Podcast
Questions and Answers
What is a common consequence of severe inflammatory bowel disease such as Crohn's disease?
What is a common consequence of severe inflammatory bowel disease such as Crohn's disease?
- Increased appetite
- Improved digestion
- Weight gain
- Nutritional malabsorption (correct)
What characterizes the physical presentation of a child with gastroschisis?
What characterizes the physical presentation of a child with gastroschisis?
- Visible bowel on the outside of the baby (correct)
- Abdominal mass resembling a sausage shape
- Intestinal perforation resulting from necrosis
- Presence of a sac covering the abdominal contents
Which treatment is used for managing ulcerative colitis to induce remission?
Which treatment is used for managing ulcerative colitis to induce remission?
- Antibiotics
- Corticosteroids (correct)
- Probiotics
- Surgical intervention
What clinical manifestation is predominantly associated with Meckel's diverticulum?
What clinical manifestation is predominantly associated with Meckel's diverticulum?
Which symptom is indicative of intussusception in a child?
Which symptom is indicative of intussusception in a child?
What complication is most ominous in Hirschsprung disease?
What complication is most ominous in Hirschsprung disease?
Which of the following is a potential extraintestinal manifestation of Crohn's disease?
Which of the following is a potential extraintestinal manifestation of Crohn's disease?
Which of these is a significant nursing consideration for patients experiencing nutritional imbalances due to inflammatory bowel disease?
Which of these is a significant nursing consideration for patients experiencing nutritional imbalances due to inflammatory bowel disease?
What occurs during the volvulus condition?
What occurs during the volvulus condition?
What is the most common congenital malformation of the gastrointestinal tract?
What is the most common congenital malformation of the gastrointestinal tract?
Hirschsprung disease is primarily caused by what physiological defect?
Hirschsprung disease is primarily caused by what physiological defect?
Which symptom is least likely to be associated with a ruptured appendix?
Which symptom is least likely to be associated with a ruptured appendix?
What is a common initial symptom of gastroschisis in newborns?
What is a common initial symptom of gastroschisis in newborns?
Which of the following is NOT a symptom associated with intussusception?
Which of the following is NOT a symptom associated with intussusception?
Which of the following is NOT a clinical manifestation of ulcerative colitis?
Which of the following is NOT a clinical manifestation of ulcerative colitis?
Which factor is least likely to contribute to infantile colic in infants?
Which factor is least likely to contribute to infantile colic in infants?
What is the primary concern related to nutritional imbalances in infants?
What is the primary concern related to nutritional imbalances in infants?
What is a primary treatment performed for a child diagnosed with gastroschisis?
What is a primary treatment performed for a child diagnosed with gastroschisis?
Which of the following interventions is most appropriate for managing nutritional imbalances in infants with colic?
Which of the following interventions is most appropriate for managing nutritional imbalances in infants with colic?
Which condition is often associated with failure to thrive in the context of infant nutritional imbalances?
Which condition is often associated with failure to thrive in the context of infant nutritional imbalances?
What symptom might indicate a nutritional imbalance leading to colic in infants?
What symptom might indicate a nutritional imbalance leading to colic in infants?
How does increased peristalsis in newborns affect their nutritional absorption?
How does increased peristalsis in newborns affect their nutritional absorption?
Which of the following might be a dietary recommendation to prevent infant colic related to nutritional imbalances?
Which of the following might be a dietary recommendation to prevent infant colic related to nutritional imbalances?
What is the most common nutritional issue faced by newborns related to digestive capability?
What is the most common nutritional issue faced by newborns related to digestive capability?
What should be assessed in a newborn if the first meconium is not passed within 24 to 36 hours?
What should be assessed in a newborn if the first meconium is not passed within 24 to 36 hours?
Which structural defect may result in a complete obstruction of the esophagus?
Which structural defect may result in a complete obstruction of the esophagus?
What is the primary concern related to the enzyme deficiencies present in newborns?
What is the primary concern related to the enzyme deficiencies present in newborns?
What type of surgical procedure is most commonly performed to minimize scarring after cleft lip correction?
What type of surgical procedure is most commonly performed to minimize scarring after cleft lip correction?
Which of the following conditions is least likely to directly contribute to failure to thrive in infants?
Which of the following conditions is least likely to directly contribute to failure to thrive in infants?
