Podcast
Questions and Answers
What is the main distinguishing factor between the diarrheal and emetic syndromes caused by B. cereus?
What is the main distinguishing factor between the diarrheal and emetic syndromes caused by B. cereus?
- Ingestion of preformed toxins (correct)
- The method of diagnosis
- The food sources involved
- The duration of symptoms
Which Clostridium species is characterized by motile rods with terminal bulging spores?
Which Clostridium species is characterized by motile rods with terminal bulging spores?
- C. perfringens
- C. tetani (correct)
- C. botulinum
- C. difficile
Which toxin type produced by B. cereus is resistant to gastric acid and heat?
Which toxin type produced by B. cereus is resistant to gastric acid and heat?
- Enterotoxin
- Heat stable toxin (correct)
- Proteolytic toxin
- Phospholipase
What is the recovery time typically associated with illnesses caused by B. cereus?
What is the recovery time typically associated with illnesses caused by B. cereus?
In diagnosing diarrheal syndrome caused by B. cereus, which of the following samples would be crucial?
In diagnosing diarrheal syndrome caused by B. cereus, which of the following samples would be crucial?
What primary factor influences the development of tetanus caused by C. tetani?
What primary factor influences the development of tetanus caused by C. tetani?
Which Clostridium species is primarily associated with foodborne illness due to heat-labile enterotoxins?
Which Clostridium species is primarily associated with foodborne illness due to heat-labile enterotoxins?
How are ocular infections associated with B. cereus primarily caused?
How are ocular infections associated with B. cereus primarily caused?
What unique characteristic does Bacillus anthracis exhibit regarding its capsule?
What unique characteristic does Bacillus anthracis exhibit regarding its capsule?
Which of the following proteins is NOT part of the anthrax toxin?
Which of the following proteins is NOT part of the anthrax toxin?
What is a primary route of entry for Bacillus anthracis spores in humans?
What is a primary route of entry for Bacillus anthracis spores in humans?
Which disease is specifically caused by inhalation of Bacillus anthracis spores?
Which disease is specifically caused by inhalation of Bacillus anthracis spores?
What type of disease is anthrax primarily categorized as?
What type of disease is anthrax primarily categorized as?
Which of the following statements is true about the D-glutamic acid capsule of Bacillus anthracis?
Which of the following statements is true about the D-glutamic acid capsule of Bacillus anthracis?
In terms of epidemiology, which group of people is most at risk for contracting anthrax?
In terms of epidemiology, which group of people is most at risk for contracting anthrax?
What is the major virulence factor of the anthrax toxin?
What is the major virulence factor of the anthrax toxin?
What primarily prevents the release of inhibitory neurotransmitters in muscle spasm associated with tetanus?
What primarily prevents the release of inhibitory neurotransmitters in muscle spasm associated with tetanus?
Which of the following is NOT a typical clinical sign of tetanus?
Which of the following is NOT a typical clinical sign of tetanus?
In which population is tetanus most likely to occur due to untreated wounds?
In which population is tetanus most likely to occur due to untreated wounds?
What critical step is essential in the treatment of tetanus?
What critical step is essential in the treatment of tetanus?
How often can the bacterium C.tetani be recovered from the wound cultures in patients with tetanus?
How often can the bacterium C.tetani be recovered from the wound cultures in patients with tetanus?
What is the characteristic appearance of C.tetani when observed microscopically?
What is the characteristic appearance of C.tetani when observed microscopically?
What environmental condition is favorable for the growth of bacteria introduced through deep wounds?
What environmental condition is favorable for the growth of bacteria introduced through deep wounds?
What is a potential consequence of spasm in the respiratory muscles during tetanus infection?
What is a potential consequence of spasm in the respiratory muscles during tetanus infection?
What immediate action should be taken for passive immunization against tetanus?
What immediate action should be taken for passive immunization against tetanus?
Which types of botulism are primarily associated with ingestion of toxin?
Which types of botulism are primarily associated with ingestion of toxin?
What is the primary cause of Type E botulism?
What is the primary cause of Type E botulism?
What is a hallmark clinical manifestation of botulism?
What is a hallmark clinical manifestation of botulism?
What method is used to demonstrate the presence of botulinum toxin for diagnosis?
What method is used to demonstrate the presence of botulinum toxin for diagnosis?
What prevents the release of acetylcholine, leading to clinical manifestations in botulism?
What prevents the release of acetylcholine, leading to clinical manifestations in botulism?
What is the recommended frequency for booster injections of the tetanus vaccine?
What is the recommended frequency for booster injections of the tetanus vaccine?
Who can receive tetanus toxoid in the third trimester to aid their neonates?
Who can receive tetanus toxoid in the third trimester to aid their neonates?
Which of the following toxins produced by Clostridium perfringens is primarily responsible for cell membrane breakdown?
