Podcast
Questions and Answers
In a patient presenting with symptoms potentially indicative of gastrointestinal (GI) dysfunction, what is the most critical initial step in differentiating somatic pain from referred pain originating in the GI system?
In a patient presenting with symptoms potentially indicative of gastrointestinal (GI) dysfunction, what is the most critical initial step in differentiating somatic pain from referred pain originating in the GI system?
- Administering a high-dose NSAID trial to assess for pain reduction.
- Initiating immediate referral to a pain management specialist for opioid therapy assessment.
- Performing advanced imaging of the musculoskeletal system (e.g., MRI).
- Conducting a detailed history focusing on bowel habits, dietary changes, and associated GI symptoms. (correct)
A patient reports experiencing arthralgia, a common GI manifestation. Which feature most strongly suggests that the arthralgia is related to an underlying gastrointestinal disorder rather than a primary rheumatological condition?
A patient reports experiencing arthralgia, a common GI manifestation. Which feature most strongly suggests that the arthralgia is related to an underlying gastrointestinal disorder rather than a primary rheumatological condition?
- Co-occurrence with symptoms such as abdominal pain, altered bowel habits, or known GI diagnosis. (correct)
- Persistent morning stiffness lasting longer than one hour.
- Elevated inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- A symmetrical distribution affecting small joints of the hands and feet.
A patient presents with concurrent anorexia, nausea, and vomiting. Which distinguishing factor most strongly suggests that these symptoms are directly related to an elevated intracranial pressure (ICP) rather than a primary gastrointestinal disorder?
A patient presents with concurrent anorexia, nausea, and vomiting. Which distinguishing factor most strongly suggests that these symptoms are directly related to an elevated intracranial pressure (ICP) rather than a primary gastrointestinal disorder?
- Gradual onset of symptoms following dietary indiscretion.
- Symptoms exacerbated by specific food textures or odors.
- Sudden projectile vomiting without preceding nausea. (correct)
- Temporary relief of symptoms with antiemetic medications.
A patient's vomitus is described as having a 'coffee ground' appearance. This signifies the presence of blood that has been exposed to gastric acid. What specific enzymatic reaction is primarily responsible for this change in the blood's appearance?
A patient's vomitus is described as having a 'coffee ground' appearance. This signifies the presence of blood that has been exposed to gastric acid. What specific enzymatic reaction is primarily responsible for this change in the blood's appearance?
A patient with persistent diarrhea is suspected of having a malabsorption syndrome. What stool characteristic is most indicative of steatorrhea, suggesting impaired fat absorption, rather than other causes of diarrhea?
A patient with persistent diarrhea is suspected of having a malabsorption syndrome. What stool characteristic is most indicative of steatorrhea, suggesting impaired fat absorption, rather than other causes of diarrhea?
In the context of gastrointestinal bleeding, which type of blood in the stool is most indicative of a significant bleed originating in the upper digestive tract, such as the stomach or duodenum?
In the context of gastrointestinal bleeding, which type of blood in the stool is most indicative of a significant bleed originating in the upper digestive tract, such as the stomach or duodenum?
A patient reports experiencing excessive gas, including borborygmi. Which pathophysiological mechanism is least likely to contribute directly to the increased production or perception of intestinal gas?
A patient reports experiencing excessive gas, including borborygmi. Which pathophysiological mechanism is least likely to contribute directly to the increased production or perception of intestinal gas?
A patient presents with chronic constipation unresponsive to typical treatments. Which of the following underlying pathophysiological processes is least likely to be a primary contributing factor?
A patient presents with chronic constipation unresponsive to typical treatments. Which of the following underlying pathophysiological processes is least likely to be a primary contributing factor?
A patient describes their abdominal pain as 'colicky'. What underlying mechanism most accurately accounts for the intermittent, wave-like nature of colicky pain?
A patient describes their abdominal pain as 'colicky'. What underlying mechanism most accurately accounts for the intermittent, wave-like nature of colicky pain?
A patient with suspected appendicitis exhibits rebound tenderness in the right lower quadrant. What specific pathophysiological process directly causes the pain associated with rebound tenderness?
