Podcast
Questions and Answers
A patient, in their first pregnancy, delivers twins at term. They have no history of miscarriages or abortions. What is their gravidity and parity (GTPAL)?
A patient, in their first pregnancy, delivers twins at term. They have no history of miscarriages or abortions. What is their gravidity and parity (GTPAL)?
- G1P1002 (correct)
- G2P2002
- G2P1002
- G1P2002
Which historical element is especially pertinent when taking a patient's medical history?
Which historical element is especially pertinent when taking a patient's medical history?
- History of cardiovascular endurance
- History of renal disease (correct)
- History of dermatological conditions
- History of ocular disorders
Which element is not typically assessed as part of a patient's Review Of Systems (ROS)?
Which element is not typically assessed as part of a patient's Review Of Systems (ROS)?
- Cardiac
- Pulmonary
- Endocrine (correct)
- General
During the physical exam, which of the following is included in the assessment?
During the physical exam, which of the following is included in the assessment?
What is the recommendation regarding routine internal pelvic examinations for asymptomatic patients under the age of 21?
What is the recommendation regarding routine internal pelvic examinations for asymptomatic patients under the age of 21?
In preparation for a pelvic exam, besides gloves and a light source, what essential supply should be assembled?
In preparation for a pelvic exam, besides gloves and a light source, what essential supply should be assembled?
To ensure patient comfort during a pelvic exam, what specific positioning instruction should be given?
To ensure patient comfort during a pelvic exam, what specific positioning instruction should be given?
During a speculum exam, what specific action should be taken if the cervix is initially difficult to locate?
During a speculum exam, what specific action should be taken if the cervix is initially difficult to locate?
What is the MOST critical reason for taking cultures from the cervical os AFTER obtaining the Pap smear specimens?
What is the MOST critical reason for taking cultures from the cervical os AFTER obtaining the Pap smear specimens?
When performing the bimanual examination, what is the primary purpose of placing one hand on the lower abdomen above the symphysis pubis while elevating the cervix and uterus with the pelvic hand?
When performing the bimanual examination, what is the primary purpose of placing one hand on the lower abdomen above the symphysis pubis while elevating the cervix and uterus with the pelvic hand?
During the speculum exam, after the cervix is visualized and before the speculum is removed, the vaginal walls should be inspected. What specific action should the examiner instruct the patient to perform at this stage, and what is the primary reason for this instruction?
During the speculum exam, after the cervix is visualized and before the speculum is removed, the vaginal walls should be inspected. What specific action should the examiner instruct the patient to perform at this stage, and what is the primary reason for this instruction?
What is the MOST precise method for inserting the speculum to minimize patient discomfort and ensure effective visualization of the cervix?
What is the MOST precise method for inserting the speculum to minimize patient discomfort and ensure effective visualization of the cervix?
During the female pelvic examination, what specific set of positional instructions should be given to the patient concerning their hips?
During the female pelvic examination, what specific set of positional instructions should be given to the patient concerning their hips?
When initiating a pelvic examination, what's the most appropriate verbal approach to empower the patient?
When initiating a pelvic examination, what's the most appropriate verbal approach to empower the patient?
During the inspection phase of a female genitalia exam, which specific areas are inspected? (Select the MOST complete answer)
During the inspection phase of a female genitalia exam, which specific areas are inspected? (Select the MOST complete answer)
When inspecting the mons pubis during an external exam, the primary characteristic to observe is:
When inspecting the mons pubis during an external exam, the primary characteristic to observe is:
What specific attributes should be assessed when inspecting the labia majora during a female external exam?
What specific attributes should be assessed when inspecting the labia majora during a female external exam?
When examining the clitoris, what specific characteristics should be evaluated to ensure a comprehensive assessment?
When examining the clitoris, what specific characteristics should be evaluated to ensure a comprehensive assessment?
During the external examination of a female patient, what findings related to the urinary meatus warrant careful inspection?
During the external examination of a female patient, what findings related to the urinary meatus warrant careful inspection?
When evaluating the vaginal introitus, which specific characteristics should be inspected to ensure thoroughness?
When evaluating the vaginal introitus, which specific characteristics should be inspected to ensure thoroughness?
During palpation of the Bartholin glands, at what approximate positions should each side be palpated to accurately assess for swelling or tenderness?
