Podcast
Questions and Answers
Who was one of the first to consider HIPEC as a possible addition to peritoneal surgery?
Who was one of the first to consider HIPEC as a possible addition to peritoneal surgery?
Sugarbaker
What is peritoneal disease often associated with?
What is peritoneal disease often associated with?
- Lung cancer
- Stomach cancer (correct)
- Liver cancer
- Breast cancer
Peritoneal metastases can occur from ovarian, gastric, colorectal, HPV, breast, and melanoma cancers.
Peritoneal metastases can occur from ovarian, gastric, colorectal, HPV, breast, and melanoma cancers.
True (A)
What is considered the 'king of radiological exams' for diagnosing and staging peritoneal carcinomatosis?
What is considered the 'king of radiological exams' for diagnosing and staging peritoneal carcinomatosis?
What are some symptoms that may lead to the identification of peritoneal disease as an incidental finding?
What are some symptoms that may lead to the identification of peritoneal disease as an incidental finding?
The peritoneum has a ________ plasma barrier that limits penetration of chemotherapeutics.
The peritoneum has a ________ plasma barrier that limits penetration of chemotherapeutics.
MRI is not commonly used in the assessment and staging of peritoneal carcinomatosis.
MRI is not commonly used in the assessment and staging of peritoneal carcinomatosis.
Match the following peritoneal tumors with their primary usage:
Match the following peritoneal tumors with their primary usage:
HIPEC usually lasts between 30-90 minutes, during which cytotoxic agents are administered into the peritoneal cavity at an elevated temperature of ____ to ____ degrees Celsius.
HIPEC usually lasts between 30-90 minutes, during which cytotoxic agents are administered into the peritoneal cavity at an elevated temperature of ____ to ____ degrees Celsius.
Match the chemotherapy agent with its associated complication:
Match the chemotherapy agent with its associated complication:
What are the benefits of heat in HIPEC? Select all that apply.
What are the benefits of heat in HIPEC? Select all that apply.
What does HIPEC stand for?
What does HIPEC stand for?
The Peritoneal Carcinomatosis Index (PCI) is a score used to assess the disease based on _____ regions.
The Peritoneal Carcinomatosis Index (PCI) is a score used to assess the disease based on _____ regions.
Mitomycin has specific toxicity on the hematological system.
Mitomycin has specific toxicity on the hematological system.
What is described by patients as a very sharp feeling that is so peculiar that it sometimes lets you diagnose it immediately?
What is described by patients as a very sharp feeling that is so peculiar that it sometimes lets you diagnose it immediately?
Which diagnostic tool is considered one of the most accurate and complete examinations?
Which diagnostic tool is considered one of the most accurate and complete examinations?
Acute appendicitis is the most frequent organic cause of acute abdomen.
Acute appendicitis is the most frequent organic cause of acute abdomen.
The highest incidence of appendicitis is between ages 15 and 30, though it also occurs in ______ and the elderly.
The highest incidence of appendicitis is between ages 15 and 30, though it also occurs in ______ and the elderly.
The results of studies on surgeons and personnel exposed to HIPEC showed significant risks.
The results of studies on surgeons and personnel exposed to HIPEC showed significant risks.
What may a gastric cancer surgeon specialize in?
What may a gastric cancer surgeon specialize in?
What is the particular treatment mentioned that may require a second specialized doctor's opinion?
What is the particular treatment mentioned that may require a second specialized doctor's opinion?
Match the following diseases with their main diagnosis:
Match the following diseases with their main diagnosis:
Which type of tumor is linked to the neuroendocrine system and has specific markers?
Which type of tumor is linked to the neuroendocrine system and has specific markers?
Mesothelial tumors include well-differentiated papillary mesothelioma, multicystic mesothelioma (borderline condition), and ____________ mesothelioma.
Mesothelial tumors include well-differentiated papillary mesothelioma, multicystic mesothelioma (borderline condition), and ____________ mesothelioma.
Flashcards are hidden until you start studying
Study Notes
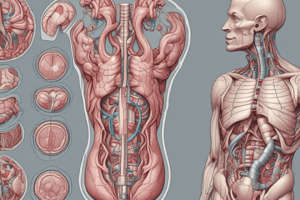
Introduction to Peritoneal Surgery
- Peritoneal disease, which was once considered incurable, can now be treated with specific surgical techniques and a better understanding of the disease's physiopathology.
- Peritoneal surgeons must be wise and consider the benefits and disadvantages of oncological treatment and overall patient survival.
History of Peritoneal Surgery
- The concept of treating peritoneal disease began in the 1980s with Dr. Sugarbaker, who founded the International Society of Regional Cancer Therapy.
- Dr. Sugarbaker considered HIPEC (Hyperthermic Intraperitoneal Chemotherapy) as a possible addition to peritoneal surgery.