A patient with suspected appendicitis exhibits rebound tenderness in the right lower quadrant. What specific pathophysiological process directly causes the pain associated with rebound tenderness?
A patient is diagnosed with malnutrition secondary to chronic gastrointestinal dysfunction. Which laboratory finding is the least reliable indicator of the severity and nature of the malnutrition?
A patient is diagnosed with malnutrition secondary to chronic gastrointestinal dysfunction. Which laboratory finding is the least reliable indicator of the severity and nature of the malnutrition?
A patient reports difficulty swallowing both solids and liquids, with frequent coughing and choking episodes. What underlying etiology should be of the highest concern, warranting immediate investigation?
A patient reports difficulty swallowing both solids and liquids, with frequent coughing and choking episodes. What underlying etiology should be of the highest concern, warranting immediate investigation?
A patient with long-standing gastroesophageal reflux disease (GERD) develops Barrett's esophagus. What cellular change best describes the metaplastic transformation occurring in the esophageal epithelium?
A patient with long-standing gastroesophageal reflux disease (GERD) develops Barrett's esophagus. What cellular change best describes the metaplastic transformation occurring in the esophageal epithelium?
A patient diagnosed with acute gastritis is suspected of having Helicobacter pylori infection. Which diagnostic test provides the most accurate and rapid confirmation of this infection?
A patient diagnosed with acute gastritis is suspected of having Helicobacter pylori infection. Which diagnostic test provides the most accurate and rapid confirmation of this infection?
In a patient with a duodenal ulcer, which pathophysiological mechanism most directly contributes to the characteristic nocturnal pain that awakens them from sleep between midnight and 3:00 AM?
In a patient with a duodenal ulcer, which pathophysiological mechanism most directly contributes to the characteristic nocturnal pain that awakens them from sleep between midnight and 3:00 AM?
A patient being evaluated for possible gastric cancer presents with a palpable left supraclavicular lymph node (Virchow's node). What is the most likely route of metastatic spread causing this clinical finding?
A patient being evaluated for possible gastric cancer presents with a palpable left supraclavicular lymph node (Virchow's node). What is the most likely route of metastatic spread causing this clinical finding?
During an acute episode of pancreatitis, which pathophysiological process is primarily responsible for the development of systemic inflammatory response syndrome (SIRS) and its associated complications?
During an acute episode of pancreatitis, which pathophysiological process is primarily responsible for the development of systemic inflammatory response syndrome (SIRS) and its associated complications?
Following partial pancreatectomy for chronic pancreatitis, a patient develops steatorrhea and diabetes mellitus. What best explains the underlying cause of these complications?
Following partial pancreatectomy for chronic pancreatitis, a patient develops steatorrhea and diabetes mellitus. What best explains the underlying cause of these complications?
A patient with confirmed celiac disease continues to experience symptoms despite strict adherence to a gluten-free diet. Which of the following is the least likely contributing factor to their persistent symptoms?
A patient with confirmed celiac disease continues to experience symptoms despite strict adherence to a gluten-free diet. Which of the following is the least likely contributing factor to their persistent symptoms?
In Crohn's disease, the characteristic 'skip lesions' refer to segments of the intestine that are inflamed, separated by areas of normal tissue. What is the most likely underlying mechanism of this discontinuous pattern of inflammation?
In Crohn's disease, the characteristic 'skip lesions' refer to segments of the intestine that are inflamed, separated by areas of normal tissue. What is the most likely underlying mechanism of this discontinuous pattern of inflammation?
A patient with ulcerative colitis develops toxic megacolon. What specific pathophysiological process most directly leads to the life-threatening colonic dilation observed in this condition?
A patient with ulcerative colitis develops toxic megacolon. What specific pathophysiological process most directly leads to the life-threatening colonic dilation observed in this condition?
A patient with irritable bowel syndrome (IBS) experiences predominant diarrhea. What is the least probable mechanism linking to the heightened visceral sensitivity?
A patient with irritable bowel syndrome (IBS) experiences predominant diarrhea. What is the least probable mechanism linking to the heightened visceral sensitivity?