During palpation of the Bartholin glands, at what approximate positions should each side be palpated to accurately assess for swelling or tenderness?
Why is lubrication used sparingly during a speculum examination.
Why is lubrication used sparingly during a speculum examination.
During a speculum examination, at what angle should the speculum be initially inserted into the vagina?
During a speculum examination, at what angle should the speculum be initially inserted into the vagina?
In what sequence are specimens typically collected during a pelvic exam when a Pap smear and cervical cultures are indicated?
In what sequence are specimens typically collected during a pelvic exam when a Pap smear and cervical cultures are indicated?
During the bimanual examination, what is the purpose of applying downward pressure with the abdominal hand while simultaneously elevating the cervix with the pelvic hand?
During the bimanual examination, what is the purpose of applying downward pressure with the abdominal hand while simultaneously elevating the cervix with the pelvic hand?
Upon visualizing the cervix during a speculum exam, which of the following cervical surface characteristics is considered a variation of normal and not necessarily pathological, often appearing as smooth, raised, and yellowish?
Upon visualizing the cervix during a speculum exam, which of the following cervical surface characteristics is considered a variation of normal and not necessarily pathological, often appearing as smooth, raised, and yellowish?
After visualizing the cervix and before removing the speculum, the text advises inspecting the vaginal walls. What specific patient instruction is recommended at this stage to aid in the assessment, and what is the primary diagnostic goal?
After visualizing the cervix and before removing the speculum, the text advises inspecting the vaginal walls. What specific patient instruction is recommended at this stage to aid in the assessment, and what is the primary diagnostic goal?
A patient who is G3P1011 is currently pregnant. Which of the following statements is MOST accurate regarding their obstetric history?
A patient who is G3P1011 is currently pregnant. Which of the following statements is MOST accurate regarding their obstetric history?
When taking a family history (FH), which of the following conditions is MOST pertinent to a gynecological assessment?
When taking a family history (FH), which of the following conditions is MOST pertinent to a gynecological assessment?
Which of the following elements is typically assessed as part of the patient's general Review Of Systems (ROS)?
Which of the following elements is typically assessed as part of the patient's general Review Of Systems (ROS)?
During a routine pelvic exam on a 24-year-old patient, the examiner notes an absence of the usual cervical landmarks. Which of the following is the MOST appropriate next step?
During a routine pelvic exam on a 24-year-old patient, the examiner notes an absence of the usual cervical landmarks. Which of the following is the MOST appropriate next step?
What critical step should be taken immediately prior to inserting a speculum during a pelvic examination, to ensure accurate collection of samples and prevent contamination?
What critical step should be taken immediately prior to inserting a speculum during a pelvic examination, to ensure accurate collection of samples and prevent contamination?
A 19-year-old presents for her first gynecological exam requesting contraception. She has no complaints, is sexually active, and reports regular menses. Considering her age and lack of symptoms, what is the MOST appropriate approach regarding the pelvic exam?
A 19-year-old presents for her first gynecological exam requesting contraception. She has no complaints, is sexually active, and reports regular menses. Considering her age and lack of symptoms, what is the MOST appropriate approach regarding the pelvic exam?
During a pelvic exam, visualization of which anatomical structure confirms proper speculum insertion and provides a necessary landmark for further assessment?
During a pelvic exam, visualization of which anatomical structure confirms proper speculum insertion and provides a necessary landmark for further assessment?
During the female pelvic examination, what is the PRIMARY combined action concerning the hips that optimizes access and comfort?
During the female pelvic examination, what is the PRIMARY combined action concerning the hips that optimizes access and comfort?
When initiating a pelvic examination, what's the MOST suitable verbal approach to ensure the patient feels empowered and in control?
When initiating a pelvic examination, what's the MOST suitable verbal approach to ensure the patient feels empowered and in control?
During the inspection phase of a female genitalia exam, which areas are inspected to ensure comprehensive coverage?
During the inspection phase of a female genitalia exam, which areas are inspected to ensure comprehensive coverage?
When examining the clitoris during a female external exam, what SPECIFIC characteristics should be evaluated to ensure a comprehensive assessment?
When examining the clitoris during a female external exam, what SPECIFIC characteristics should be evaluated to ensure a comprehensive assessment?
During the external examination of a female patient, which finding related to the urinary meatus warrants the MOST careful inspection?
