Podcast
Questions and Answers
What is the primary characteristic of non-inflammatory diarrhea?
What is the primary characteristic of non-inflammatory diarrhea?
- Presence of mucous and blood
- Severe abdominal cramping
- Watery stool with large volume (correct)
- Presence of fever
Which organism is NOT typically associated with non-inflammatory diarrhea?
Which organism is NOT typically associated with non-inflammatory diarrhea?
- Clostridium difficile (correct)
- Enterotoxigenic E. coli
- Giardia lamblia
- Vibrio cholerae
What type of diarrhea is characterized by the invasion of intestinal mucosa?
What type of diarrhea is characterized by the invasion of intestinal mucosa?
- Chronic diarrhea
- Inflammatory diarrhea (correct)
- Enterotoxin-mediated diarrhea
- Non-inflammatory diarrhea
Which of the following is a characteristic of dysentery?
Which of the following is a characteristic of dysentery?
What is the main role of normal flora in the gastrointestinal tract?
What is the main role of normal flora in the gastrointestinal tract?
Which characteristic is NOT associated with inflammatory diarrhea?
Which characteristic is NOT associated with inflammatory diarrhea?
Which of the following organisms is associated with enterotoxin-mediated diarrhea?
Which of the following organisms is associated with enterotoxin-mediated diarrhea?
What is a defining factor of diarrhea categorized as enterocolitis?
What is a defining factor of diarrhea categorized as enterocolitis?
Which term refers to inflammation of the rectal mucosa?
Which term refers to inflammation of the rectal mucosa?
Which of the following statements about diarrhea is false?
Which of the following statements about diarrhea is false?
Flashcards
Gastroenteritis
Gastroenteritis
Inflammation of the stomach and intestines.
Gastritis
Gastritis
Inflammation of the stomach.
Enterocolitis
Enterocolitis
Inflammation of the small and large intestines.
Diarrhea
Diarrhea
Signup and view all the flashcards
Dysentery
Dysentery
Signup and view all the flashcards
Proctitis
Proctitis
Signup and view all the flashcards
Normal Flora
Normal Flora
Signup and view all the flashcards
Non-Inflammatory Diarrhea
Non-Inflammatory Diarrhea
Signup and view all the flashcards
Inflammatory Diarrhea
Inflammatory Diarrhea
Signup and view all the flashcards
Enterotoxin-Mediated Diarrhea
Enterotoxin-Mediated Diarrhea
Signup and view all the flashcards
Study Notes
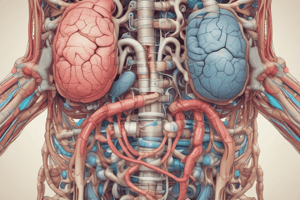
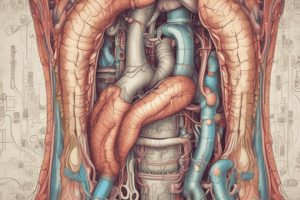
Gastrointestinal Tract
- The gastrointestinal tract includes the esophagus, stomach, small intestines (duodenum, jejunum, ileum), large intestines (cecum, colon, rectum), and anus.
- The introduction section of the notes lists these elements in order, and includes an image giving a visual representation of the GI tract organs.
Gastrointestinal Tract Terms
- Gastritis: Inflammation of the stomach.
- Gastroenteritis: Inflammation of the stomach and intestines.
- Enterocolitis: Inflammation of the small and large intestines.
Gastrointestinal Tract Terms (cont.)
- Diarrhea: Abnormal increased bowel movements, often loose to liquid stool.
- Dysentery: Diarrhea with cramping abdominal pain.
- Proctitis: Inflammation of the rectal mucosa.
- Conditions causing Proctitis: N. gonorrhoeae, C. trachomatis, T. pallidum
Normal Flora
- 80% of the dry weight of feces is bacteria.
- Normal flora helps prevent colonization by pathogens.
- Key bacteria include anaerobic bacilli (Bacteroides spp.), GN enteric bacilli, Enterococci, Streptococci, S. aureus, and yeast (Candida).
Non-Inflammatory Diarrhea
- Caused by bacterial toxins (enterotoxin).