Following appendectomy for acute appendicitis, a patient develops a persistent fever, abdominal pain, and signs of systemic inflammation. What is the highest concern?
Following appendectomy for acute appendicitis, a patient develops a persistent fever, abdominal pain, and signs of systemic inflammation. What is the highest concern?
A patient with diverticulitis is treated with broad-spectrum antibiotics. What specific component of the gut microbiota is the least important in preventing recurrent diverticulitis episodes?
A patient with diverticulitis is treated with broad-spectrum antibiotics. What specific component of the gut microbiota is the least important in preventing recurrent diverticulitis episodes?
A patient with newly diagnosed colorectal cancer presents with iron deficiency anemia. Which mechanism describes its pathogenesis?
A patient with newly diagnosed colorectal cancer presents with iron deficiency anemia. Which mechanism describes its pathogenesis?
A patient is diagnosed with a small bowel obstruction. What is the most immediate pathophysiological consequence of this complete obstruction on the intestinal wall?
A patient is diagnosed with a small bowel obstruction. What is the most immediate pathophysiological consequence of this complete obstruction on the intestinal wall?
A patient with peritonitis develops septic shock. What is the most critical pathophysiological event leading to hypotension and multi-organ dysfunction?
A patient with peritonitis develops septic shock. What is the most critical pathophysiological event leading to hypotension and multi-organ dysfunction?
A patient with esophageal cancer reports referred pain to the upper back that intensifies with swallowing. What structure explains the pain pathway?
A patient with esophageal cancer reports referred pain to the upper back that intensifies with swallowing. What structure explains the pain pathway?
Which finding is least associated with hiatal hernia?
Which finding is least associated with hiatal hernia?
What medication group is least indicated for GERD?
What medication group is least indicated for GERD?
What is Least likely to result in Acute Gastritis?
What is Least likely to result in Acute Gastritis?
Which of the following can result in damage to the mucosal barrier?
Which of the following can result in damage to the mucosal barrier?
Which is least likely to be a symptom of gastric cancer?
Which is least likely to be a symptom of gastric cancer?
What is least likely to be a potential cause of acute pancreatitis?
What is least likely to be a potential cause of acute pancreatitis?
Which is not associated with signs and symptoms of chronic pancreatitis?
Which is not associated with signs and symptoms of chronic pancreatitis?
What can Celiac Disease prevent?
What can Celiac Disease prevent?
What is least likely to be associated with Crohn's Disease?
What is least likely to be associated with Crohn's Disease?
What is least likely to be a shared clinical feature between crohn's and ulcerative colitis?
What is least likely to be a shared clinical feature between crohn's and ulcerative colitis?
IBS can be not associated with:
IBS can be not associated with:
What is not a typical sign/symptom of appendicitis?
What is not a typical sign/symptom of appendicitis?
Which of the options is least typical of diverticular disease?
Which of the options is least typical of diverticular disease?
What is least associated with colorectal cancer?
What is least associated with colorectal cancer?
What is least linked to intestinal obstruction?
What is least linked to intestinal obstruction?
Flashcards
Psychoneuroimmunology
Psychoneuroimmunology
The relationship between the enteric system, immune system, and brain.
Referred pain from GI issues
Referred pain from GI issues
GI disorders can cause pain in regions that mimic musculoskeletal issues.
Arthritis & Crohn's disease
Arthritis & Crohn's disease
Arthritis and migratory arthralgias occur in this percentage of patients with Crohn's disease.
