Podcast
Questions and Answers
Which of the following best describes the primary function of bile?
Which of the following best describes the primary function of bile?
- To store glycogen, fats, and vitamins.
- To produce intrinsic factor for vitamin B12 absorption.
- To neutralize stomach acid and emulsify fats for better absorption. (correct)
- To directly digest proteins into amino acids.
The inferior mesenteric artery supplies blood to the foregut.
The inferior mesenteric artery supplies blood to the foregut.
False (B)
Through which vessel does blood from the gastrointestinal tract enter the liver?
Through which vessel does blood from the gastrointestinal tract enter the liver?
portal vein
Bile is composed of bile acids, cholesterol, phospholipids, bile pigments, electrolytes, and ______.
Bile is composed of bile acids, cholesterol, phospholipids, bile pigments, electrolytes, and ______.
Match the following arteries with the region of the gut that they supply:
Match the following arteries with the region of the gut that they supply:
Which of the following is NOT a function of the liver related to nutrient management?
Which of the following is NOT a function of the liver related to nutrient management?
What stimulates bile secretions, increasing the water and bicarbonate ion content of the bile?
What stimulates bile secretions, increasing the water and bicarbonate ion content of the bile?
Name two waste products excreted in bile.
Name two waste products excreted in bile.
Which of the following transport mechanisms is responsible for the absorption of glucose across the apical membrane of enterocytes?
Which of the following transport mechanisms is responsible for the absorption of glucose across the apical membrane of enterocytes?
Chylomicrons enter the bloodstream directly from the enterocytes.
Chylomicrons enter the bloodstream directly from the enterocytes.
What is the primary mechanism by which water absorption occurs in the small intestine?
What is the primary mechanism by which water absorption occurs in the small intestine?
Amino acids are absorbed via a Sodium ________, similar to the absorption of monosaccharides.
Amino acids are absorbed via a Sodium ________, similar to the absorption of monosaccharides.
Match the following molecules with their mode of transport across the enterocyte membrane:
Match the following molecules with their mode of transport across the enterocyte membrane:
Which of the following best describes the role of bile acids in fat absorption?
Which of the following best describes the role of bile acids in fat absorption?
The absorption of both calcium and iron ions is unregulated and occurs regardless of the body's needs.
The absorption of both calcium and iron ions is unregulated and occurs regardless of the body's needs.
Which of the following is the primary function of Kupffer cells within the liver?
Which of the following is the primary function of Kupffer cells within the liver?
What is the function of GLUT2 receptors in carbohydrate absorption?
What is the function of GLUT2 receptors in carbohydrate absorption?
Hepatocytes secrete the bile acid-independent component of bile.
Hepatocytes secrete the bile acid-independent component of bile.
What hormone stimulates the ductal cells to secrete an alkaline solution into the bile ducts?
What hormone stimulates the ductal cells to secrete an alkaline solution into the bile ducts?
The gallbladder concentrates bile by removing water and ______ from it.
The gallbladder concentrates bile by removing water and ______ from it.
Match the following processes with their liver functions:
Match the following processes with their liver functions:
What causes gallstones related to excessive cholesterol?
What causes gallstones related to excessive cholesterol?
A gallstone that blocks the pancreatic duct can lead to what condition?
A gallstone that blocks the pancreatic duct can lead to what condition?
Why can drastic dieting or crash diets lead to the formation of gallstones?
Why can drastic dieting or crash diets lead to the formation of gallstones?
Flashcards
Kidney's Role in Vitamin D
Kidney's Role in Vitamin D
Finalizes Vitamin D activation, promoting bone growth and calcium absorption.
Hepatocyte Detoxification
Hepatocyte Detoxification
Liver cells that convert toxic ammonia to urea for excretion.
Kupffer Cells
Kupffer Cells
Liver macrophages that engulf old blood cells and bacteria.