- Results in the outpouring of electrolytes and fluid, leading to watery stools.
- Individuals are not febrile.
- Stool does not contain PMN, blood, or mucus.
Non-Inflammatory Diarrhea (cont.)
- Common causes: V. cholerae, Enterotoxigenic E. coli, Bacteroides spp., Viruses, Giardia lamblia, Cyclospora, Cryptosporidium.
Inflammatory Diarrhea
- Organisms invade the intestinal mucosa.
- Cytotoxins destroy intestinal cells.
- Individuals have fever and loose, small-volume stools.
- Stool usually contains PMNs, blood, and mucus.
Inflammatory Diarrhea (cont.)
- Common causes: Salmonella spp., Shigella spp., Y. enterocolitica, Campylobacter spp., Enteroinvasive E. coli, Clostridium difficile.
Enterotoxin-Mediated Diarrhea
- Caused by ingestion of food containing toxins.
- Rapid onset (less than 12 hours).
- Common causes include Enterotoxigenic E. coli, V. cholera, S. aureus, C. perfringens, B. cereus.
Diarrheal Diseases
- Salmonella: gastroenteritis
- Shigella: bacillary dysentery
- Y. enterocolitica: enterocolitis (can resemble acute appendicitis)
- Campylobacter jejuni and C. coli
- Edwardsiella tarda (uncommon)
- Vibrio cholerae: cholera
- V. parahaemolyticus: milder case
- Plesiomonas shigelloides
- Listeria monocytogenes: gastroenteritis
Diarrheal Diseases (cont.)
- Intestinal parasites: Giardia, Entamoeba, Cryptosporidium, Cyclospora, Microsporidia
- Viruses: Rotavirus, adenovirus, calcivirus, astrovirus
Diseases (cont.)
- H. pylori: chronic gastritis, peptic and duodenal ulcers
- C. difficile: antibiotic-associated diarrhea, pseudomembranous colitis
- C. perfringens: enterotoxin
- Mycobacterium avium: GI diseases in AIDS patients
- E. coli: enterohemorrhagic (O157:H7 and others, cause hemorrhagic colitis and hemolytic uremic syndrome (HUS)), enteroinvasive (Shigella-like disease), enterotoxigenic (traveler's diarrhea), enteropathogenic (enteroadherent, usually children), enteroaggregative (traveler's diarrhea)
Specimen Collection
- For fecal specimens (2-3 samples), a clean, non-sterile, wide-mouth container without urine contamination is used with Cary-Blair transport medium.
- Process specimens within 1–2 hours of collection.
- Other specimens include duodenal, colostomy, ileostomy material, and diapers.
- Additional include food specimens collected by public health departments.
Visual Examination
- Macroscopic examination includes stool consistency (watery, formed, or loose) and color. Observation of blood and mucus is also included
Microscopic Examination
- Fecal WBC (PMN) can aid in distinguishing inflammatory from non-inflammatory diarrhea. Use methylene blue for wet mounts.
- Motility of Campylobacter can be assessed.
- Gram staining is used for identifying bacteria. Campylobacter has a seagull-wing appearance.
- GPR morphology is used to identify Clostridium.
Stool WBC
- Distinguish inflammatory diarrhea from non-inflammatory diarrhea
Culture
- Culture is not generally done for all samples, it is done based on patient history and symptoms.
- Cultures for specific specimens like Salmonella, Shigella, Campylobacter, E. coli O157:H7, and Vibrio are considered.
- Physicians should request specific culture tests.
Media Inoculation
- Non-sterile pipettes or swabs are used.
- Plates are streaked for isolation.
- Enrichment broth containing large amounts of specimen are inoculated.
Media
- BAP or EMB media detects S. aureus and yeast overgrowth.
- MAC or EMB are used for differential and selective testing.
- NLF is used to identify Salmonella, Shigella, Y. enterocolitica, E. tarda, Plesiomonas, Aeromonas, Vibrio.
- XLD or HE, SS agar is differential and selective media to identify Salmonella and Shigella (colorless colonies, +/- black center).
- Campy-BAP is a selective media used to isolate Campylobacter jejuni and C. coli.