Anorexia, Nausea, Vomiting
Anorexia, Nausea, Vomiting
Signup and view all the flashcards
Nausea
Nausea
Signup and view all the flashcards
Vomiting
Vomiting
Signup and view all the flashcards
Hematemesis
Hematemesis
Signup and view all the flashcards
Diarrhea
Diarrhea
Signup and view all the flashcards
Large-volume diarrhea
Large-volume diarrhea
Signup and view all the flashcards
Small-volume diarrhea
Small-volume diarrhea
Signup and view all the flashcards
Steatorrhea
Steatorrhea
Signup and view all the flashcards
Blood in Stool
Blood in Stool
Signup and view all the flashcards
Gas
Gas
Signup and view all the flashcards
Causes of Constipation
Causes of Constipation
Signup and view all the flashcards
Visceral Pain
Visceral Pain
Signup and view all the flashcards
Somatic Pain
Somatic Pain
Signup and view all the flashcards
Limited Malnutrition
Limited Malnutrition
Signup and view all the flashcards
Generalised Malnutrition
Generalised Malnutrition
Signup and view all the flashcards
Dysphagia
Dysphagia
Signup and view all the flashcards
Hiatal Hernia
Hiatal Hernia
Signup and view all the flashcards
GERD
GERD
Signup and view all the flashcards
Acute Gastritis
Acute Gastritis
Signup and view all the flashcards
Peptic Ulcer
Peptic Ulcer
Signup and view all the flashcards
Gastric (Stomach) Cancer
Gastric (Stomach) Cancer
Signup and view all the flashcards
Acute Pancreatitis
Acute Pancreatitis
Signup and view all the flashcards
Pancreatitis
Pancreatitis
Signup and view all the flashcards
Acute Pancreatitis: Symptoms
Acute Pancreatitis: Symptoms
Signup and view all the flashcards
Chronic Pancreatitis: Symptoms
Chronic Pancreatitis: Symptoms
Signup and view all the flashcards
Pancreatic Cancer: Symptoms
Pancreatic Cancer: Symptoms
Signup and view all the flashcards
Celiac Disease
Celiac Disease
Signup and view all the flashcards
Celiac Disease: Manifestation
Celiac Disease: Manifestation
Signup and view all the flashcards
Inflammatory Bowel Diseases
Inflammatory Bowel Diseases
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Shared Clinical Features
Shared Clinical Features
Signup and view all the flashcards
Bowel Syndrome
Bowel Syndrome
Signup and view all the flashcards
Bowel Manifestations
Bowel Manifestations
Signup and view all the flashcards
Appendicitis
Appendicitis
Signup and view all the flashcards
Diverticulitis
Diverticulitis
Signup and view all the flashcards
Study Notes
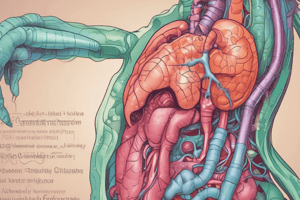
Objectives
- The presentation is to review key signs and symptoms of gastrointestinal (GI) and hepatobiliary dysfunction.
- It will discuss common GI and hepatobiliary pathologies that may mimic somatic pain.
Psychoneuroimmunology
- There is a relationship between the enteric system, the immune system, and the brain.
- Two-thirds of all immune activity occurs in the gut.
- This concept relates to disorders like fibromyalgia, SLE, RA, and chronic fatigue syndrome (CFS).
GI Disorders and Referred/Mimicked Pain
- GI disorders can cause referred pain in several regions, mimicking musculoskeletal (MSK) issues.
- Regions of referred pain include the sternum, neck, shoulder, scapula, low back, sacrum, groin, and hip.
- GI conditions can cause referred pain to the back and shoulder, such as upper back pain.
- Arthritis and migratory arthralgias occur in approximately 25% of patients with Crohn’s disease.
- Appendicitis, Crohn’s disease, and ulcerative colitis can cause iliopsoas muscle abscesses, leading to hip, thigh, or groin pain.
- Antibiotics and NSAIDs are medications can induce GI symptoms.
GI Manifestations
- Common GI manifestations include abdominal pain, dysphagia, odynophagia and GI bleeding.
- GI bleeding can present as emesis or melena.
- Further GI manifestations are altered eating habits, including anorexia, nausea, and vomiting.
- GI disorders can present as arthralgia, neurologic disorders and early satiety with weight loss.
- Other GI manifestations include constipation, diarrhea, fecal incontinence, referred shoulder pain, and epigastric pain that radiates to the back.
Anorexia, Nausea, and Vomiting
- Anorexia, nausea, and vomiting can be signs of a GI disorder or other conditions.
- Other potential origins are systemic infections, uremia and emotional responses.