What is the primary age range recommended for surgical correction of cleft palate?
What is the primary age range recommended for surgical correction of cleft palate?
What is the primary purpose of elbow restraints in post-operative care for cleft palate repair?
What is the primary purpose of elbow restraints in post-operative care for cleft palate repair?
What feeding equipment is designed specifically to assist children with cleft palate during bottle feeding?
What feeding equipment is designed specifically to assist children with cleft palate during bottle feeding?
What is a potential complication of esophageal atresia in infants?
What is a potential complication of esophageal atresia in infants?
What is one important consideration when managing feeding for infants affected by cleft lip and palate?
What is one important consideration when managing feeding for infants affected by cleft lip and palate?
Which of the following statements about newborns' gastrointestinal functions is accurate?
Which of the following statements about newborns' gastrointestinal functions is accurate?
What is the primary defect associated with esophageal atresia in infants?
What is the primary defect associated with esophageal atresia in infants?
Which of the following conditions may be indicated if a newborn does not pass their first meconium within 24 to 36 hours?
Which of the following conditions may be indicated if a newborn does not pass their first meconium within 24 to 36 hours?
What is a significant risk associated with cleft lip and palate deformities in infants?
What is a significant risk associated with cleft lip and palate deformities in infants?
What surgical technique is commonly performed to address cleft lip repair?
What surgical technique is commonly performed to address cleft lip repair?
What is the primary impact of surgical correction of cleft palate on a child's development?
What is the primary impact of surgical correction of cleft palate on a child's development?
Which intervention is crucial for feeding infants with cleft palate?
Which intervention is crucial for feeding infants with cleft palate?
What nursing consideration is most important after cleft palate surgery?
What nursing consideration is most important after cleft palate surgery?
What age range is typically recommended for performing surgical correction of cleft palate?
What age range is typically recommended for performing surgical correction of cleft palate?
What is the significance of using elbow restraints for a child post-cleft palate surgery?
What is the significance of using elbow restraints for a child post-cleft palate surgery?
Flashcards
GI system function
GI system function
Digests food, absorbs nutrients, and eliminates waste.
Newborn GI differences
Newborn GI differences
Newborns have weaker swallowing, faster gut movements, and might have trouble processing certain nutrients.
Meconium passage delay
Meconium passage delay
Meconium (newborn stool) should usually be passed within 24-36 hours of birth. Delayed passage warrants investigation for conditions like Hirschsprung disease or hypothyroidism.
Infant colic
Infant colic
Signup and view all the flashcards
Cleft lip/palate
Cleft lip/palate
Signup and view all the flashcards
Esophageal atresia
Esophageal atresia
Signup and view all the flashcards
Pyloric stenosis
Pyloric stenosis
Signup and view all the flashcards
Gastroesophageal reflux
Gastroesophageal reflux
Signup and view all the flashcards
Omphalocele
Omphalocele
Signup and view all the flashcards
Gastroschisis
Gastroschisis
Signup and view all the flashcards
Intussusception
Intussusception
Signup and view all the flashcards
Volvulus
Volvulus
Signup and view all the flashcards
Hirschsprung disease
Hirschsprung disease
Signup and view all the flashcards
Anorectal malformations
Anorectal malformations
Signup and view all the flashcards
Intestinal perforation
Intestinal perforation
Signup and view all the flashcards
Enterocolitis
Enterocolitis
Signup and view all the flashcards
Ruptured appendix signs
Ruptured appendix signs
Signup and view all the flashcards
Meckel's Diverticulum
Meckel's Diverticulum
Signup and view all the flashcards
Ulcerative Colitis (UC)
Ulcerative Colitis (UC)
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Pain in 10-year-old boy
Pain in 10-year-old boy
Signup and view all the flashcards
Congenital GI Tract Malformation
Congenital GI Tract Malformation
Signup and view all the flashcards
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD)
Signup and view all the flashcards
Pain Management in Children
Pain Management in Children
Signup and view all the flashcards
Meconium Delay
Meconium Delay
Signup and view all the flashcards
Cleft Palate Repair: When?
Cleft Palate Repair: When?
Signup and view all the flashcards
Cleft Palate Repair: Why?
Cleft Palate Repair: Why?