Classification of Peritoneal Tumors
- Peritoneal tumors can be classified into:
- Benign and malignant tumors of mesothelial derivation (primary tumors of the peritoneum)
- Lesions of the secondary Mullerian system (e.g., endometriosis)
- Secondary cancers (e.g., peritoneal metastases from other cancers)
Pathophysiology of Peritoneal Disease
- The peritoneum has a plasma barrier that limits the penetration of chemotherapeutics.
- Peritoneal fluid circulation follows gravity and a counterclockwise pattern, with preferred implantation sites in the pelvis, diaphragm, and latero-colic spaces.
- The peritoneum and omentum have specific areas (milky spots) where the plasma barrier is less present, allowing for fluid reabsorption and carcinomatosis implantation.
Resources for Peritoneal Surgery
- The PSOGI (Peritoneal Surface Oncology Group International) is a society dedicated to peritoneal surface oncology.
- The Chicago Consensus Guidelines (2018) provide a summary of treatments for peritoneal diseases.
Assessing Peritoneal Disease
- To assess peritoneal disease, consider:
- Presence of a primary tumor
- Type of peritoneal disease (synchronous or metachronous)
- Burden of peritoneal disease (can be determined radiologically or with diagnostic laparoscopy)
- Peritoneal cancer index (PCI)
Diagnosis and Staging
- Peritoneal disease can be diagnosed incidentally, during initial symptoms, or during the workup of a primary disease.
- Diagnostic and staging exams include:
- CT scan
- MRI
- PET/CT scan
- Exploratory laparoscopy
Peritoneal Carcinomatosis Index (PCI)
- The PCI is a score used to assess the burden of peritoneal disease.
- The PCI is calculated by evaluating 12 regions of the abdomen and assigning a score based on the dimension of the carcinomatosis.
Multidisciplinary Tumor Board (MDT)
- The MDT is essential for deciding on the best course of treatment for patients with peritoneal disease.
- The MDT reviews images and decides on the best approach, considering the expertise of various specialists.
Surgery
- Principles of surgery and therapy for peritoneal disease include:
- Completeness of cytoreduction score
- Indications for surgery (e.g., PCI score, disease location)### Peritoneal Surgery
- Cytoreductive surgery (CRS) is the primary surgery for peritoneal disease, not a curative aimed resection.
- CRS is classified into 4 categories based on the completeness of cytoreduction score (CC-0, CC-1, CC-2, CC-3).
Surgical Candidate
- Patients must be able to tolerate long surgeries and potential multi-visceral resection.
- The extent of carcinomatosis may not be fully predictable, and surgeries can be extremely long.
Techniques
- Multi-visceral resection and peritonectomy are used to remove the peritoneum involved by the disease.
- Sugarbaker's technique: complete peritonectomy + HIPEC (hyperthermic intraperitoneal chemotherapy).
- Partial peritonectomy can be used for smaller nodules.
HIPEC
- Hyperthermic intraperitoneal chemotherapy (HIPEC) involves administering cytotoxic agents into the peritoneal cavity at an elevated temperature (41-43°C).
- Benefits of HIPEC include:
- Damaging locally the cells, addressing minimal residual disease.
- Allowing for better penetration of chemotherapeutic drugs into the tumor.
- Longer direct contact between tumor cells and the chemo reduces or destroys chemoresistance mechanisms.
- HIPEC usually lasts between 30-90 minutes.
Disadvantages of HIPEC
- Risks associated with heat:
- Hyperthermia of the patient.
- Worsening the risk profile associated with cytoreductive surgery.
- Risks associated with chemotherapeutics:
- Mitomycin: toxicity on the hematological system, severe neutropenia.
- Cisplatin: acute kidney insufficiency, requires high-volume IV fluids.
- Oxaliplatin: postoperative bleeding risk, thrombocytopenia.
Choice of Chemotherapy Agent
- Criteria for selecting a chemotherapy agent for HIPEC:
- Hydrosoluble.
- Active at HIPEC temperatures.
- High molecular weight.
- High systemic clearance.
- High capacity of intratumor diffusion.
- Not cell cycle specific.
HIPEC Techniques
- Open technique: uses retractors to keep the abdomen open, and a surgeon with gloved hands to wash out the abdomen.
- Closed technique: closes the abdomen, leaving the fascia exposed to chemotherapy, and uses a machine to heat and circulate the chemotherapy.
Patient Selection for HIPEC
- Exclusion criteria:
- Advanced age (>75).
- Comorbidities (renal disease, etc.).
- Peritonitis or sepsis.
- Malnutrition.
- Extra-abdominal metastasis.
- Massive involvement of retroperitoneum.
- Inability to achieve complete or almost complete cytoreduction (CC-0, CC-1).
Alternatives to HIPEC
- NIPEC (normothermic intraperitoneal chemotherapy): for drugs inactivated by heat.