- Further causes are motion sickness, elevated ICP, overindulgence of food or drugs, and pain.
- Anorexia and vomiting can have serious complications, including dehydration, acidosis, and malnutrition.
- Nausea is an unpleasant subjective feeling stimulated by distention, irritation, and inflammation of the digestive tract, as well as smells, visual images, pain, and chemical toxins or drugs.
- Vomiting may be triggered by distention or irritation in the digestive tract and stimuli from various parts of the brain.
- Vomiting is induced by unpleasant sights or smells, ischemia, pain or stress, vestibular issues, and increased intracranial pressure. Projectile vomiting without preceding nausea may also prompt the vomiting reflex.
- Stimulation of the chemoreceptor trigger zone and drugs, toxins, and chemicals can induce vomiting.
Characteristics of Vomitus
- Presence of blood in vomit, known as hematemesis, can indicate coffee ground vomitus.
- Brown granular material indicates the action of HCl on hemoglobin, and hemorrhage indicates that red blood may be present in the vomit.
- Yellow or green-stained vomitus are caused by bile from the duodenum.
- Deep brown vomit indicates content from the lower intestine.
- Recurrent vomiting of undigested food indicates a problem with gastric emptying or infection.
Diarrhea
- Diarrhea features excessive frequency of stools, usually with loose or watery consistency
- Diarrhea may be acute or chronic and accompanied by nausea and vomiting when infection or inflammation develops.
- Cramping pain can occur during a bout of diarrhea.
- Prolonged diarrhea may lead to dehydration, electrolyte imbalance, acidosis, and malnutrition.
Common Types of Diarrhea
- Large-volume diarrhea can be secretory or osmotic.
- The stool is watery resulting from secretions into the intestine from the plasma and is often related to infection.
- Small-volume diarrhea is often caused by inflammatory bowel disease.
- Stool may contain blood, mucus, or pus and may be accompanied by abdominal cramps.
- Steatorrhea involves frequent bulky, greasy, loose stools with a foul odor and is characteristic of malabsorption syndromes like celiac disease and cystic fibrosis.
- With steatorrhea, fat is usually the first dietary component affected, interferes with the digestion of other nutrients, and the abdomen is often distended.
Blood in Stool
- Blood may occur in normal stools, diarrhea, constipation, tumors, or inflammatory conditions.
- Frank blood originates usually from lesions in rectum or anal canal-
- Occult blood are small hidden amounts detectable with a stool test and may be caused by small bleeding ulcers.
- Melena causes stool that is dark-colored and tarry.
- It may result from significant bleeding in the upper digestive tract.
Gas
- Gas develops normally due to swallowed air, bacterial action on food, certain foods, or alterations in motility.
- Excessive gas may manifest as eructation, borborygmus, abdominal distention and pain, and flatulence.
Constipation
- Constipation is a condition of less frequent bowel movements than normal.
- Characterized by small, hard stools, the causative problem is acute or chronic.
- It may be caused by decreased peristalsis.
- Periods of constipation may alternate with periods of diarrhea.
- Chronic constipation may cause hemorrhoids, anal fissures, or diverticulitis.
Causes of Constipation
- Constipation can be triggered by weakness of smooth muscle, inadequate dietary fiber and/or fluid intake.
- Ignoring the defecation reflex, Immobility and neurological disorders can result in constipation.
- Certain Medications (opiates, antacids, and iron supplements) as well as obstructions caused by tumors or strictures may also result in constipation.
Pain: Visceral Pain Characteristics
- Visceral pain creates a burning sensation and may occur with inflammation and ulceration in the GI tract.
- Patients experience a dull, aching pain due to stretching of liver capsule.
- Cramping or diffuse pain occurs with inflammation, distention, and stretching of the intestines.
- Colicky pain features sharp spasms that are wave-like and often severe.
- Colicky pain starts and stops quickly due to intermittent contractions and can occur in response to severe inflammation or obstruction.
Pain: Somatic Pain
- Somatic pain receptors are directly linked to spinal nerves.
- Causes reflex spasm of overlying abdominal muscles.
- Stays steady, intense, and well-localized to a specific abdominal area.