During the external examination of a female patient, which finding related to the urinary meatus warrants the MOST careful inspection?
Why is it preferable to lubricate the speculum with warm water rather than a standard lubricant during a speculum examination?
Why is it preferable to lubricate the speculum with warm water rather than a standard lubricant during a speculum examination?
Flashcards
Gravidity (G)
Gravidity (G)
Number of pregnancies a woman has had, regardless of the outcome or number of babies.
Term (T)
Term (T)
Number of term pregnancies (37 weeks or later) a woman has had.
Pre-term (P)
Pre-term (P)
Number of preterm pregnancies (between 20 and 37 weeks) a woman has had.
Abortions
Abortions
Signup and view all the flashcards
History
History
Signup and view all the flashcards
Pelvic Exam Equipment
Pelvic Exam Equipment
Signup and view all the flashcards
Positioning of a Patient for a Pelvic Exam
Positioning of a Patient for a Pelvic Exam
Signup and view all the flashcards
Speculum
Speculum
Signup and view all the flashcards
Speculum Insertion Technique
Speculum Insertion Technique
Signup and view all the flashcards
Cervical Assessment Points
Cervical Assessment Points
Signup and view all the flashcards
Papanicolaou (Pap) Smear
Papanicolaou (Pap) Smear
Signup and view all the flashcards
Bimanual Exam
Bimanual Exam
Signup and view all the flashcards
Hip Position for Female Exam
Hip Position for Female Exam
Signup and view all the flashcards
Patient Empowerment
Patient Empowerment
Signup and view all the flashcards
External Genitalia Exam
External Genitalia Exam
Signup and view all the flashcards
Mons Pubis Examination
Mons Pubis Examination
Signup and view all the flashcards
Labia Majora Inspection
Labia Majora Inspection
Signup and view all the flashcards
Labia Minora Inspection
Labia Minora Inspection
Signup and view all the flashcards
Clitoris Examination
Clitoris Examination
Signup and view all the flashcards
Urinary Meatus Inspection
Urinary Meatus Inspection
Signup and view all the flashcards
Vaginal Introitus Inspection
Vaginal Introitus Inspection
Signup and view all the flashcards
Bartholin Gland Palpation
Bartholin Gland Palpation
Signup and view all the flashcards
Polycystic Kidney Disease
Polycystic Kidney Disease
Signup and view all the flashcards
Patient History
Patient History
Signup and view all the flashcards
Gravidity
Gravidity
Signup and view all the flashcards
G1P1002
G1P1002
Signup and view all the flashcards
Review of Systems (ROS)
Review of Systems (ROS)
Signup and view all the flashcards
Physical Exam
Physical Exam
Signup and view all the flashcards
Renal History
Renal History
Signup and view all the flashcards
Bartholinitis
Bartholinitis
Signup and view all the flashcards
Urethral Polyps
Urethral Polyps
Signup and view all the flashcards
Cervical Ectropion
Cervical Ectropion
Signup and view all the flashcards
Urethral Caruncles
Urethral Caruncles
Signup and view all the flashcards
Nabothian Cysts
Nabothian Cysts
Signup and view all the flashcards
Labial Excoriations
Labial Excoriations
Signup and view all the flashcards
Cervical Erythema
Cervical Erythema
Signup and view all the flashcards
Labia Majora Abnormalities
Labia Majora Abnormalities
Signup and view all the flashcards
Cervical Motion Tenderness (CMT)
Cervical Motion Tenderness (CMT)
Signup and view all the flashcards
Genital Swelling
Genital Swelling
Signup and view all the flashcards
Vaginal Wall Bulging
Vaginal Wall Bulging
Signup and view all the flashcards
Skene's Gland Discharge
Skene's Gland Discharge
Signup and view all the flashcards
Urethral Inflammation
Urethral Inflammation
Signup and view all the flashcards
Vaginal Fissures
Vaginal Fissures
Signup and view all the flashcards
Unusual Vaginal Discharge
Unusual Vaginal Discharge
Signup and view all the flashcards
Study Notes
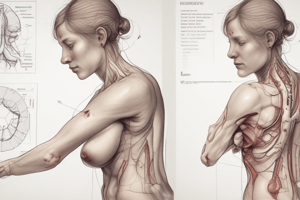
- Female Genitalia: Bates Chapter 21
Instructional Objectives
- Understanding female genitalia anatomy and physiology is important.