- EPIC (early postoperative intraperitoneal chemotherapy): uses peritoneal portal system.
- PIPAC (pressurized intraperitoneal aerosol chemotherapy): for palliative reasons, uses pressurization to increase chemotherapy penetration.
- NIPS (neoadjuvant intraperitoneal-systemic chemotherapy protocol): a bimodal therapy using IV and intraperitoneal chemotherapy.
Mesothelial Tumors
- Well-differentiated papillary mesothelioma: tends to be benign.
- Multicystic mesothelioma: borderline condition.
- Malignant mesothelioma: has a terrible prognosis if untreated.
Appendiceal Tumors
- Secondary tumors that spread to the peritoneum.
- Peritoneal metastasis varies depending on the type of tumor.
- Perforation of the appendix increases the risk of peritoneal metastasis.
- Pseudomixoma peritonei: a peculiar peritoneal tumor with a characteristic presentation, characterized by an abundant quantity of mucin.### Peritoneal Surgery
- Types of appendiceal carcinoma:
- Low-grade tumor with disseminated mucin
- High-grade tumor with mucin
- High-grade tumor with signet ring cells
- Goblet cell tumor (specific entity of the appendix, interacts with the enterochromaffin system, has neuroendocrine markers)
Pseudomixoma Peritonei
- Clinical presentation: clear diagnosis, symptoms like perforated appendix and other formations
- Macroscopic and clinical appearance: "jelly belly" appearance
Principles of Systemic Chemotherapy and Surgery
- Chemotherapy: depends on the type of cancer
- Surgery: may require multiple visceral resections (up to 7-9 times), tolerable, but dependent on patient's condition (age, general health)
- HIPEC: performed with specific dosages, may be considered for high-risk patients, extensive lymph node involvement, and specific histotypes related to metastasis
Secondary Carcinomatosis
- Depend on the type of cancer:
- Colorectal carcinomatosis: responsive to drugs and surgery, high heterogeneity
- Pancreaticobiliary carcinomatosis: incurable, no survival improvement with cytoreduction or HIPEC
Colorectal Carcinomatosis
- After response to generalized chemotherapy, HIPEC and surgery may be considered
- PCI (Peritoneal Cancer Index) higher than 10: may be considered for HIPEC and surgery
- Metachronous and synchronous metastasis may arise
Gastric Carcinomatosis
- Recurrence of disease after surgery: common (up to 50% of patients)
- Survival after peritoneal failure: 3-8 months
- Adjuvant therapy may extend survival time
- NOMOgrams: useful tools to understand and predict the risk of metachronous peritoneal carcinomatosis
Acute Abdomen
- Definition: sudden onset of pain, requiring prompt decision on intervention
- Causes:
- Distension or spasm of a hollow viscus
- Distension of the capsule of parenchymatous organs
- Traction on the mesentery, ligaments, or peritoneum (especially parietal peritoneum)
- Infiltration or compression of sensitive nerves
- Irritating substances (e.g., bile) in the peritoneum
Diagnostic Tools
- Objective exam: Blumberg sign
- US: first choice, non-invasive, useful for detecting air, perforation, or obstruction
- CT scan: accurate and complete examination
- Fecal exam: useful in patients with communication problems (psychiatric, neurologic, geriatric)
Disease Approach
- Primite etiology: essential to avoid progression to peritonitis
- Main causes of acute abdomen:
- Acute appendicitis
- Acute cholecistitis
- Acute pancreatitis
Appendicitis
- Definition: obstruction of the appendix lumen, leading to bacterial overgrowth, stasis, and increased pressure
- Causes:
- Fecaliths
- Foreign bodies
- Tumors
- Lymphoid hyperplasia
- Stages:
- Minor inflammation
- Phlegmonous appendicitis
- Necrosis
- Gangrene
- Complications:
- Localized or diffuse peritonitis
- Abscesses
- Rarely, portal vein thrombosis
- Diagnosis:
- Clinical evaluation
- Laboratory tests
- Imaging (US, CT scans)
- Alvarado score
- Treatment:
- Surgical (laparoscopic or open)
- Conservative (antibiotics)
- Postoperative considerations:
- Complications (superficial and deep surgical site infections, bowel obstruction, secondary infertility)
- Chronic appendicitis: a controversial condition, may require elective appendectomy
Cholecystitis
- Pathophysiology: similar to appendicitis
- Risk factors:
- Conditions causing bile stasis
- Advanced age
- Hormonal factors
- Drug use
- Diagnosis:
- Ultrasound
- CT scan with contrast (in severe cases)
- Treatment:
- Surgery (cholecystectomy)
- Conservative management with antibiotics (in cases where surgery is delayed)
- Complex cases:
- Alternative treatments (percutaneous cholecystostomy)
- Delayed, elective cholecystectomy
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.