- Arises from Involvemen or inflammation of the parietal peritoneum.
- Rebound tenderness occurs over the specified area of inflammation and intensifying when pressure is released -- appendicitis is an example.
Malnutrition
- Malnutrition may be limited to a specific nutrient or generalized deficiency.
- Limited malnutrition can be Vitamin B12 or iron deficiency related.
- Generalized malnutrition stems from systemic conditions.
- It occurs due to chronic anorexia, vomiting, and diarrhea, stemming from causes such as chronic inflammatory bowel disorders and cancer treatments.
Dysphagia
- Dysphagia is difficulty swallowing.
- Presentation involves pain with swallowing (odynophagia).
- Can arise from the inability to swallow larger pieces of solid material and difficulty swallowing liquids in general.
- May trigger choking and coughing with the attempt to shallow.
- Related to a Neurological deficit, Muscular disorder or Mechanical obstruction.
- Neurological deficits are related to stroke or TBI issues.
- Muscular disorder may be secondary to trauma or Commonly occurs following anterior cervical fusions.
- With mechanical obstruction stenosis (narrowing of the esophagus) is developmental or acquired in nature.
Esophageal Cancer
- Esophageal cancer usually originates in distal esophagus.
- Significant dysphagia occurs in later stages and presents with the patient reporting upper back pain.
- Swallowing food may worsen symptoms.
- Poor prognosis due to late manifestations.
- Often associated with chronic irritation related to chronic esophagitis, Achalasia or Hiatal hernia.
- Can come about from Alcohol abuse and/or smoking.
Hiatal Hernia
- Part of the stomach protrudes into the thoracic cavity.
- Food may lodge in pouch of the hernia.
- Causes inflammation of the mucosa, reflux of food up the esophagus and chronic esophagitis. Signs include heartburn, constant belching and increased discomfort when lying down.
- Patients may have substernal pain that may radiate to shoulder and jaw
Gastroesophageal Reflux Disease (GERD)
- Periodic reflux of gastric contents into distal esophagus causes erosion and inflammation.
- Often occurs with hiatal hernia.
- Increased symptoms when laying down, especially after eating.
- Avoid consumption of caffeine, fatty and spicy foods and alcohol, smoking, certain drugs to reduce symptoms.
- Use of medication assists in reducing reflux & inflammation.
- Patients may experience symptoms in the form of atypical MI symptoms.
Gastritis: Acute Gastritis
- Gastric mucosa is inflamed, possibly ulcerated and bleeding.
- Caused by infection by microorganisms, allergies to foods, irritating foods and excessive alcohol intake.
- Originates with the ingestion of aspirin, other NSAIDs or corrosive/toxic substances as well as radiation or chemotherapy.
- Basic signs of GI irritation are anorexia, nausea, vomiting and Hematemesis caused by bleeding.
- Patients may experience Epigastric pain, cramps or general discomfort with infection and diarrhea.
- Acute gastritis is usually self-limiting.
Peptic Ulcer: Gastric and Duodenal Ulcers
- Most commonly originates from H. pylori infection, and is associated with proximal duodenum
- Patients experience ulcers due to breakdown of - mucosal barrier.
- Decreased mucosal defense is more common in gastric ulcer development, where increased acid secretion is a predominant factor in duodenal ulcers.
Gastric and Duodenal Ulcers
- Damage to mucosal barrier is associated with Inadequate blood supply due to vasoconstriction.
- Stress, smoking, shock, circulatory impairment and rapid regeneration of epithelium can also cause ulcer formations.
- Excessive glucocorticoid secretion or medications and ulcerogenic substances (Aspirin, NSAIDs, alcohol) that break down mucous occur as well.
Complications of Ulcers
- Hemorrhage is relatively common because erosion of blood vessels.
- It may be the first sign.
- Perforation occurs as the ulcer erodes completely through the wall.
- Chyme can enter the peritoneal cavity, resulting in chemical peritonitis.
- Obstruction results from increased scar tissue at the ulcer site.
Ulcer Symptoms
- "Heartburn" or epigastric pain as well as Aggravation by food.
