Podcast
Questions and Answers
What is the primary treatment for gas gangrene caused by Clostridium perfringens?
What is the primary treatment for gas gangrene caused by Clostridium perfringens?
- Antibiotics alone
- Surgical amputation
- Symptomatic treatment
- Penicillin G plus debridement of the wound (correct)
What is the transmission method for Clostridium botulinum?
What is the transmission method for Clostridium botulinum?
- Improperly preserved food (correct)
- Inhalation of airborne particles
- Direct contact with infected individuals
- Fecal-oral route
Which of the following diseases is associated with Clostridium difficile?
Which of the following diseases is associated with Clostridium difficile?
- Pseudomembranous colitis (correct)
- Nocardiosis
- Botulism
- Actinomycosis
What is a significant characteristic of Actinomyces israelii?
What is a significant characteristic of Actinomyces israelii?
Which method is recommended for preventing botulism?
Which method is recommended for preventing botulism?
Which Gram-positive bacilli are known for their endospore-forming ability?
Which Gram-positive bacilli are known for their endospore-forming ability?
What is the main symptom of food poisoning caused by Bacillus cereus?
What is the main symptom of food poisoning caused by Bacillus cereus?
What is the transmission method for Bacillus anthracis?
What is the transmission method for Bacillus anthracis?
Which of the following is a characteristic feature of Corynebacterium diphtheriae?
Which of the following is a characteristic feature of Corynebacterium diphtheriae?
What type of bacteria causes gastrointestinal anthrax?
What type of bacteria causes gastrointestinal anthrax?
What is a common reservoir for Bacillus cereus?
What is a common reservoir for Bacillus cereus?
Which Gram-positive bacillus is an obligate anaerobe?
Which Gram-positive bacillus is an obligate anaerobe?
What is a distinguishing symptom of cutaneous anthrax?
What is a distinguishing symptom of cutaneous anthrax?
What organism produces the pseudomembrane in the throat associated with diphtheria?
What organism produces the pseudomembrane in the throat associated with diphtheria?
Which treatment is effective against Corynebacterium diphtheriae?
Which treatment is effective against Corynebacterium diphtheriae?
What is the primary habitat of Listeria monocytogenes?
What is the primary habitat of Listeria monocytogenes?
What is the shape of Clostridium tetani when observed under a microscope?
What is the shape of Clostridium tetani when observed under a microscope?
What is a significant predisposing factor for Listeria monocytogenes infections?
What is a significant predisposing factor for Listeria monocytogenes infections?
Which disease is associated with Clostridium perfringens?
Which disease is associated with Clostridium perfringens?
Which prevention method is used against tetanus?
Which prevention method is used against tetanus?
What is the primary route of transmission for Clostridium tetani?
What is the primary route of transmission for Clostridium tetani?
Flashcards are hidden until you start studying
Study Notes
Gram-Positive Bacilli
- There are five medically important genera of gram-positive bacilli: Bacillus, Clostridium, Corynebacterium, Listeria, and Gardnerella.
- Bacillus and Clostridia are spore-forming rods, while Listeria, Gardnerella, and Corynebacterium are not.
- Bacillus species are obligate aerobes, whereas Clostridium species are obligate anaerobes.
Bacillus cereus
- Causes: Food poisoning
- Habitat: Domestic animals, soil, and rice grains
- Transmission: Acquired by eating "reheated rice". Spores germinate when rice is kept warm for many hours.
- Diagnosis: Aerobic, spore-forming, Gram-positive bacillus
- Symptoms: Nausea, vomiting, and non-bloody diarrhea
- Toxin Production: Produces two toxins, one similar to cholera toxin, and another similar to staphylococcal enterotoxin.
Bacillus anthracis
- Causes: Anthrax
- Habitat: Soil
- Transmission: Contact with infected animals, inhalation of spores from animal hair and wool.
- Forms of Anthrax:
- Cutaneous (malignant pustule): Painless ulcer with black eschar (crust, scab) and local edema. Untreated cases progress to bacteremia and death.
- Pulmonary (woolsorter's disease): Begins with flu-like symptoms, rapidly progresses to hemorrhagic mediastinitis, bloody pleural effusions, septic shock, and death.
