Which of the following hormones is involved in long-term regulation of blood pressure?
What determines blood flow according to Ohm's Law?
What determines blood flow according to Ohm's Law?
How does an increase in resistance affect blood flow?
How does an increase in resistance affect blood flow?
What arrangement of blood vessels allows each tissue to regulate its own blood flow?
What arrangement of blood vessels allows each tissue to regulate its own blood flow?
If blood vessels are arranged in series, how is total resistance calculated?
If blood vessels are arranged in series, how is total resistance calculated?
What happens to the pressure as blood flows through a series of vessels?
What happens to the pressure as blood flows through a series of vessels?
What is the effect of increased blood viscosity on blood flow?
What is the effect of increased blood viscosity on blood flow?
In a parallel arrangement of blood vessels, how is total resistance calculated?
In a parallel arrangement of blood vessels, how is total resistance calculated?
What is the typical pressure difference between the aorta and the vena cava?
What is the typical pressure difference between the aorta and the vena cava?
What happens to blood flow in anemia as viscosity decreases?
What happens to blood flow in anemia as viscosity decreases?
How does vessel length affect resistance in the circulatory system?
How does vessel length affect resistance in the circulatory system?
What is the relationship between blood vessel diameter and resistance?
What is the relationship between blood vessel diameter and resistance?
What is the velocity of blood flow through the aorta under resting conditions?
What is the velocity of blood flow through the aorta under resting conditions?
Which factor is NOT one of the main determinants of blood flow velocity?
Which factor is NOT one of the main determinants of blood flow velocity?
What role does vascular distensibility play in blood circulation?
What role does vascular distensibility play in blood circulation?
According to Poiseuille’s law, the flow rate (F) is influenced by which of the following parameters?
According to Poiseuille’s law, the flow rate (F) is influenced by which of the following parameters?
Which of the following statements about atherosclerosis is correct?
Which of the following statements about atherosclerosis is correct?
What factor primarily describes the ability of blood vessels to stretch and store blood under pressure?
What factor primarily describes the ability of blood vessels to stretch and store blood under pressure?
Which blood vessel type has a higher compliance compared to its corresponding artery?
Which blood vessel type has a higher compliance compared to its corresponding artery?
During blood loss, which mechanism helps to maintain arterial pressure?
During blood loss, which mechanism helps to maintain arterial pressure?
What is the primary source of blood reservoir in the circulatory system?
What is the primary source of blood reservoir in the circulatory system?
Which substance is NOT typically involved in the hormonal regulation of blood flow?
Which substance is NOT typically involved in the hormonal regulation of blood flow?
What role does vasopressin play during severe hemorrhage?
What role does vasopressin play during severe hemorrhage?
How does the compliance of veins compare to that of arteries?
How does the compliance of veins compare to that of arteries?
Which of the following factors is NOT involved in regulating blood flow to tissues?
Which of the following factors is NOT involved in regulating blood flow to tissues?
Flashcards
Haemodynamics
Haemodynamics
The study of physical laws governing blood circulation, encompassing the properties of blood and blood vessels.
Systemic Circulation
Systemic Circulation
The circulatory network supplying blood to all body tissues except the lungs. Consists of arteries, veins, arterioles, and capillaries.
Pulmonary Circulation
Pulmonary Circulation
The circulatory network that transports blood between the heart and lungs for oxygenation.
