Podcast
Questions and Answers
What is a common consequence of misplaced gastrostomy tubes in pediatric patients?
What is a common consequence of misplaced gastrostomy tubes in pediatric patients?
- Tract disruption
- Stoma stenosis
- Granulation tissue formation
- All of the above (correct)
What percentage of patients with gastrostomy tubes experience displacement within 30 days of initial placement?
What percentage of patients with gastrostomy tubes experience displacement within 30 days of initial placement?
- 20%
- 80%
- 40%
- 61% (correct)
Why is timely replacement of a displaced gastrostomy tube important?
Why is timely replacement of a displaced gastrostomy tube important?
- To prevent tract disruption
- To prevent stoma stenosis (correct)
- To prevent granulation tissue formation
- To prevent infection
What is the name of the interorganizational workgroup that addressed nasogastric tube misplacement issues?
What is the name of the interorganizational workgroup that addressed nasogastric tube misplacement issues?
What percentage of all diagnosed cancers did head and neck cancers represent globally in 2017?
What percentage of all diagnosed cancers did head and neck cancers represent globally in 2017?
What is the primary goal of the ASPEN Pediatric Section workgroup?
What is the primary goal of the ASPEN Pediatric Section workgroup?
What is a major nutrition challenge in head and neck cancer patients?
What is a major nutrition challenge in head and neck cancer patients?
Why do patients undergoing cardiac surgery often experience delays in initiation of medical nutrition therapy?
Why do patients undergoing cardiac surgery often experience delays in initiation of medical nutrition therapy?
What is a common factor that may impact outcomes from pediatric critical illness?
What is a common factor that may impact outcomes from pediatric critical illness?
What is the consequence of acute nutritional deficiencies in cardiac surgery patients?
What is the consequence of acute nutritional deficiencies in cardiac surgery patients?
What is a consequence of preexisting or acquired nutritional deterioration in pediatric critical illness?
What is a consequence of preexisting or acquired nutritional deterioration in pediatric critical illness?
What is the primary reason for the development of the ASPEN International Nutrition Guidelines?
What is the primary reason for the development of the ASPEN International Nutrition Guidelines?
What is a common risk factor for worsening nutritional status in pediatric critical illness?
What is a common risk factor for worsening nutritional status in pediatric critical illness?
What is the consequence of tract disruption in gastrostomy tube replacement?
What is the consequence of tract disruption in gastrostomy tube replacement?
What is the estimated daily muscle loss in immobilized children with respiratory failure?
What is the estimated daily muscle loss in immobilized children with respiratory failure?
Why is verification of appropriate placement prior to tube use essential?
Why is verification of appropriate placement prior to tube use essential?
What is the purpose of updating the ASPEN/SCCM Pediatric Critical Care Nutrition Guideline?
What is the purpose of updating the ASPEN/SCCM Pediatric Critical Care Nutrition Guideline?
What is the frequency of nutritional status assessment recommended for pediatric critically ill patients?
What is the frequency of nutritional status assessment recommended for pediatric critically ill patients?
What is the primary reason for the increasing rates of gastrostomy tube placement in the United States?
What is the primary reason for the increasing rates of gastrostomy tube placement in the United States?
Which type of gastrostomy tubes are most commonly used in pediatric patients?
Which type of gastrostomy tubes are most commonly used in pediatric patients?
What is a primary advantage of low-profile balloon gastrostomy tubes over percutaneous tubes?
What is a primary advantage of low-profile balloon gastrostomy tubes over percutaneous tubes?
Who typically performs primary placement of low-profile balloon gastrostomy tubes in pediatric patients?
Who typically performs primary placement of low-profile balloon gastrostomy tubes in pediatric patients?
What is a common reason for replacement of balloon gastrostomy tubes?
What is a common reason for replacement of balloon gastrostomy tubes?
Where can replacement of balloon gastrostomy tubes occur?
Where can replacement of balloon gastrostomy tubes occur?
What is a current limitation in the management of balloon gastrostomy tubes?
What is a current limitation in the management of balloon gastrostomy tubes?
Why is there a need for standardization in balloon gastrostomy tube placement and management?
Why is there a need for standardization in balloon gastrostomy tube placement and management?