Signup and view all the flashcards
Cleft Palate Repair: Elbow Restraints
Cleft Palate Repair: Elbow Restraints
Signup and view all the flashcards
Special Needs Feeder
Special Needs Feeder
Signup and view all the flashcards
Cleft Lip/Palate Feeding Issues
Cleft Lip/Palate Feeding Issues
Signup and view all the flashcards
Elbow Restraints
Elbow Restraints
Signup and view all the flashcards
Cleft Palate Repair: Age
Cleft Palate Repair: Age
Signup and view all the flashcards
Cleft Palate Repair: Goal
Cleft Palate Repair: Goal
Signup and view all the flashcards
Cleft Lip/Palate Feeding
Cleft Lip/Palate Feeding
Signup and view all the flashcards
Study Notes
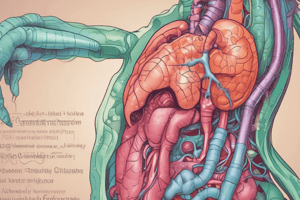
Gastrointestinal Dysfunction in Children
- The gastrointestinal (GI) system is responsible for absorbing and digesting food and fluids, and eliminating waste.
- Key organs of the GI system include the esophagus, stomach, pancreas, large and small intestines, gallbladder, and liver.
- Infants have smaller stomach capacities than older children or adolescents.
- Stomach capacity increases with age. A 30-day-old infant has a stomach capacity of 90 ml, and an adult stomach holds 2-3 liters.
Pediatric Differences
- Newborns have poor swallowing control and increased peristalsis.
- Newborns may have limited enzyme function, impacting bilirubin conjugation, gluconeogenesis, deamination, plasma protein, and ketone formation.
Newborn Period
- Meconium should be passed within 24-36 hours of birth.
- Conditions to assess for if meconium is not passed include Hirschsprung disease and hypothyroidism, meconium plug, or meconium ileus (CF).
GI Problems in Infancy
- Nutritional imbalances
- Colic
- Food sensitivities
- Failure to thrive
Structural Defects
- Head: Cleft lip and cleft palate
- Esophagus and Stomach: Esophageal atresia, tracheoesophageal fistula, pyloric stenosis, gastroesophageal reflux
- Intestines: Omphalocele, gastroschisis, intussusception, volvulus, Hirschsprung disease
- Anus: Anorectal malformations, ostomies
Cleft Lip/Cleft Palate
- Facial malformations occurring during embryonic development.
- Can appear separately or together.
- Etiology (cause) and pathophysiology (how it works) should be studied.
- Diagnostic evaluation is also a key part of the process.
Surgical Correction of Cleft Lip/Palate
- Lip repair typically precedes palate repair.
- Surgeons use Z-plasty to help reduce scar retraction.
- Cleft palate repair is typically done at 6-18 months of age.
Cleft Lip/Palate Feeding
- Issues and interventions regarding feeding are important to note.
- Special feeding equipment, such as modified nipples, may be needed.
- Breastfeeding issues may also need to be addressed.
Question 1 (Rationale for Elbow Restraints)
- Elbow restraints are used postoperatively to prevent children from touching the surgical site for healing.
Question 9 (Rationale for Child's Statement)
- The child may have difficulty communicating pain effectively or might be apprehensive about surgery. A ruptured appendix would cause different symptoms.
Pathophysiology of Esophageal Atresia and Tracheoesophageal Fistula
- In the common type, the upper esophagus ends in a blind pouch connected to the trachea. A fistula connects the lower esophagus to the trachea.
Hypertrophic Pyloric Stenosis
- A constriction of the pyloric sphincter preventing passage of stomach contents.
- Key signs include projectile vomiting, dehydration, and a palpable olive-shaped mass.
- Treatment usually involves surgical correction.
Gastroesophageal Reflux (GER)
- The transfer of gastric contents into the esophagus.
- GER becomes abnormal when frequent and severe.
- Symptoms in infants can include spitting up, forceful vomiting, and excessive crying. In children, it may manifest as heartburn, abdominal pain, difficulty swallowing, and chronic cough.
Inflammatory Disorders
- Appendicitis, Necrotizing Enterocolitis (NEC), Meckel's Diverticulum, Inflammatory Bowel Disease (Crohn's disease and ulcerative colitis), Peptic Ulcer, and acute diarrhea
- Each condition has unique symptoms and treatments.