Arteries
Arteries
Signup and view all the flashcards
Arterioles
Arterioles
Signup and view all the flashcards
Capillaries
Capillaries
Signup and view all the flashcards
Venules
Venules
Signup and view all the flashcards
Veins
Veins
Signup and view all the flashcards
Capillary Pressure (Pc)
Capillary Pressure (Pc)
Signup and view all the flashcards
Interstitial Fluid Pressure (Pif)
Interstitial Fluid Pressure (Pif)
Signup and view all the flashcards
Capillary Plasma Colloid Osmotic Pressure (Πp)
Capillary Plasma Colloid Osmotic Pressure (Πp)
Signup and view all the flashcards
Interstitial Fluid Colloid Osmotic Pressure (Πif)
Interstitial Fluid Colloid Osmotic Pressure (Πif)
Signup and view all the flashcards
Net Filtration Pressure
Net Filtration Pressure
Signup and view all the flashcards
Blood Pressure (BP)
Blood Pressure (BP)
Signup and view all the flashcards
Systolic Blood Pressure
Systolic Blood Pressure
Signup and view all the flashcards
Diastolic Blood Pressure
Diastolic Blood Pressure
Signup and view all the flashcards
Mean blood pressure
Mean blood pressure
Signup and view all the flashcards
End-diastolic volume (EDV)
End-diastolic volume (EDV)
Signup and view all the flashcards
Contractility
Contractility
Signup and view all the flashcards
Afterload
Afterload
Signup and view all the flashcards
Total peripheral resistance (TPR)
Total peripheral resistance (TPR)
Signup and view all the flashcards
Baroreceptor reflex
Baroreceptor reflex
Signup and view all the flashcards
Central chemoreceptors
Central chemoreceptors
Signup and view all the flashcards
Peripheral chemoreceptors
Peripheral chemoreceptors
Signup and view all the flashcards
Velocity of blood flow
Velocity of blood flow
Signup and view all the flashcards
Cardiac output (CO)
Cardiac output (CO)
Signup and view all the flashcards
Cross-sectional area (TCA)
Cross-sectional area (TCA)
Signup and view all the flashcards
Viscosity of blood
Viscosity of blood
Signup and view all the flashcards
Conductance of a vessel
Conductance of a vessel
Signup and view all the flashcards
Vascular Distensibility
Vascular Distensibility
Signup and view all the flashcards
Distensible nature of arteries
Distensible nature of arteries
Signup and view all the flashcards
Veins: Most distensible vessels
Veins: Most distensible vessels
Signup and view all the flashcards
Vascular Resistance
Vascular Resistance
Signup and view all the flashcards
Series Flow
Series Flow
Signup and view all the flashcards
Parallel Flow
Parallel Flow
Signup and view all the flashcards
Pressure Difference (ΔP)
Pressure Difference (ΔP)
Signup and view all the flashcards
Viscosity
Viscosity
Signup and view all the flashcards
Blood Viscosity Increase
Blood Viscosity Increase
Signup and view all the flashcards
Polycythemia
Polycythemia
Signup and view all the flashcards
Ohm's Law (in Hemodynamics)
Ohm's Law (in Hemodynamics)
Signup and view all the flashcards
Vascular Compliance
Vascular Compliance
Signup and view all the flashcards
Vein Compliance vs Artery Compliance
Vein Compliance vs Artery Compliance
Signup and view all the flashcards
Venous System as Blood Reservoir
Venous System as Blood Reservoir
Signup and view all the flashcards
Venous Constriction During Blood Loss
Venous Constriction During Blood Loss
Signup and view all the flashcards
Other Blood Reservoirs
Other Blood Reservoirs
Signup and view all the flashcards
Functions of Blood Flow to Tissues
Functions of Blood Flow to Tissues
Signup and view all the flashcards
Hormonal Vasoconstrictors
Hormonal Vasoconstrictors
Signup and view all the flashcards
Examples of Vasoconstrictors
Examples of Vasoconstrictors
Signup and view all the flashcards
Study Notes
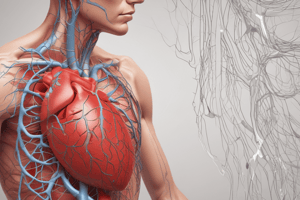
Circulatory System
- The circulatory system is responsible for blood circulation, encompassing both blood and blood vessels.
- Haemodynamics studies the physical laws governing blood circulation and blood vessel characteristics.
Systemic Circulation
- Systemic circulation (peripheral circulation) supplies blood to all body tissues except the lungs.
- This comprises approximately 84% of the circulatory system.
- Blood flow distribution to various tissues is: 64% in veins, 13% in arteries, 7% in systemic arterioles and capillaries.
Pulmonary Circulation
- Pulmonary circulation is dedicated to supplying the lungs, comprising about 16% of the circulatory system.
- This involves:
- 9% in pulmonary blood vessels
- 7% in the heart
Vascular System
- Arteries: Large, elastic arteries carry blood from the heart to muscular arteries that branch to organs. Arterioles deliver blood to capillaries.
- Arterioles: These regulate blood flow to capillaries through precapillary sphincters and metarterioles.
- Capillaries: Tiny vessels where nutrient and waste exchange between blood and interstitial fluid occurs.