Which of the following toxins produced by Clostridium perfringens is primarily responsible for cell membrane breakdown?
What is the key feature of gas gangrene that distinguishes it from other infections?
What is the key feature of gas gangrene that distinguishes it from other infections?
In which type of wound is there a higher likelihood of developing a Clostridium perfringens infection?
In which type of wound is there a higher likelihood of developing a Clostridium perfringens infection?
What role does collagenase play in the virulence of Clostridium perfringens?
What role does collagenase play in the virulence of Clostridium perfringens?
What are the earliest symptoms of gas gangrene?
What are the earliest symptoms of gas gangrene?
Which toxin produced by Clostridium perfringens has blood-destructing activity?
Which toxin produced by Clostridium perfringens has blood-destructing activity?
What is a common outcome for hosts with healthy immune systems regarding Clostridium perfringens infection?
What is a common outcome for hosts with healthy immune systems regarding Clostridium perfringens infection?
What is the significance of anaerobiasis in the context of gas gangrene?
What is the significance of anaerobiasis in the context of gas gangrene?
What sensation may occur when pressing the affected area in cases of gas gangrene?
What sensation may occur when pressing the affected area in cases of gas gangrene?
What color change might occur in tissues affected by gas gangrene?
What color change might occur in tissues affected by gas gangrene?
What is a common symptom associated with Clostridium difficile infection?
What is a common symptom associated with Clostridium difficile infection?
What reaction does Nagler's test detect in relation to Clostridium perfringens?
What reaction does Nagler's test detect in relation to Clostridium perfringens?
What immediate treatment is critical for a patient with gas gangrene?
What immediate treatment is critical for a patient with gas gangrene?
Which antibiotic is specifically indicated for the treatment of Clostridium difficile infections?
Which antibiotic is specifically indicated for the treatment of Clostridium difficile infections?
What consequence is likely without treatment for gas gangrene?
What consequence is likely without treatment for gas gangrene?
What structural feature characterizes Clostridium perfringens as observed under Gram stain?
What structural feature characterizes Clostridium perfringens as observed under Gram stain?
Flashcards
Bacillus anthracis
Bacillus anthracis
A Gram-positive, rod-shaped bacterium, forming endospores.
Anthrax Capsule
Anthrax Capsule
Composed of D-glutamic acid, prevents phagocytosis by immune cells.
Anthrax Transmission
Anthrax Transmission
Spread through contact with infected animals or contaminated materials/products and inhalation of spores.
Anthrax Toxin Proteins
Anthrax Toxin Proteins
Signup and view all the flashcards
Cutaneous Anthrax
Cutaneous Anthrax
Signup and view all the flashcards
Pneumonic Anthrax
Pneumonic Anthrax
Signup and view all the flashcards
Anthrax Pathogenesis
Anthrax Pathogenesis
Signup and view all the flashcards
Anthrax Virulence Factors
Anthrax Virulence Factors
Signup and view all the flashcards
Gram-positive, Spore-forming bacteria
Gram-positive, Spore-forming bacteria
Signup and view all the flashcards
Bacillus cereus toxins
Bacillus cereus toxins
Signup and view all the flashcards
Diarrheal syndrome (B. cereus)
Diarrheal syndrome (B. cereus)
Signup and view all the flashcards
Emetic syndrome (B. cereus)
Emetic syndrome (B. cereus)
Signup and view all the flashcards
Clostridium species (Gram+ve rods)
Clostridium species (Gram+ve rods)
Signup and view all the flashcards
Clostridium tetani
Clostridium tetani
Signup and view all the flashcards
Spore forming characteristics
Spore forming characteristics
Signup and view all the flashcards
Tetanus development factors
Tetanus development factors
Signup and view all the flashcards
Tetanus Transmission
Tetanus Transmission
Signup and view all the flashcards
Tetanus Epidemiology
Tetanus Epidemiology
Signup and view all the flashcards
Tetanospasmin
Tetanospasmin
Signup and view all the flashcards
Tetanus Pathogenesis
Tetanus Pathogenesis
Signup and view all the flashcards
Trismus
Trismus
Signup and view all the flashcards
Diagnosis Challenges
Diagnosis Challenges
Signup and view all the flashcards
Tetanus Treatment
Tetanus Treatment
Signup and view all the flashcards
Tetanus Signs & Symptoms
Tetanus Signs & Symptoms
Signup and view all the flashcards
Passive Immunization (Tetanus)
Passive Immunization (Tetanus)
Signup and view all the flashcards
