Podcast
Questions and Answers
What is the primary mechanism behind heartburn in GERD?
What is the primary mechanism behind heartburn in GERD?
- Excessive production of stomach acid
- Increased production of bile, irritating the esophagus
- Weakening of the esophageal sphincter allowing gastric acid reflux (correct)
- Inflammation of the stomach lining due to bacterial infection
Taking antacids like Tums or Rolaids can prevent the release of acid, preventing GERD in the long term.
Taking antacids like Tums or Rolaids can prevent the release of acid, preventing GERD in the long term.
False (B)
List three risk factors for Gastroesophageal Reflux Disease (GERD).
List three risk factors for Gastroesophageal Reflux Disease (GERD).
Obesity, pregnancy, smoking
Over time, GERD can lead to a precancerous condition in the esophagus called ______'s Esophagitis.
Over time, GERD can lead to a precancerous condition in the esophagus called ______'s Esophagitis.
A patient with chest pain is given a "cardiac cocktail" in the ER. If their pain resolves, what is the likely diagnosis?
A patient with chest pain is given a "cardiac cocktail" in the ER. If their pain resolves, what is the likely diagnosis?
A Nissen fundoplication, a surgical treatment for severe reflux, allows patients to vomit or belch air from the stomach.
A Nissen fundoplication, a surgical treatment for severe reflux, allows patients to vomit or belch air from the stomach.
What is the primary issue caused by a hiatal hernia?
What is the primary issue caused by a hiatal hernia?
Hiatal hernias are more common in individuals over ______ years old.
Hiatal hernias are more common in individuals over ______ years old.
What bacteria is most commonly associated with peptic ulcer disease (PUD)?
What bacteria is most commonly associated with peptic ulcer disease (PUD)?
Peptic Ulcer Disease (PUD) pain is typically worsened by eating.
Peptic Ulcer Disease (PUD) pain is typically worsened by eating.
Why are stress ulcers common in hospitalized patients?
Why are stress ulcers common in hospitalized patients?
A positive fecal occult blood test result, without visible blood in the feces, indicates ______ GI bleeding.
A positive fecal occult blood test result, without visible blood in the feces, indicates ______ GI bleeding.
What does "coffee-ground emesis" typically indicate?
What does "coffee-ground emesis" typically indicate?
Irritable Bowel Syndrome (IBS) causes structural damage to the gastrointestinal tract.
Irritable Bowel Syndrome (IBS) causes structural damage to the gastrointestinal tract.
What is a defining characteristic of IBS-related abdominal pain?
What is a defining characteristic of IBS-related abdominal pain?
In Crohn's disease, lesions involving the bowel are characterized as ______ lesions due to the patchy nature of the inflammation.
In Crohn's disease, lesions involving the bowel are characterized as ______ lesions due to the patchy nature of the inflammation.
Which layer of the bowel is affected by Ulcerative Colitis (UC)?
Which layer of the bowel is affected by Ulcerative Colitis (UC)?
Colorectal cancer is more common in men than in women.
Colorectal cancer is more common in men than in women.
List two risk factors for colorectal cancer.
List two risk factors for colorectal cancer.
Match the following terms related to GI bleeding with their descriptions:
Match the following terms related to GI bleeding with their descriptions:
Flashcards
GERD Pathophysiology
GERD Pathophysiology
Weak esophageal sphincter allows gastric juices to backflow into the esophagus, causing inflammation and tissue erosion.
Cause of Heartburn
Cause of Heartburn
Heartburn is caused by chyme and gastric acid regurgitating into the esophagus, leading to inflammation and erosion.
GERD Signs/Symptoms
GERD Signs/Symptoms
Pain worsens when lying down; may mimic heart attack; respiratory symptoms due to gastric reflux into larynx.