- Venules: These are small veins formed by the convergence of capillaries; they transport blood back to the heart.
- Veins: Large, compliant vessels with low resistance; they carry blood back to the heart with valves to prevent backflow.
- Vasa vasorum: These are small blood vessels that supply blood to the walls of larger blood vessels.
Microcirculation of Capillary Exchange
- Substances move between blood and interstitial fluid via three mechanisms:
- Diffusion: Movement of O2, CO2, nutrients, and wastes across the capillary membrane down their respective concentration gradients.
- Transcytosis: Transport of large molecules like hormones and antibodies across the capillary wall via vesicles.
- Bulk flow: Movement of fluid and solutes between blood and interstitial fluid via filtration (blood to interstitial fluid) and reabsorption (interstitial fluid to blood) mechanisms.
Capillary Exchange in Kidneys and other Organs
- Four forces influence fluid movements across capillary walls:
- Capillary pressure (Pc) – pushes fluid outward.
- Interstitial fluid pressure (Pif) – pushes fluid inward.
- Capillary plasma colloid osmotic pressure (πp) – pulls fluid inward.
- Interstitial fluid colloid osmotic pressure (πif) – pulls fluid outward.
Blood Pressure
- Blood pressure is the force exerted by blood against the vessel walls.
- Normal blood pressure is 120/80 mmHg.
- Blood pressure is the product of cardiac output and vascular resistance.
Hypertension and Hypotension
- Hypertension:
- Elevated systemic blood pressure.
- Types include primary (essential), benign and malignant.
- Hypotension:
- Lowered systemic blood pressure.
Pulse Pressure
- The difference between systolic and diastolic pressures.
- The two primary factors influencing pulse pressure include stroke volume and compliance of the arterial tree.
Blood Flow
- The amount of blood that flows through a particular tissue per unit time.
- Two types of blood flow are laminar and non-pulsatile (steady).
- The third type is turbulent flow.
Factors Determining Blood Flow
- Pressure gradient: Driving force for blood flow.
- Resistance to blood flow: Opposing force to blood flow.
- Blood vessel diameter: Crucial for resistance to blood flow.
- Velocity and viscosity of blood: Blood velocity and viscosity influence blood flow.
Blood Flow and Resistance
- Resistance to blood flow plays a pivotal role in influencing local blood pressure and affects blood flow as well. There are several factors which contribute to resistance including blood viscosity, total blood vessel length and blood vessel diameter.
Vascular Resistance
- Resistance occurs in series, or parallel, circuits. When blood vessels are arranged in series, the resistance collectively is the sum of individual resistances. In parallel arrangements, resistance is lower than that in series arrangements.
Vascular Control by lons
- Vasoconstrictors: Calcium ions increase vasoconstriction.
- Vasodilators: Potassium and magnesium ions, hydrogen ions, and anions like acetate and citrate cause vasodilation. Carbon dioxide also causes vasodilation.
Hormonal Vasoconstrictors and Vasodilators
- Hormonal vasoconstrictors (e.g., Norepinephrine, Angiotensin II, and Vasopressin, Endothelin): These hormones promote vasoconstriction in various situations.
- Hormonal vasodilators (e.g., bradykinin, histamine): These promote vasodilation and regulate blood flow to specific tissues.
Factors regulating blood flow to tissues
- Delivery of oxygen, nutrients (e.g. glucose, amino acids, and fatty acids), and removal of waste products (e.g CO2, H+ ions) and other ions. This includes the transport of hormones to the tissues, as well.
Vascular Distensibility and Compliance
- Vascular distensibility refers to a vessel's ability to stretch.
- Vascular compliance pertains to the ability of the circulatory system to accommodate blood volume changes.
- Veins have significantly higher distensibility and compliance than arteries.
Venous System as a Blood Reservoir
- The venous system holds a substantial proportion of circulating blood (約60%).
- When blood loss occurs, the venous system acts as a reservoir, constricting to deliver blood to peripheral tissues as needed. Some organs that serve as reservoirs include the spleen, liver and venous plexus around the skin.
Neurological Regulation of Blood Pressure
- Cardiovascular center: Plays a crucial role in regulating heart rate and blood vessel tone; it is activated by impulses from higher brain centers, baroreceptors, and chemoreceptors. There are distinct cardio inhibitory and cardio acceleratory centers.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.