- With duodenal ulcer, patients experience night pain in a time range from midnight to 3:00 AM. Patients may also Radiating back and/or right shoulder pain with the usual complaints such as nausea or anorexia and passing blood in stool.
Gastric (Stomach) Cancer
- Most patients are asymptomatic in early stages.
- Leading to late diagnosis and poor prognosis.
- Risk stems from Genetic predisposition, H/o pernicious anemia, eating too much smoked foods, nitrites etc.
- Other Signs/symptoms include Epigastric pain and weight loss.
- Patient report Dysphagia, and an Iron deficiency stems to Hematemesis or melena.
- May develop palpable mass on the left supraclavicular lymph node
Acute Pancreatitis
- Pancreatitis is medical emergency because the pancreas lacks fibrous capsules, in response Destructive actions may progress to surrounding tissues.
- Substances released by necrotic tissues release inflammatory compounds resulting in Hypovolemia and circulatory collapse
- Chemical peritonitis results in bacterial peritonitis, potentially leades to Adult respiratory distress syndrome and acute renal failure.
- Potential causes includes Gallstones, Alcohol abuse and Sudden onset by taking too much fat or alcohol food
Causes of Acute Pancreatitis Symptoms
- Primary symptoms are Severe epigastric pain radiating to the back.
- Low-grade fever may present until infection develops, in which a High temp is present.
- Abdominal distention may happen and create decreased bowel sounds, as a result of Decreased peristalsis and paralytic ileus.
- Signs of shock may occur originating from Hypovolemia
Symptoms of Chronic Pancreatitis
- Patients experience recurring Epigastric pain radiating to the back and Upper left as well asLumbar pain.
- Can also cause Nausea, vomiting, Weight loss and Oily/fatty and Clay stool.
Pancreatic Cancer
- It is typically asymptomatic until well advanced.
- risk includes smoking, Obesity and Liver cirrhosis due to Chronic pancreatitis.
- Symptoms includes Epigastric and back pain with Jaundice and anorexia and weight loss
- Other symptoms involve Light-colored stools, and constipation.
Celiac Disease
- A malabsorption syndrome with A genetic link and Primarily diagnosed in childhood.
- Manifestation may occur later in an adults
- It occurs because of Defect in Intestinal enzyme where Patients have difficulty when adding cereals to their diet.
- First signs typically appear at about 4 - 6 months of age.
- Prevents the full digestion of gliadin, damaging the intestinal villi and resulting in and Malnutrition
Manifestations of Celiac Disease
- Can occur Steatorrhea along with Muscle wasting which create Failure to gain weight.
- Other symptoms are Irritability and malaise.
- Diagnosis requires Diagnosis from sample tissue and various blood tests.
Chronic Inflammatory Bowel Disease (IBD)
- Major condition are Crohn’s disease and Ulcerative colitis, all due to an Autoimmune defect.
- IBD manifests as skin, eye and joint symptoms and displays similar symptoms.
Crohn’s Disease
- Any part can get affected but the digestive tract is more prevalent because of the inflammation.
- Patients report skip lesions where Affected areas separated by areas of normal tissue.
- This can be a result of Damage inhibiting Processing a lack of adequate nutrition.
- Can develop Progressive inflammation that can affect the motility and cause restricted areas.
- With this lack of digestion, leads to Hypoproteinemia, avitaminosis, malnutrition,, ad possibly to steatorrhea.
- Complications are Adhesions of loops to develop and fistulas.
- Children experience Delayed in maturation and sexual development.
Ulcerative Colitis
- Inflammation starts in the rectum and Progresses through the colon resulting in extreme symptoms (toxic megacolon)
- Can results in frequent passing of mucus and painful cramps of up to 12 times a day.
- Mucosa and submucosa becomes inflamed, due to decreased Electrolyte fluid
What Crohn’s and Ulcerative Colitis Have in Common
- Diarrhea and Constipation with a Fever, leading to Abdominal pain when Rectal (anal passage) Bleeding during their Night sweats.
- Due to this their Bodies decrease in weight .
- Skin becomes dry, Uveitis which creates in the The irritation of both eyes.