- It is important to obtain a thorough patient history regarding changes in menstruation, vaginal bleeding/discharge, or vulvovaginal lesions.
- Understanding risk factors for cervical cancer, STDs, and HIV is important.
- Describing the principles of the pelvic examination is important.
Helpful Definitions
- Menarche refers to the onset of menses.
- Dysmenorrhea is characterized by pain with menses, often with bearing down, aching, or cramping in the lower abdomen or pelvis.
- Premenstrual syndrome (PMS) is a cluster of emotional, behavioral, and physical symptoms that occur 5 days before menses for three consecutive cycles.
- Abnormal uterine bleeding occurs between menses and includes infrequent, excessive, prolonged, or postmenopausal bleeding.
- Menopause is defined as the absence of menses for 12 consecutive months, usually occurring between the ages of 48 and 55 years.
- Postmenopausal bleeding is any bleeding that occurs after menopause.
- Menorrhagia is periods where the bleeding is quite heavy, or the duration is longer than usual.
- Metrorrhagia is bleeding or spotting in between menstruation.
- Menometrorrhagia is a combination of menorrhagia and metrorrhagia.
- Polymenorrhea is having less than 21-day intervals between menses.
- Oligomenorrhea is infrequent bleeding.
- Amenorrhea is the absence of menses.
- Gravidity refers to the number of times a woman has been pregnant.
- Primigravida refers to a woman who is currently pregnant or has been pregnant once.
- Multigravida is a woman who has been pregnant more than once.
- Nulligravida is a woman who has never been pregnant.
- Parity refers to the number of times a woman has given birth to a baby of viable age (≥24 weeks) regardless of birth outcome.
- Primipara (Primip) is a woman who is pregnant for the first time (and has made it beyond viable age) or has given birth to only 1 child.
- Multipara (Multip) is a woman who has given birth 2 or more times.
- Nullipara (Nullip) is a woman who has never given birth or who has never had a pregnancy progress beyond viability.
- Miscarriage (spontaneous abortion) - fetal demise before the 20th week of gestation.
History: Chief Complaint (CC)
- Yearly well-woman visits are important for preventative care.
- Inquiring about menarche and menstruation provides important information about reproductive health.
- Premenstrual syndrome (PMS) presents with a range of symptoms including depression, angry outbursts, irritability, anxiety, and confusion.
- PMS also presents with crying spells, sleep disturbance, poor concentration, social withdrawal, bloating, weight gain, swelling of hands and feet, and generalized aches/pains.
- The criteria to be diagnosed with PMS is the symptoms must be present in the 5 days prior to menses for at least three consecutive cycles, and cessation of symptoms/signs within 4 days after onset of menses, and interfere daily activities.
- Amenorrhea: Primary is absence of ever initiating periods. Secondary is the cessation of periods after they have been established.
- Abnormal bleeding can manifest as menorrhagia, metrorrhagia, and menometrorrhagia.
- Also, abnormal bleeding can present as polymenorrhea, oligomenorrhea, and post coital bleeding.
- Dysmenorrhea is abnormal when interfering with ADLs.
- Primary dysmenorrhea is an increased prostaglandin production during the luteal phase of the menstrual cycle, when estrogen and progesterone levels decline.
- Secondary Dysmenorrhea: Endometriosis, adenomyosis (endometriosis in the muscular layers of the uterus), pelvic inflammatory disease (PID), and endometrial polyps.
- Also, chief complaints include menopause, postmenopausal bleeding, pelvic pain (acute and chronic), and vulvovaginal symptoms.
- Other chief complaints include STIs, sexual health, pregnancy, and urinary symptoms (dysuria, frequency, urgency, incontinence).
History
- HPI: Use OLDCARTS to gather details about the present illness.
- It is important to note pertinent positives/negatives during the HPI.
- PMH: reproductive health history/STI's are important to assess impact on fertility, risk for ectopic pregnancy, and the best contraceptive to prescribe.
- History of UTIs, glomerulonephritis, previous urinary catheterization/dilation, spina bifida (risk factor for recurrent UTI), trauma/spinal cord injury are important.
- Medications and forms of birth control, and surgical history are included when gathering patient history.