Bile Acid-Dependent Component
Bile Acid-Dependent Component
Signup and view all the flashcards
Bile Acid-Independent Component
Bile Acid-Independent Component
Signup and view all the flashcards
Gallbladder Function
Gallbladder Function
Signup and view all the flashcards
Gallstones
Gallstones
Signup and view all the flashcards
Enterohepatic Circulation (EHC)
Enterohepatic Circulation (EHC)
Signup and view all the flashcards
Intrinsic Factor
Intrinsic Factor
Signup and view all the flashcards
Main Arteries Supplying the Gut
Main Arteries Supplying the Gut
Signup and view all the flashcards
GIT Regions supplied by arteries
GIT Regions supplied by arteries
Signup and view all the flashcards
Accessory Digestive Organs
Accessory Digestive Organs
Signup and view all the flashcards
Bile Function
Bile Function
Signup and view all the flashcards
What is bile made of?
What is bile made of?
Signup and view all the flashcards
Liver Nutrient Storage
Liver Nutrient Storage
Signup and view all the flashcards
Liver Nutrient Conversion
Liver Nutrient Conversion
Signup and view all the flashcards
Bile Acid Secretion
Bile Acid Secretion
Signup and view all the flashcards
Glucose/Galactose Absorption
Glucose/Galactose Absorption
Signup and view all the flashcards
Fructose Absorption
Fructose Absorption
Signup and view all the flashcards
Amino Acid Absorption
Amino Acid Absorption
Signup and view all the flashcards
Dipeptide/Tripeptide Absorption
Dipeptide/Tripeptide Absorption
Signup and view all the flashcards
Fat Absorption Process
Fat Absorption Process
Signup and view all the flashcards
Water Absorption Mechanism
Water Absorption Mechanism
Signup and view all the flashcards
Calcium Absorption Regulation
Calcium Absorption Regulation
Signup and view all the flashcards
Study Notes
- There are review questions about the intrinsic factor and its role in digestion
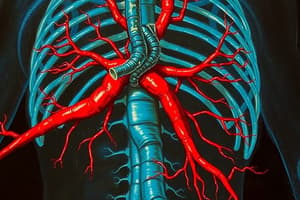
- There are three main trunks/arteries off the descending aorta that supply blood to the guts
- Venous drainage of the abdominal gastrointestinal tract, spleen, pancreas, and gallbladder (except the inferior rectum) use the portal system of veins
- Blood enters the liver from GIT via the portal vein and exits via the hepatic veins to enter the inferior vena cava
Blood Supply to GIT
-
Celiac trunk supplies the foregut, from the stomach to where the bile duct enters the duodenum
-
Important arterial branches of the celiac trunk are:
- Common Hepatic
- Hepatic proper
- Left Hepatic
- Right Hepatic
- Right Gastric
- Gastroduodenal
- Hepatic proper
- Left Gastric
- Splenic
- Common Hepatic
-
The superior mesenteric artery supplies the midgut from where the bile duct enters the duodenum to 2/3 across the transverse colon
-
Relevant arterial branches of the superior mesenteric artery:
- Right colic
- Middle colic
- Ileocolic
- Ileal and jejunal branches
-
Supply occurs via the inferior mesenteric artery to the hindgut (from 2/3 across the transverse colon to the rectum)
-
Arterial branches of the inferior mesenteric artery:
- Left colic
- Sigmoid
- Superior rectal
-
Accessory organs include the liver, pancreas and gall bladder
Liver Functions and Bile Physiology
- Bile consists of bile acids, cholesterol, phospholipids, bile pigments, electrolytes, and water
- Bile serves as a means for eliminating waste products, including bilirubin and cholesterol excesses
- Bile production occurs at 100 mL/day
- Bile salts (bilirubin, biliverdin), cholesterol, fats, fat-soluble hormones, lecithin, neutralize and dilute stomach acid
- Bile salts emulsify fats.