Irritable Bowel Syndrome (IBS)
- Occurs with a abnormal Inflammatory reaction.
- Can develops Gastrointestinal trouble and Visceral (internal hypersensitivity).
- Other infections are Overgrowth bacteria infection, Food poisoning resulting from the infection as well as Physiciatric disturbance.
IBS: Manifestations and Diagnosis
- Results in Lower abdominal pain, Diarrhea and Constipation in alternating order.
- Bloating that creates low back pain; especially if constipation is present.
Anorexia symptoms
General pain begins in the Upper part of the Naval and Vomiting.
- Pain creates serious pain that travels to the Lower Right of the Body or pain in the thigh, groin, or testicle
- Diagnosis requires Positive hop test and a sign of Dysuria
Appendicitis Progression
- After rupture, Pain temporarily subsides which makes for pain. The patient may indicate a generalized Severe pain and guarding resulting in a fever and inflammation . Patients report a Rigid abdomen which is detected by the development of perotonits and abdominal issues that cause reduced blood pressure
Diverticular Disease
- When a layer of tissue pushes the layer of the colon.
- This is known as hernia action.
- When this hernia action causes Asymptomatic movement.
- It also leads to inflammation creating Diverticulitics.
- This process is caused to gaps being created where Weak points exists.
- At times there are no symptoms, however, the patient does express Infection.
Diverticulitis Symptoms
- Discomfort, pain and elevated levels and causes Lower pain and uneasiness.
Symptoms of Collorectal
- Early identification is key as Collorectal patients occur primarily in the in a persons later years, due to Gene transfers that develop from Familial history and from ulcerative . Can derive from genetics where family can inherit the cancer or the patient consumes food without fiber
Collorectal General Complications
- Changes depends on the Initial diagnosis with symptoms consisting of Changes relating to diarrhea,
- Patients experience Fatigue, weight loss and anemia.
- Early signs consists of hemorrhoids .
- Other sensations consist of Abdominal and hip pain, and back sensation.
Late and Serious Complications of Collorectal Cancer
- Constipation results in a restricted movement and discharge.
- Patients endure Nausea which causes a drastic Reduction in body bulk.
- Fever is a less common trait.
- In general patients endure tiredness as well as hard and heavy respiration
Intestinal Obstruction
- Absence in motion leads to intestine restriction.
- Its typically stems from adhesions, a hernia to a tumour in the body.
- Problems with the intestines movement or non-movement
Intestinal Obstruction Complications
- An over amount of fluids can distend the body during obstruction, this increases stress and force.
- Body try's to eject substances to the colon which can lead to an electrolyte imbalance.
- Blood walls can constrict.
- Body can cause intestinal swelling which can lead to peritonitis ( bacterial production).
- Intestinal wall becomes necrotic causing bacteria and toxins to spill into the nearby spaces in the abdomen this leads to infection called septicemia.
More Obstruction complications
- Can lead to surgery abdominal injury which requires a high dose of spinal anesthesia.
- Results from high exposure of radiation or infection of the kidneys can result with a SCI.
- Caused from hernia, tissue tears or tumors as well.
- Conditions such as Crohn can cause this effect.
Specific Intestional Obstrucion Complications
- Can lead to small intestines damage, due to colicky pains that result in an inconsistent bowel action that gets worst during Bile discharge.
- When body fails it fails into hypovolemia
Peritonitis (tissue tearing)
- This condition may develop as enzymes leak out from the intestines which is caused from enlargement or perforated section of the intestines to rupture.
- This will result from other foreign complications or factors that causes an Rupture.
Causes of Peritonitis
- Starts bacterial effects that damage from Trauma, A ruptured appendix.
- If non-natural agents comes in contact with abdominal fluids, or the Infection can also creates issues that results with the fall of the Ovaries which gets infected by fallopian tubes.
Results of Tissue Tear (Peritonitis) Complications
- Severe abdominal aches with continuous and ongoing pain
- Results In reduced of body pressure due to blood loss and fever or a high heart rate
- Patients start passing pus/ or yellow discharge and creates a form of swelling near the body.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.