- Gastrointestinal: Vomiting, abdominal pain, and bloody diarrhea
- Diagnosis: Aerobic, Gram-positive, spore-forming rods, Poly-D-glutamate Capsule (amino acids, NOT polysaccharides)
Corynebacterium diphtheriae
- Causes: Diphtheria
- Habitat: Human throat
- Transmission: Respiratory droplets
- Symptoms: High temperature, chills, sore throat, and enlargement of neck lymph nodes. Grayish membrane on the throat that cannot be removed, and bleeding occurs if pulled away.
- Diagnosis: Club-shaped gram-positive rods arranged in V or L shape. Granules stain metachromatically. Aerobic, Non–spore-forming organism.
- Treatment: Antitoxin made in horses neutralizes the toxin. Penicillin G kills the organism. No significant resistance to penicillin.
- Prevention: Toxoid Vaccine (formaldehyde-treated toxin). Given to children in combination with tetanus toxoid and pertussis vaccine (DTaP).
Listeria monocytogenes
- Causes: Meningitis and sepsis in newborns and immunocompromised adults. Gastroenteritis.
- Habitat: Colonizes the GI and female genital tracts, widespread in animals, plants, and soil.
- Transmission: Across placenta or by contact during delivery. Outbreaks of sepsis in neonates and gastroenteritis are related to ingestion of unpasteurized milk products (e.g., cheese).
- Growth: Grows well at cold temperatures, called "cold enhancement."
- Predisposing factors: Reduced cell-mediated immunity, immunologic immaturity (neonates).
- Prevention: Pregnant women and immunocompromised patients should avoid unpasteurized milk products or raw vegetables. Trimethoprim-sulfamethoxazole can prevent listeriosis.
Clostridium tetani
- Causes: Tetanus, produces exotoxin Tetanus toxin (tetanospasmin).
- Habitat: Soil
- Transmission: Enters through traumatic breaks in the skin.
- Diagnosis: Anaerobic, Gram-positive, spore-forming rods. Spore is at one end ("terminal spore"), giving the organism a "tennis racket" appearance.
- Treatment: Hyperimmune human globulin to neutralize toxin. Penicillin G and spasmolytic drugs (e.g. Valium). No significant resistance to penicillin.
- Prevention: Toxoid vaccine (formaldehyde-treated toxin). Given to children in combination with diphtheria toxoid and pertussis vaccine (DTaP).
Clostridium perfringens
- Causes:
- Gas gangrene: Due to alpha toxin (lecithinase)
- Food poisoning: Due to enterotoxin
- Habitat: Soil and human colon.
- Transmission:
- Gas gangrene: Contamination of wound with soil or feces
- Food poisoning: Ingestion of contaminated food
- Diagnosis: Anaerobic, gram-positive, spore-forming rods.
- Treatment:
- Gas gangrene: Penicillin G plus debridement of wound (no significant resistance to penicillin).
- Food poisoning: Symptomatic treatment.
- Prevention: No vaccine. Extensive debridement of the wound plus administration of penicillin decreases the probability of gas gangrene.
Clostridium botulinum
- Causes: Botulism, due to Botulinum toxin that causes flaccid paralysis.
- Habitat: Soil
- Transmission: Organism and toxin transmitted in improperly preserved food
- Diagnosis: Anaerobic, Gram-positive, spore-forming rods.
- Prevention: Observing proper food preservation techniques, including cooking all home-canned food and discarding bulging cans.
Clostridium difficile
- Causes: Pseudomembranous colitis. Antibiotics disrupt normal flora of colon, leading to C.difficile overgrowth and production of large amounts of exotoxins.
- Habitat: Human colon
- Transmission: Fecal-oral
- Diagnosis: Anaerobic, Gram-positive, spore-forming rods.
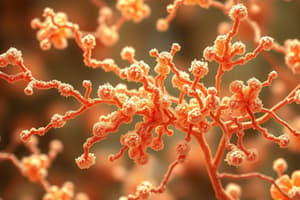
Actinomyces israelii
- Causes: Actinomycosis (abscesses with draining sinus tracts)
- Habitat: Human mouth, especially anaerobic crevices around the teeth.
- Transmission: During dental disease or trauma. Can be aspirated into lungs, causing thoracic actinomycosis. Retained intrauterine device predisposes to pelvic actinomycosis.
- Diagnosis: Anaerobic, Gram-positive filamentous, branching rods.
Nocardia asteroides
- Causes: Nocardiosis (especially lung and brain abscesses)
- Habitat: Soil
- Transmission: Via airborne particles inhaled into the lungs.
- Diagnosis: Aerobic, Gram-positive filamentous, branching rods. Weakly acid-fast.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.