Reproductive Health History
- Includes Onset of Menarche and Last Normal Menstrual Period
- Includes Obstetric History: # of Pregnancies, Losses/Abortions, Delivery History
- Includes Gynecological History: Ovarian cyst, Endometriosis, Infertility/treatments, Fibroids, Salpingitis, Tubo-ovarian
- Includes Sexual History
- Includes Screenings: Last pap smear, Last mammogram
Reproductive Health History/Sexual History: The 5 "Ps+"
- Partners includes genders of sexual partners, recent sexual intercourse, # of partners in the last 6 months, 5 years, and lifetime, any new partners in the last 6 months
- Practices includes Types of sex (oral, vaginal, anal, etc).
- Protection from STIs includes Use of condoms.
- Past history of STIs includes what kind of STI, when did they have it, what treatment, last screening
- Pregnancy Plans includes any plans or desire to have (more) children and discussing concerns, birth control, etc.
- Plus encompasses an assessment of trauma, violence, sexual satisfaction, sexual health concerns/problems, and support for sexual orientation and gender identify (SOGI)
Reproductive Health History/OB History
- Gravidity and Parity can be documented succinctly as G and P.
- A G2P2 has had two pregnancies and two deliveries after 24 weeks.
- A G2P0 has had two pregnancies, neither of which survived to a gestational age of 24 weeks.
- Parity can be broken down even further G,P(TPAL)
- G= Gravidity - # of pregnancies
- P= Parity
- T= Term- # of term pregnancies/deliveries
- 37-40 weeks
- P= Premature- # of premature pregnancies/deliveries
- 20-36 weeks
- A= Abortions/miscarriages
- Elective abortions and spontaneous abortions
- L= Living children
- If a woman with two spontaneous losses prior to 20 weeks gestation, 3 living children who were delivered at term, and currently pregnant = G6P3023
- For twins it’s important to note that for gravidity, it's about number of pregnancies, not number of babies.
History
- FH: History of renal disease, Polycystic Kidney dz, Renal failure, Cancer
- SH: Sexual history
- ROS: General, Skin, Pulm, Cardiac, GI, GU
Physical Exam
- Includes vital signs, general, skin, pulm, cardiac, and GI
- Rectal exam when indicated
- GU and Pelvic exam
Before preparing for the exam
- Determine if patient is younger than 21 years old.
- Pelvic exams on patients under 21 years old should only occur if indicated by the medical history.
- NO EVIDENCE SUPPORTS THE ROUTINE INTERNAL EXAMINATION OF THE HEALTHY, ASYMPTOMATIC PATIENT BEFORE AGE 21 YEARS.
- Male examiners should be accompanied by female chaperones, and female examiners should be accompanied by a chaperone as well.
Tips for Successful Female Genitalia Exam
- Examiner obtains permission and selects chaperone
- Examiner explains each step of the examination in advance
- Examiner drapes the patient from midabdomen to knees and depresses the drape between the knees to provide eye contact with patient
- Examiner avoids unexpected or sudden movements and chooses a speculum that is the correct size, as well as, warms the speculum with tap water
- Examiner monitors the comfort of the examination by watching the patient's face and obtaining verbal feedback
- Examiner uses excellent but gentle technique, especially when inserting the speculum (see p. 699)
- Patient avoids intercourse, douching, or use of vaginal suppositories for 24 to 48 hours before examination
- Patient empties bladder before the physical exam
- Patient lies supine, with head and shoulders elevated, and arms at her sides or folded across the chest to enhance eye contact and reduce tightening of abdominal muscles
Prep for the Pelvic Exam
- Assemble equipment, which includes Moveable light source, Gloves, Vaginal speculum of appropriate size, Water-soluble lubricant, Pap smear equipment (if indicated), Specimen/culture equipment (if
Make Sure The Patient is Comfortable
- Assist the patient into lithotomy position
- May be warmer and feel less exposed with socks on
- Patient slides all the way down the exam table until her buttocks extend slightly beyond the edge with the hips flexed, abducted, and externally rotated
- Head is supported with a pillow
Touching the Patient
- Give the patient power by your words such as, "This is the speculum I will use", "We will begin the examination now with your permission", and "You will feel the back of my hand"
GU Female Exam
- Involves inspection (and palpation if indicated) of the external genitalia
- Inspect Mons pubis, labia majora and perineum, labia minora, clitoris, urethral meatus, and Also, Anus
External Exam inspection of:
- Inspect: pubic hair pattern/distribution
- Labia majora: color, symmetry, moisture, scarring, inflammation, swelling.