Inflammatory Disorders: Appendicitis
- Earliest symptoms: periumbilical pain and vomiting; later right-lower quadrant pain.
- Important diagnostic differentiator: children who are hungry likely do not have appendicitis.
Inflammatory Disorders: Meckel's Diverticulum
- Congenital malformation of the GI tract.
- Common symptoms include rectal bleeding and abdominal discomfort.
Inflammatory Disorders: Ulcerative Colitis
- Inflammation within the colon and rectum.
- Symptoms include ulceration, bleeding, anorexia and anemia.
Inflammatory Disorders: Crohn's Disease
- Inflammatory bowel disease (IBD) affecting any part of the GI tract.
- Symptoms include abdominal pain, severe diarrhea, and malabsorption.
Inflammatory Disorders: Peptic Ulcer
- Loss of mucosal, submucosal and muscular layer.
- Key symptoms should be studied; treatment may involve medical and surgical interventions.
Disorders of Motility:
- Gastroenteritis (Acute Diarrhea)
- Constipation
- Encopresis
Disorders of Motility: Gastroenteritis/Acute Diarrhea
- Leading cause of illness in young children.
- Factors to consider include infection prevention measures, such as hand-washing and water supply precautions
- Complications include dehydration.
Intestinal Parasitic Disorders
- Common triggers for intestinal parasitic infection include camping, drinking contaminated water and exposure to pets or wildlife.
- The condition is treated using antihelmintic medications.
Dehydration
- Dehydration occurs in various forms, such as isotonic, hypotonic, and hypertonic.
- Diagnosing and treating dehydration requires appropriate assessment and rehydration strategies.
Malabsorption Disorders
- Celiac disease, lactose intolerance, and short bowel syndrome
- Each condition results in an inability to absorb certain nutrients or food properly.
- Dietary restrictions and supplemental feeding are often necessary therapies.
Celiac Disease
- Gluten-induced enteropathy, causing impaired nutrient absorption.
- Symptoms include fatty stools, malnutrition, and abdominal distension.
- Strict gluten-free diet is crucial for management and remission.
Lactose Intolerance
- Involves difficulty digesting lactose, a sugar found in milk and dairy products.
- Symptoms include bloating, abdominal discomfort, pain and flatulence.
- Treatment typically involves avoiding lactose-containing foods, or using lactose-free alternatives, or enzyme replacement.
PKU-Phenylketonuria
- Metabolic disorder due to a lack of phenylalanine hydroxylase, impacting phenylalanine metabolism.
- Results in toxic levels of phenylalanine in the body, causing various problems, including cognitive impairment, and a characteristic musty odor in urine.
- Early recognition and dietary management are crucial for avoiding severe health consequences.
Short Bowel Syndrome
- Malabsorptive disorder resulting from extensive small-bowel resection.
- Treatments usually include nutritional support and medical therapies.
Hepatic Disorders
- Hyperbilirubinemia, Biliary Atresia, Viral Hepatitis, and Cirrhosis
- Each condition encompasses a wide range of causes, symptoms, potential complications and treatment options.
Hepatitis
- Viral infections affecting the liver
- Transmission via contaminated food or water, blood, or close contact are prominent aspects of the condition.
- Key phases to document include Anicteric (5-7 days) and Icteric (4weeks).
- Prevention and supportive care are central elements of management.
Cirrhosis
- End-stage of liver disease.
- Irreversible condition with various etiologies such as biliary atresia, chronic hepatitis, hemophilia, or cystic fibrosis.
- Potential for various complications
Injuries to the GI System
- Abdominal trauma and poisoning(referring to specific antidotes/intervention for particular toxins)
- Lead poisoning (varied symptoms depending on exposure level)
- Foreign object ingestion.
Nursing Management of All GI Disorders
- Includes preventive strategies, pain control, effective diet and hydration management, and emotional support.
- The nurse’s role extends to both pre- and postoperative care.
Nursing Management: GI Disorders Requiring Surgery
- Addresses pre-operative anxiety, prepares the patient for surgery, and manages post-operative care, including pain assessment, wound healing, fluid and nutrition management and infection prevention.
Developmental Considerations
- GI pain considerations vary between infant, child and adolescent ages.
- Each age group has specific needs for assessment and management.
Summary
- Focuses on the varied causes of GI disorders, common symptoms, and the role of nurses in preventive education and post-treatment support.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.