GERD Risk Factors
GERD Risk Factors
Signup and view all the flashcards
GERD Treatment
GERD Treatment
Signup and view all the flashcards
GERD complication
GERD complication
Signup and view all the flashcards
Hiatal Hernia Pathophysiology
Hiatal Hernia Pathophysiology
Signup and view all the flashcards
Hiatal Hernia Treatment
Hiatal Hernia Treatment
Signup and view all the flashcards
Peptic Ulcer Disease (PUD)
Peptic Ulcer Disease (PUD)
Signup and view all the flashcards
PUD Risk Factors
PUD Risk Factors
Signup and view all the flashcards
PUD Treatment
PUD Treatment
Signup and view all the flashcards
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS)
Signup and view all the flashcards
Crohn’s Disease
Crohn’s Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Colorectal Cancer Symptoms
Colorectal Cancer Symptoms
Signup and view all the flashcards
Colorectal Cancer Detection
Colorectal Cancer Detection
Signup and view all the flashcards
Hepatic Pathologies
Hepatic Pathologies
Signup and view all the flashcards
Liver Functions
Liver Functions
Signup and view all the flashcards
Cirrhosis
Cirrhosis
Signup and view all the flashcards
Pancreatitis Pathophysiology
Pancreatitis Pathophysiology
Signup and view all the flashcards
Study Notes
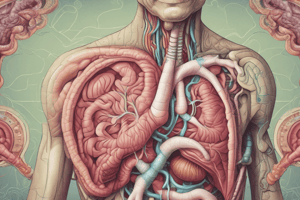
- Module 9 focuses on the digestive system
- Covers content from pages 36-38
Upper Gastrointestinal (UGI) Tract
Gastroesophageal Reflux Disease (GERD)
- Textbook reference pg 949
- A weak esophageal sphincter fails to completely close after food enters the stomach
- This allows stomach acid backflow into the esophagus
- Throat tissue cannot withstand stomach acid
- GERD can result over time from bearing down during bowel movements
- GERD can result from weightlifting while holding breath
- Heartburn results 30-60 minutes after meals due to chyme and gastric acid regurgitation, causing esophagitis which leads to tissue erosion
- Fibrosis (scar tissue) from the healing process does not stretch like esophageal tissue
- Over-the-counter antacids, like Tums or Rolaids, are temporary solutions
- Antacids do not prevent acid release
- Excessive antacid use can cause electrolyte imbalances due to high sodium, calcium, or magnesium content
- Pain worsens when lying down or bending over
- Patients may need to sleep in a recliner or with their head elevated
- GERD pain can mimic a heart attack requiring that patients are taught not to ignore or assume chest pain is heartburn
- Respiratory symptoms can develop if gastric reflux enters the larynx
GERD risk factors
- Obesity
- Pregnancy
- Smoking
- Hiatal hernia
- Fatty foods
- Alcohol
- Chocolate
GERD Treatment (Rx)
- Acid-suppressing medications like omeprazole
- Stop smoking and avoid secondhand smoke
- Limit caffeine intake
- Check for gluten intolerance
- Maintain a high-protein, low-fat diet
- Sleep with the head of the bed elevated
- Stay upright for 2-3 hours after eating
- A "cardiac cocktail", like Mylanta and viscous lidocaine, is administered to ER patients to rule out M.I.
- If pain subsides after the "cocktail", the problem is GI-related, not cardiac
- If pain is worse when lying down, indicative of GERD, not a cardiac issue
- Nissen Wrap/fundoplication surgery is an option for severe reflux, wrapping the stomach's top around the esophagus for a tighter sphincter
- Following surgery, the patient will be unable to vomit or belch air
- GERD can cause precancerous dysplasia (Barrett’s Esophagitis) and can develop into throat cancer
- Patients should be advised to never ignore heartburn, as it can lead to throat cancer
Hiatal Hernia
- Textbook reference pg 949
- Protrusion of the upper stomach through the diaphragm into the thorax causing congestion of blood flow and ischemia
- Pressure weakens the esophageal opening through the diaphragm called the "hiatus"
- Exact causes unknown
- Can be due to weakening of tissue that allows the diaphragm ring to widen
- Increases with age, pregnancy, obesity, habitual vomiting, weight training, and smoking/alcohol
- Very common, especially in people over 50 years old
- Hiatal hernias are commonly asymptomatic unless GERD is also present
- Hiatal hernia pain, similarly to GERD, can mimic a heart attack, where chest pain must be evaluated and tested for cardiac causes first and foremost