- Palpate Labia majora for tenderness
- Labia minora: symmetry, moisture, inflammation, discharge, excoriations, lesions
- Palpate Labia minora for tenderness
- Clitoris: Size, atrophy, inflammation, adhesions
- Urinary meatus: Discharge, polyps, caruncles, inflammation
- Vaginal introitus: Moisture, swelling, discoloration, discharge, lesions, fissures
- Skene and Bartholin glands: inspect the discharge and swelling while palpate the bartholin glands for tenderness
Bartholin Glands Exam
- Palpate each side at approximate the 4-o'clock and 8-o'clock position between your finger and thumb
- Check for swelling or tenderness
- Note any discharge exuding from the duct opening of the gland and culture if present
Speculum Examination
- Understand mechanics of the speculum and make sure it's in good working order.
- Preferably lubricate with warm water but only use sparingly because can prevent accurate pap/culture results so use with caution!
Internal Exam-Speculum Exam
- Advise patient they you will now place the speculum in the vagina
- Place 1-2 fingers in the posterior introitus and press downward
- If needed, locate the position of the cervix with your fingers to guide the direction of the speculum
- With speculum closed, insert at an oblique angle and gradually rotate to horizontal position
- Insert at a 30-degree downward angle towards the cervix
- Gradually open the speculum, bring cervix into view, and lock
- If having difficulty finding the cervix, withdraw slightly and reposition on a different slope
- If discharge obscures the view, wipe away gently with a large cotton swab
- Note the color and symmetry of the cervix
- Note the surface characteristics: Smooth, ectropion, Nabothian cysts, polyps, erythema
- Note the shape of the os
- Note the presence of any discharge and odor, consistency
- Obtain pap smear and cultures if indicated
- Withdraw the speculum just until it clears the cervix, then inspect the vaginal walls- Inspect for color, surface characteristics, lesions, secretions, or bleeding
- Have the patient bear down, and check for bulging in the vaginal wall or incontinence
- Ensuring the speculum has cleared the cervix, close the speculum and remove slowly at the same oblique angle
Papanicolaou (Pap) Smear
- Once the cervix is clearly visualized: Obtain one specimen from the endocervix and another from the ectocervix
- If indicated/consented: Then take cultures from the cervical os
- TAKE CUTURES LAST!!!
GU Female Exam (Bimanual Examination)
- Lubricate index and middle fingers
- Inform patient you will insert fingers
- Insert fingers exerting pressure posteriorly, with the thumb abducted and 4th and 5th fingers flexed into the palm
- Note any lesions or tenderness in the vaginal wall, including the region of the urethra and bladder anteriorly .Palpate the cervix, noting the size, contour/consistency, and assess for cervical motion tenderness
- Palpate the uterus by placing your other hand on the lower abdomen just above the symphysis pubis while you elevate the cervix and uterus with your pelvic hand. Press the abdominal hand in and down, capturing the uterus between your two hands
- Note its position, size, shape, contour/consistency, any masses present, mobility and identify any tenderness.
- Palpate each ovary by placing your abdominal hand on the right lower quadrant and your pelvic hand in the right lateral fornix, pushing your abdominal hand in and down.
- Try to identify the right ovary or any adjacent adnexal masses
- Note the size, shape, consistency, mobility, and tenderness
- Repeat on left side
- DRE (Verbalize only that you will perform)- Note the sphincter tone and any scarring, fissures, lesions, rectal wall masses, polyps, tenderness, uterus position/size/tenderness, stool color, and presence of any blood.
