Podcast
Questions and Answers
Which part of the gastrointestinal tract directly processes food and waste?
Which part of the gastrointestinal tract directly processes food and waste?
- Liver
- Large intestine (correct)
- Pancreas
- Salivary glands
What is the primary function of bile acids in digestion?
What is the primary function of bile acids in digestion?
- Transport nutrient molecules
- Solubilize lipids (correct)
- Secrete electrolytes
- Hydrolyze macromolecules
Which organs are essential for the digestion and absorption of all basic nutrients?
Which organs are essential for the digestion and absorption of all basic nutrients?
- Teeth and tongue
- Gallbladder and salivary glands
- Pancreas and small intestine (correct)
- Stomach and esophagus
Which of the following processes is NOT part of the sequence of events for digestion and absorption?
Which of the following processes is NOT part of the sequence of events for digestion and absorption?
Which type of cells in the salivary glands, gastric mucosa, and pancreas support enzyme secretion?
Which type of cells in the salivary glands, gastric mucosa, and pancreas support enzyme secretion?
What primarily controls salivary secretion?
What primarily controls salivary secretion?
Which area of the brain is responsible for controlling salivary secretion?
Which area of the brain is responsible for controlling salivary secretion?
Which of the following agents inhibits salivary secretion?
Which of the following agents inhibits salivary secretion?
What is xerostomia?
What is xerostomia?
How does sympathetic stimulation affect salivary secretion?
How does sympathetic stimulation affect salivary secretion?
What is the primary function of kallikrein in the salivary glands?
What is the primary function of kallikrein in the salivary glands?
Which factors are known to inhibit salivary secretion?
Which factors are known to inhibit salivary secretion?
What effect does pilocarpine have on salivary secretion?
What effect does pilocarpine have on salivary secretion?
What is the primary product of endopeptidase activity in the stomach?
What is the primary product of endopeptidase activity in the stomach?
What happens during the phenomenon known as alkaline tide?
What happens during the phenomenon known as alkaline tide?
Which of the following factors does NOT contribute to the secretion of H+ in the stomach?
Which of the following factors does NOT contribute to the secretion of H+ in the stomach?
What is the main function of the gastric mucosal barrier?
What is the main function of the gastric mucosal barrier?
What initiates the secretion of somatostatin in the stomach?
What initiates the secretion of somatostatin in the stomach?
How thick is the mucus gel layer that protects the gastric mucosa?
How thick is the mucus gel layer that protects the gastric mucosa?
What is the consequence of the absence of gastrin, histamine, or acetylcholine on H+ secretion?
What is the consequence of the absence of gastrin, histamine, or acetylcholine on H+ secretion?
What percentage of lipid digestion occurs in the stomach due to gastric lipase?
What percentage of lipid digestion occurs in the stomach due to gastric lipase?
What is the primary function of Brunner's glands in the small intestine?
What is the primary function of Brunner's glands in the small intestine?
Which of the following enzymes is responsible for breaking down disaccharides into monosaccharides?
Which of the following enzymes is responsible for breaking down disaccharides into monosaccharides?
What is the pH range of intestinal juice?
What is the pH range of intestinal juice?
Which hormone does NOT inhibit acid secretion in the stomach?
Which hormone does NOT inhibit acid secretion in the stomach?
Which of the following components is NOT a part of the composition of intestinal juice?
Which of the following components is NOT a part of the composition of intestinal juice?
Which gland secretes substances in response to irritating stimuli and vagal stimulation?
Which gland secretes substances in response to irritating stimuli and vagal stimulation?
What is the main role of cholecystokinin in digestion?
What is the main role of cholecystokinin in digestion?
How much intestinal juice is typically produced per day?
How much intestinal juice is typically produced per day?
What is the primary composition of bile from the liver?
What is the primary composition of bile from the liver?
What is one of the roles of bile salts in digestion?
What is one of the roles of bile salts in digestion?
Which of the following substances is considered a powerful choleretic?
Which of the following substances is considered a powerful choleretic?
What is the capacity of the gallbladder?
What is the capacity of the gallbladder?
Which statement describes a change that occurs in bile when stored in the gallbladder?