- Enrichment broth is used (GN/Salmonella, Shigella/Selenite F/Salmonella, some Shigella).
- Special media, such as Cefsulodin-irgasan-novobiocin (CIN) agar, Salmonella Shigella (SS) agar, and Cycloserine-cefoxitin-fructose agar (CCFA), are used to identify specific organisms.
MAC
- Media is used to differentiate bacteria that ferment lactose.
Gram Stain Analysis of Sputum
- Count the number of epithelial and PMN cells per low-power field (LPF).
- A good specimen will have < 10 epithelial/LPF and >25 PMN/LPF. Reject specimens with >25 epithelial cells per LPF.
- Under oil immersion, record the quantity (rare, moderate, or many) and type of bacteria.
Acceptable Gram Stain
- Acceptable Gram Stain images are provided for comparison in the slides.
Routine Cultures
- BAP, CHOC, MAC
- Incubated at 35°C in CO2
- Other media are sometimes used for particular patient situations (e.g., cystic fibrosis)
Anaerobic Cultures
- Lung aspirates (pleural fluid) and open-lung biopsies are only cultured anaerobically if the method did not involve the oral cavity.
Work-Up
- Analysis depends on the specimen quality and type.
- Gram stain evaluation is important.
Reporting Results
- Susceptibility panel and identification results are reported.
- Public health officials are notified when Salmonella or Shigella are isolated.
- Overgrowth of S. aureus, yeast, or Ps. aeruginosa should be reported.
- Negative results report no isolation of Salmonella, Shigella, Vibrio, E. coli O157:H7, or Campylobacter.
Respiratory Tract
- Upper Respiratory Tract (URT) infections involve the oral cavity and neck (nose, mouth, throat, epiglottis, larynx)
- Contains normal flora.
- Lower respiratory tract (LRT) infections include the trachea, bronchi, bronchioles, and lung alveoli.
- Below the larynx, the tract is typically sterile.
URT Normal Flora
- Staphylococci (CONS, S. aureus)
- Streptococci (viridans, pneumococci)
- Micrococcus spp.
- Diphtheroids,Neisseria spp.
- Haemophilus,Anaerobes,Spirochetes,Candida spp.
URT Infections
- Thrush, Laryngitis, Epiglottitis, Phayngitis, Tonsillitis, Sinusitis, Otitis media, Diphtheria, Pertussis (Whooping cough).
URT Pathogens
- Respiratory viruses (e.g., influenza, parainfluenza, RSV, adenovirus, rhinovirus, coronavirus, coxsackie A, EBV, CMV)
- S. pyogenes
- B-hemolytic strep group C, F and G
- Arcanobacterium haemolyticum;
- H. influenzae, N. gonorrhoeae, Corynebacterium diphtheriae, Bordetella pertussis, Parapertussis, Yeast
URT Specimen Collection
- Specimens obtained with syringes and needles, swabs, and/or biopsies.
- Diphtheria is cultured on BAP, Loeffler, tellurite media.
- Pertussis is cultured on Bordet-Gengou blood agar.
- Posterior pharynx and tonsils are swabbed, placed in transport media.
URT Microscopic Examination
- Gram stain is not typically done because it shows a lot of normal flora.
URT Culture
- Mainly for group A strep (mostly).
- Other organisms (e.g., B, C, F, G), N. gonorrhoeae, Arcanobacterium haemolyticum, and C. diphtheriae, are also possible, depending on patient needs.
- Throat cultures demonstrate specific examples.
Epiglottitis
- Common in 2–6-year-old children.
- Almost exclusively caused by H. influenzae type b (becoming rare because of vaccination).
- Can cause obstructed airways.
- Diagnosed clinically.
- Collection of samples may be hazardous.
- Blood cultures may be needed (bacteremia).
Sinusitis
- Often preceded by a viral URTI.
- Acute sinusitis agents include S. pneumoniae, H. influenzae, M. catarrhalis, group A strep, anaerobes, S. aureus, and GNR.
- Chronic sinusitis can be caused by anaerobes, S. aureus (adults) or S. pneumoniae, S. aureus, viridans streptococci (children).
Otitis Media
- Middle ear infection.
- Common in children <10 years.