Special Techniques
- Milking the urethra assists to evaluate possible urethritis or inflammation of the paraurethral glands, insert your index finger into the vagina and milk the urethra gently outward from the inside
- Note any discharge from the urethral meatus and if discharge is present, culture it
Common Abnormalities: Vulvar/Vaginal Lesions
- Herpes simplex presents with vesicles/ulcers
- Syphilis
- Cancer
- Bartholin cysts
- HPV presents with warts
Common Abnormalities Presenting as Vaginal Pruritus/Pain
- Candidiasis
- Trichomoniasis
- Herpes simplex with Vesicles
Common Abnormalities Presenting with Vaginal Discharge
- Urethritis/cervicitis
- Chlamydia/GC with Mucopurulent discharge
- Bacterial Vaginosis with Homogeneous white discharge which coats t+clue cells and Fishy odor, "whiff” test
- Candidiasis with White clumped discharge
- Trichomoniasis-Yellow/green, often malodorous discharge with vulvar itching as well as Motile flagellated organisms
Urethrocele
- When a prolapsed urethra protrudes into the anterior vaginal wall
Cystocele
- A bulge of the upper two-thirds of the anterior vaginal wall due to a prolapsed bladder
Cystourethrocele
- When the entire anterior vaginal wall, together with the bladder and urethra, produces the bulge.
Rectocele
- Herniation of the rectum into the posterior wall of the vagina, resulting from a weakness or defect in the endopelvic fascia.
Urethral abnormalities
- Caruncle-Small red benign tumor visible at the posterior urethral meatus is Most common in in postmenopausal women and Typically asymptomatic but it is Important to avo with carcinoma of the
Cervical abnormalities presenting as Mucopurulent discharge
- Mucopurulent cervicitis produces purulent yellow drainage from the cervical os, usually from C. trachomatis, N. gonorrhoeae, or herpes infection.
Carcinoma of the cervix
- Earliest stages-cannot be distinguished from a normal cervix.
- Later stages-an extensive, irregular, cauliflower-like growth may develop.
- Early frequent intercourse, multiple partners, smoking, and infection with human papillomavirus increase the risk for cervical cancer.
Fetal exposure to DES
- Daughters of women who took DES during pregnancy are at greatly increased risk for several abnormalities such as Columnar epithelium that covers most or all of the cervix, Vaginal adenosis (i.e extension of this epithelium to the vaginal wall), A circular collar or ridge of tissue, between the cervix and vagina,Rare carcinoma of the upper vagina.
- Nabothian cysts (AKA Mucinous retention cysts)
Uterine abnormalities
- Fibroids (Myomas): Very common, benign tumors that Vary in number and size.
- Can be firm, irregular nodules
- Prolapse: Weakness of supporting structures of the pelvic floor that is defined in 3-degrees.
- 1st degree-cervix is still well within the vagina
- 2nd degree-cervix is at the introitus
- 3rd degree-cervix and vagina are outside the introitus
Adnexal masses and other causes of pelvic pain includes:
- Ovarian cancer
- Ovarian cysts/tumors that Cysts can be transient or suggestive of PCOS. PCOS-Requires 2/3 factors to be present for diagnosis:
- Androgen excess
- Ovulatory dysfunction
- Polycystic ovaries on U/S
- Ectopic pregnancy, PID, Dysmenorrhea, Endometriosis
Renal Conditions includes?
- UTI and Pyelonephritis, Nephrolithiasis presenting as Gross hematuria, Glomerulonephritis that has Previous history of streptococcal infection with Microscopic hematuria.
- Nephrotic syndrome which presents as Facial edema/increased bp/> 3grams of protein in 24hours
Documentation sample
- "External genitalia without erythema, lesions, or masses. Vaginal mucosa pink. Cervix parous, pink, and without discharge. Uterus anterior, midline, smooth, and not enlarged. No adnexal tenderness. Pap smear obtained. Rectovaginal wall intact. Rectal vault without masses. Stool brown and negative for fecal blood."
- Another Sample: "External genitalia without erythema or lesions. Vaginal mucosa and cervix coated with white homogenous discharge with mild fishy odor. After swabbing cervix, no discharge visible in the cervical os. Uterus midline; no adnexal masses. Rectal vault without masses. Stool brown and negative for fecal blood."
Screen for average-risk women for cervical cancer
- Start screening at 21 years old
- From ages 21-65 screen cytology every 3 years OR
- Ages 30-65 screen with cytology plus HPV testing (for high-risk or oncogenic HPV types) every 5 years; HPV testing alone (age 25 or 30)
- Age >65 yrs, assuming three consecutive negative results on cytology or two consecutive negative results on cytology plus HPV testing within 10 yrs before cessation of screening, with the most recent test performed within 5 yrs
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.