Which statement describes a change that occurs in bile when stored in the gallbladder?
What role does secretin play in biliary secretion?
What role does secretin play in biliary secretion?
What happens to bile pH during storage in the gallbladder?
What happens to bile pH during storage in the gallbladder?
Which of the following is a function of bile salts related to cholesterol?
Which of the following is a function of bile salts related to cholesterol?
Flashcards are hidden until you start studying
Study Notes
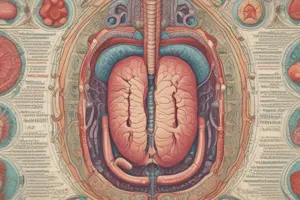
GIT System Subdivisions
- Alimentary Canal: Pathway for food and waste; includes mouth, pharynx, esophagus, stomach, small intestine, and large intestine.
- Accessory Organs: Connected to the alimentary canal; involved in digestion but not in the passage of food; includes teeth, tongue, salivary glands, liver, gallbladder, and pancreas.
Digestion and Absorption Sequence
- Mechanical Homogenization: Mixing of food with digestive fluids throughout the GIT.
- Enzyme Secretion: Over 30g of digestive enzymes produced daily to break down macromolecules into smaller units (oligomers, dimers, monomers).
- Electrolyte Secretion: Acids and bases secreted to maintain an optimal environment for enzymes.
- Bile Acids: Function as biological detergents to emulsify lipids for better digestion and absorption.
- Intestinal Final Digestion: Completed by intestinal surface enzymes breaking down nutrients further.
- Nutrient Transport: Nutrients absorbed from intestinal lumen into the bloodstream.
Specialized GIT Components
- Glands and Epithelia: Specialized glands (salivary glands, stomach, pancreas, liver, intestines) support digestion.
- Exocrine Cells: Produce enzymes for digestion within the GIT lumen.
Salivary Secretion Control
- Autonomic Regulation: Salivary secretion controlled primarily by the autonomic nervous system, not by GIT hormones.
- Parasympathetic Activation: Increased salivation initiated by the salivatory nuclei in the brainstem; stimulated by taste, smell, and chewing.
- Inhibitors: Atropine inhibits saliva; agents like pilocarpine increase secretion.
- Sympathetic Stimulation: Leads to a smaller increase in salivation, primarily through beta-adrenergic receptors.
Stomach Structure
- Regions: Divided into Cardia (cardiac glands), Fundus and Body (oxytonic or parietal glands), and Antrum (pyloric glands).
- Surface Mucous Cells: Produce neutral mucins and bicarbonate (HCO3-).
- Digestive Function: Partial lipid digestion occurs via gastric lipase.
HCl Production and Regulation
- Alkaline Tide: During active acid secretion, parietal cells release HCl and HCO3- into the bloodstream, causing an alkaline shift.
- HCl Secretion Regulation: Driven by gastrin, histamine, and acetylcholine; absence of any factor affects H+ secretion.
Gastric Mucosa Protection
- Gastric Mucosal Barrier: Mucus gel and alkaline secretions protect the mucosa from acidic contents.
- Mucus Layer: About 0.2mm thick; maintains near-neutral pH for epithelial cells despite acidic luminal environment.
Intestinal Secretions
- Brunner's Glands: Secrete alkaline mucus in response to irritation, vagal stimulation, and secretin.
- Crypts of Liberkuhn: Produce intestinal juice with a volume of 1800 ml/day, pH 7.5-8; involved in acid neutralization and nutrient breakdown.
- Enzymes Present: Include peptidase, sucrase, maltase, lactase, lipase, and enterokinase.
Bile Secretion
- Composition: Roughly 97% water and 3% solids; contains bile salts, mucin, bile pigments, lipids, and inorganic substances.
- Physiological Roles: Aids in lipid digestion, cholesterol elimination, fat-soluble vitamin absorption, and cholesterol solubility to prevent galls stones.
Biliary Secretion Regulation
- Choleretics: Substances that enhance bile secretion; includes bile salts, secretin, gastrin, CCK, and vagal stimulation.
- Gallbladder Function: Stores bile, absorbs water to concentrate bile up to 5-10 times, and regulates pH to prevent gallstone formation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.