- Usually follows viral URTI.
- Common agents include S. pneumoniae, H. influenzae, other bacteria (group A strep, S. aureus), M. catarrhalis, anaerobes, GNR.
Specimen Collection (Otitis Media)
- Tympanocentesis collects fluid (TF).
- Aseptically puncturing the tympanic membrane and aspirating fluid is used.
- Specimen is placed in an anaerobic transport medium.
- A swab can collect samples from ruptured eardrums.
Processing TF
- Gram stain and culture samples in both anaerobic and aerobic conditions (BAP, CHOC, MAC, anaBAP).
- Identify and perform susceptibility tests
LRT Infections
- Bronchitis/Influenzae, Pneumonia, Empyema, Pleural fluid, Tuberculosis
LRT Pathogens
- Respiratory viruses (including Influenza A and B)
- S. pneumoniae, H. influenzae, M. catarrhalis, M. pneumoniae, Chlamydia spp.
- GNR, S. aureus, Legionella spp., Anaerobes, Mycobacteria, Fungi
Community-Acquired Pneumonia
- S. pneumonia (most common, pneumococcal pneumonia)
- Mycoplasma pneumoniae, H. influenzae, M. catarrhalis
Hospital-Acquired Pneumonia
- Contaminated ventilators/inhalation therapy
- Enterobacteriaceae, K. pneumoniae, S. marcescens, S. aureus, NFGNR, P. aeruginosa, Burkholderia cepacia, CF and nosocomial S. pneumoniae, Anaerobic bacteria
Miscellaneous Causative Agents
- Mycobacteria (MTB), Legionella (immunocompromised individuals, community acquired/nosocomial), Chlamydia (C. trachomatis in neonates, C. pneumoniae in young adults).
Emerging Viral Infections
- Avian Influenza-H5N1, H1N1 influenza A, SARS coronavirus
Bioterrorism Agents
- B. anthracis (anthrax), Y. pestis (plague), Coxiella burnetii (Q fever), F. tularensis (tularemia)
Routes of Infection
- Most are opportunistic.
- Waiting for low defenses to infect lungs.
- Inhalation of infectious aerosols.
- Hemotogenous (blood stream).
- Aspiration of oral secretions (excessive drinking, intubation).
- Sputum - easiest specimen but difficult interpretations due to contamination with normal flora.
Specimen Collection(LRT)
- Sputum - the matter ejected from the LRT through the mouth (may be contaminated with NF); Washings, brushing, biopsies, pleural fluid samples, and tracheal/bronchial aspirates; bronchial washings, brushing, biopsies.
- Specific specimens like for cystic fibrosis require specialized media like for B. cepacia, MRSA, and Pseudomonas.
Sputum: Non-invasive Collection Methods
- Expectorated Sputum, Deep Cough, Induced Sputum (methods), Assisted by RT and chest percussions
- Inhale aerosolized saline to induce cough
- Tracheostomy/endotracheal aspirates, Sucking/Suctioning secretions into tubes.
Sputum: Invasive Collection Methods
- Bronchoscopy (specimens), bronchial lavage washings, and bronchial brushings.
- Reserved for cases involving unusual infections or cases where sputum specimens cannot diagnose the condition (chronic or immunocompromised patients).
Specimen Transport and Processing (LRT)
- Sterile screw-cap cups/tubes
- Bronchial brush placement in sterile saline.
- Specimens must be cultured within two hours of collection.
- Processing includes Gram stain and culture.
Sputum Gram Stain
- May reveal the causative agent.
- Determine sputum quality, suitability for culture (e.g., distinguish between spit/sputum).
- Low-power field (LPF) (10X): determine the quantity of epithelial/normal flora/PMNs
- Oil immersion (100X): morphology, quantity.
Gram Stain Analysis of Sputum
- LPF (10X): count the number of epithelial and PMNs per LPF, classify results as <10, >10, <25, >25
- A good specimen will have < 10 epithelial and >25 PMNs per LPF.
- Reject specimens if there are more than 25 epithelial cells per LPF.
- Record the quantity of bacteria observed (rare, moderate, or many) and the type of bacteria. -Images are shown of unacceptable and acceptable gram stains
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.