Clostridium Botulinum
Clostridium Botulinum
Signup and view all the flashcards
Botulism Toxins
Botulism Toxins
Signup and view all the flashcards
Foodborne Botulism
Foodborne Botulism
Signup and view all the flashcards
Infant Botulism
Infant Botulism
Signup and view all the flashcards
Wound Botulism
Wound Botulism
Signup and view all the flashcards
Botulism Diagnosis
Botulism Diagnosis
Signup and view all the flashcards
Botulism Treatment
Botulism Treatment
Signup and view all the flashcards
Gas gangrene
Gas gangrene
Signup and view all the flashcards
Clostridium perfringens toxins
Clostridium perfringens toxins
Signup and view all the flashcards
Wound infection risk factors
Wound infection risk factors
Signup and view all the flashcards
Transmission of Clostridium perfringens
Transmission of Clostridium perfringens
Signup and view all the flashcards
Symptoms of gas gangrene
Symptoms of gas gangrene
Signup and view all the flashcards
Clostridium perfringens enzymes
Clostridium perfringens enzymes
Signup and view all the flashcards
Toxins effect
Toxins effect
Signup and view all the flashcards
Localized infection risk
Localized infection risk
Signup and view all the flashcards
Gas Gangrene Symptoms
Gas Gangrene Symptoms
Signup and view all the flashcards
Clostridium perfringens
Clostridium perfringens
Signup and view all the flashcards
Gas Gangrene Treatment
Gas Gangrene Treatment
Signup and view all the flashcards
Clostridium difficile
Clostridium difficile
Signup and view all the flashcards
Pseudomembranous colitis
Pseudomembranous colitis
Signup and view all the flashcards
C. difficile Treatment
C. difficile Treatment
Signup and view all the flashcards
Lecithinase
Lecithinase
Signup and view all the flashcards
Gas Gangrene Diagnosis
Gas Gangrene Diagnosis
Signup and view all the flashcards
Study Notes
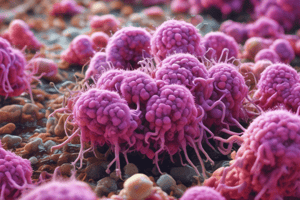
Gram-Positive Rods: Aerobic Spore-Forming
- Genus: Bacillus anthracis
- Capsule: Unique, composed of D-glutamic acid, antiphagocytic
- Transmission: Contact with infected animals, contaminated products, occupational exposure (farmers, butchers, wool workers)
- Virulence Factors: Anthrax toxin (PA, EF, LF), edema toxin (PA + EF), lethal toxin (PA + LF)
- Pathogenesis: Spores enter through injured skin, ingestion, or inhalation; germinate at entry site; lymphatics to bloodstream
- Disease Presentation: Cutaneous (malignant pustule), pulmonary (wool sorter's disease), intestinal (severe abdominal pain) and septicemic anthrax.
Bacillus cereus
- Food Poisoning: Produces toxins, intoxication, not infection; self-limiting
- Properties: Gram-positive, motile, spore-forming, facultative anaerobe
- Transmission: Foodborne (spores survive food preparation),
- Virulence Factors: Two types of toxins: diarrheal toxin (heat-labile), emetic toxin (heat-stable)
- Diarrheal Syndrome: Long incubation time,
- Emetic Syndrome: Short incubation time,
- Diagnosis: Isolation from food or stool,
- Treatment: Supportive care.
Clostridium tetani
- Properties: Motile, spore-forming, anaerobic, terminal bulging spores
- Transmission: Wound contamination with spores (soil, nails)
- Transmission: in-depth wounds
- Epidemiology: Occupational, surgical procedures, neonates
- Virulence Factors: Tetanospasmin, neurotoxin
- Pathogenesis: Blocks neurotransmitter release, muscle rigidity, spasms
- Disease Presentation: Trismus (lockjaw), risus sardonicus, opisthotonos
- Diagnosis: Clinical signs, possibly wound culture.
Clostridium botulinum
- Food Poisoning: Produce toxins (most potent), associated with canned foods, sausages,
- Transmission: Foodborne, wound botulism, infant botulism
- Disease Presentation: Symmetrical descending flaccid paralysis, ocular paralysis, dry mucous membranes
- Diagnosis: Clinical presentation, toxin detection in serum/stool,
- Treatment: Immune globulin therapy.
Clostridium perfringens
- Gas Gangrene: Necrotic infection of tissue.
- Transmission: Deep penetrating wounds, contaminated wounds.
- Epidemiology: Opportunistic organism, wounds.
- Virulence Factors: Diverse range of toxins (damage to cell membranes)
- Pathogenesis: Tissue damage and edema,
- Disease Presentation: Pain, fever, edema, foul-smelling discharge
- Diagnosis: Tissue samples, Gram stain,
Clostridium difficile
- Properties: Gram-positive rod, spore-forming, anaerobic,
- Epidemiology: Normal flora of the GIT, disturbance related to antibiotic therapy
- Virulence Factors: Enterotoxin, induces inflammation
- Disease Presentation: Pseudomembranous colitis. Increased fluid, mucus, and leukocytes
- Diagnosis: Colonoscopy, stool tests,
- Treatment: Antibiotic therapy.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.