- Most bile salts are reabsorbed in the ileum
- Secretin stimulates bile secretions (increasing water and bicarbonate ion content)
- The liver stores glycogen, fat, vitamins, copper, and iron
- Hepatic portal blood comes to the liver from the small intestine
- The nutrient interconversion process converts amino acids to energy producing compounds and hydroxylates vitamin D
- Vitamin D travels to kidney where it is hydroxylated again into its active form to promotes bone growth and absorption of calcium
- Hepatocytes detoxify removing ammonia and converting it to urea
- Kupffer cells phagocytize worn-out and dying red and white blood cells, and some bacteria
- The liver synthesizes albumins, fibrinogen, globulins, heparin, and clotting factors
- Bile acid-dependent components are produced by hepatocytes, secreted into canaliculi, and transported through the bile ducts
- Bile acid- independent components are made by the ductal cells, these cells secrete alkaline fluid made by pancreatic duct cells which is stimulated by the hormone secretin
- Dependent and independent bile components enter the intrahepatic bile ducts which drain into the biliary tree
- The biliary tree transports bile from the liver to the gallbladder and to the duodenum
- The gallbladder concentrates and stores bile by removing water and ions, regulated by hormone cholecystokinin released from the duodenum
Gall Bladder
- The maximum volume that the gallbladder can hold is 30 to 60ml, but it stores about 450ml
- The gallbladder mucosa absorbs water, sodium, chloride, and other small electrolytes, concentrating the remaining bile components
- Gallstones forms via precipitated cholesterol when excess cholesterol due to high-cholesterol diet and not enough bile salts accumulate
- Gallstones can block the cystic duct and lead to pancreatitis if moving far in the duct
- Gallstones occur because of drastic dieting/fasting as the liver secretes extra cholesterol into bile causing gallstones
Regulation
- Vagus nerve stimulation causes the contraction of the gallbladder
- Secretin stimulates bile secretion by the liver
- Cholecystokinin stimulates contraction of gall bladder
- Bile salts reabsorbed in the ileum stimulate additional bile secretion
Enterohepatic Circulation
- Enterohepatic Circulation (EHC) is the movement of bild acid from the liver to the small intestine and back
Carbohydrate Absorption
- Glucose and galactose absorption occurs via secondary active transport through the Sodium-Glucose co-transporter (SGLT1)
- Glucose and galactose exit the cell via GLUT2 receptors across the basolateral membrane into the blood
- Fructose enters the cell by facilitated diffusion via GLUT5
- Fructose is transported into the blood via GLUT2 receptors
Protein Absorption
- Amino acids are absorbed via a Sodium cotransporter, in a similar mechanism to the monosaccharides
- Transport is across the basolateral membrane via facilitated diffusion
- Di and tripeptides are absorbed via separate H+ dependent cotransporters and are hydrolysed to amino acids within the cell
- Whole protein molecules are absorbed by transcytosis by newborns
Fat Absorption
- The products of digestion are released at the apical membrane and diffuse into the enterocyte
- Inside the cell, the products are re-esterified to form the reassembled lipids, triglycerides, cholesterol and phospholipids.
- The lipids are then packaged inside apoproteins to form a chylomicron
- Chylomicrons are too large to enter circulation, so they enter the lymphatic system via lacteals
Water Absorption
- Most water and electrolyte absorption occurs in the small intestine, with a little absorbed in the colon
- Water absorption depends on solute absorption, such as Na+ and Cl-
- Na+ is absorbed from the intestinal lumen, most use the cotransport with glucose and amino acids and the Na^/H+ exchange
- Water can follow transcellularly or paracellularly (between enterocyte tight junctions)
- Water and Na+ ions diffuse into the capillaries
Absorption of Other Ions
- Calcium is absorbed in the blood especially from the duodenum
- Calcium ion absorption is controlled to body need by parathyroid hormone and vitamin D
- Iron ions are actively absorbed from the small intestine, regulated to body's need for hemoglobin formation
- Actively absorbed through the intestinal mucosa are potassium, magnesium, phosphate,
Vitamins
- Vitamin K, vitamin B12, thiamine, and riboflavin may be found in the colon
- Gases that contribute to flatus in the colon are carbon dioxide, hydrogen gas, and methane
- Vitamin K is important because what you eat doesn't have enough to maintain blood coagulation
- Intrinsic factor is necessary for B12 absorbtion
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Review questions about the intrinsic factor and its role in digestion. Arteries off the descending aorta supply blood to the guts. Venous drainage of the abdominal gastrointestinal tract, spleen, pancreas, and gallbladder use the portal system of veins.