Study Notes
Gastrostomy Tube Placement
- Rates of gastrostomy tube (GT) placement are rising in the US due to increased appreciation for nutrition support and refined placement techniques.
- Initial placement techniques for balloon gastrostomy tubes (BGT) include percutaneous endoscopic, radiologic, laparoscopic, and open surgical methods.
- Pediatric GTs are mostly placed by surgeons and interventional radiologists, with many surgeons performing primary placement of low-profile balloon gastrostomy (LPBG) tubes.
Advantages and Challenges of LPBG Tubes
- LPBG tubes are appreciated by patients and caregivers for their aesthetic appeal and ease of use.
- They sit at skin level, can be concealed, and provide limited interference with clothing.
- LPBGs are thought to have fewer adverse events, such as accidental dislodgement and leakage, compared to percutaneous tubes.
Replacement and Verification of BGT Placement
- BGTs require replacement due to wear and tear and unexpected dislodgement.
- Management for routine and non-routine tube replacement lacks standardization and varies widely among institutions and settings.
- No overall standard of care exists for placement verification following BGT replacement.
- Replacement can occur in various settings, including pediatric inpatient units, emergency departments, outpatient clinics, and residential pediatric care facilities.
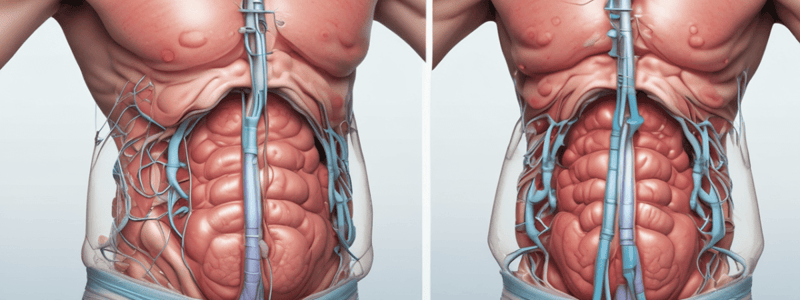
Consequences of Misplaced GTs
- Gastrostomy tube displacement in children leads to ED visits in up to 61% of patients within 30 days of initial placement.
- Timely replacement of a displaced GT is required to prevent stoma stenosis.
- Misplaced tubes can lead to serious consequences, including ED visits, hospital readmissions, additional surgical interventions, etc.
Importance of Verification of Appropriate Placement
- Verification of proper placement is essential to detect potential misplacement or adverse events.
- Tract disruption is a common adverse consequence of GT replacement, which may lead to dislodgment, leakage of gastric contents, infection, development or worsening of granulation tissue, or peritonitis.
ASPEN Guidelines for BGT Replacement Verification
- In 2012, ASPEN convened the NOVEL workgroup to address nasogastric tube misplacement issues.
- A multi-organizational workgroup was later convened to develop evidence-based or expert opinion clinical guidelines for BGT replacement verification in pediatric patients.
Nutrition Guidelines for Adult Perioperative Cardiac Patients
- Patients undergoing cardiac surgery are at increased risk of iatrogenic underfeeding during the pre- and postoperative course.
- Delays in initiating medical nutrition therapy (MNT) and lower overall total nutritional adequacy are common in this population.
- Acute nutritional deficiencies may exacerbate pre-existing malnutrition, leading to complicated and prolonged critical illness courses.
Nutrition Guidelines for Adult Head and Neck Cancer
- Head and neck cancer patients present special nutrition challenges and are at higher risk for malnutrition due to difficulties with chewing and swallowing.
- Treatment toxicities and tumor-related symptoms can further compromise nutritional status in this population.
ASPEN/SCCM Pediatric Critical Care Nutrition Guideline
- Nutritional status on admission, nutrient delivery, and nutritional deterioration are important factors that impact outcomes from pediatric critical illness.
- Preexisting malnutrition is common in children admitted to the pediatric intensive care unit (PICU).
- Imbalance between nutrient requirement and delivery, excessive nutrient losses, and altered nutrient absorption or utilization during critical illness may result in nutritional deterioration.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the different methods of gastrostomy tube placement, including percutaneous endoscopic, radiologic, laparoscopic, and open surgical methods. It also discusses the role of nutrition support and growth.