- Treatments include acid suppressing medications and potentially surgery if severe
- Endoscopic exam can observe and diagnose a hiatal hernia
Peptic Ulcer Disease (PUD)
- Textbook reference pg 954
- Erosion of the stomach lining
- Helicobacter pylori (H. pylori) is present in >90% in duodenal ulcers, and about 80% of stomach ulcers
- Stress ulcers are common in hospitalized patients (burn trauma, head injuries, critically ill patients)
- Multifactorial, though shock is a known precursor due to low blood perfusion to the stomach
- Proton-pump inhibitor drugs are used, such as I.V. pantoprazole [Protonix]
- Other risk factors include smoking, alcohol use, and NSAID use such as aspirin, ibuprofen, naproxen, etc
- Epigastric (substernal) or chest pain (dull, achy, or sharp) starts about two hours after eating, or in the middle of the night after the stomach has emptied
- Pain is often relieved by eating
- Ulcers can self-resolve or worsen to upper gastrointestinal bleeding or stomach/duodenal perforation
- Common finding in patients with unexplained low hematocrit/hemoglobin
- Main dangers include anemia, profuse bleeding, and stomach cancer
Tests for PUD and UGIB
- CBC
- Hematocrit & Hemoglobin
- H. pylori blood test
- Occult blood smear
- EGD (Esophagogastroduodenoscopy) visualizes and stops a GI bleed
- Biopsy of stomach tissue tests for H. Pylori, during the EGD procedure
- Treatment: Combination Drug Therapy with antibiotics to kill the H. pylori along with acid-suppressing medication
- Active UGIBs can often be cauterized during endoscopy
Types of Ulcers
- Includes duodenal, gastric, and stress
Duodenal Ulcers
- Age: 25-50 years old; any age, usually early adulthood
- Gender: Men > women 3 or 4:1
- Stress factors: N/A According to new research
- Hyperacidity: Increased
- Ulcerogenic drugs: Increased use of ETOH/tobacco
- Associated gastritis: Seldom
- Bacterial infection: Often H. pylori
- Pain: Pain relieved by eating, common nocturnal, remissions and exacerbations
- Hemorrhage: Common
Gastric Ulcers
- Age: 55-70 years old
- Gender: Men > women 3 or 4:1
- Stress factors: N/A According to new research
- Hyperacidity: Normal to low
- Ulcerogenic drugs: Moderate use of ETOH / tobacco
- Associated gastritis: Common
- Bacterial infection: May be present
- Pain: Pain relieved by eating, uncommon nocturnal, no remission and exacerbation
- Hemorrhage: Less common
Stress Ulcers
- Age: Persons with severe stress or trauma (hospitalized patients)*
- Gender: Both genders
- Stress factors: Increased
- Hyperacidity: Increased
- Ulcerogenic drugs: Increased use of ETOH, ASA, NSAID's
- Associated gastritis: Acute and common
- Bacterial infection: Not a factor
- Pain: Asymptomatic until hemorrhage or perforation
- Hemorrhage: Very common
- Stress ulcers are so common in hospitalized patients that they are given an acid-suppressing medication by IV prophylactically with pantoprazole/Protonix
Indications of a GI Bleed
-
Type of blood informs of bleeding source
-
UGIB (upper GI bleed) and LGIB (lower GI Bleeds) can be either slow/chronic with minimal symptoms or sudden and life-threatening
-
Ulcer perforations will cause stomach acid to enter the peritoneal cavity, sudden agonizing pain and a RIGID ABDOMEN, sepsis, and shock
-
Slow ulcer bleeds cause fatigue and anemia
-
Occult GI Bleeding: Positive fecal occult blood test with no visible blood in feces
-
Overt GI Bleeding can manifest as: - Hematemesis - Melena - Hematochezia
-
“Bright red emesis” is a dangerous sign and indicates an emergency
-
“Coffee-ground emesis” is due to partial digestion of blood in the stomach by stomach acids
-
Melena causes black “sticky” stools that look like tar and smell awful caused by blood being partially digested in the small/large intestines which indicates a bleeding site in the stomach or intestines
-
Hematochezia causes bright red blood from the rectum and is typically not a serious problem
Lower Gastrointestinal Tract
Irritable Bowel Syndrome (IBS)
- Textbook, pg. 958
- A "functional gastrointestinal (GI) disorder" with symptoms caused by changes in how the GI tract works
- IBS is a group of symptoms that occur together, not a disease, without damage like in Ulcerative Colitis and Crohn’s disease
- The disorder has physical and mental causes
- Defining characteristic: Pain relieved by defecation
IBS includes other potential contributing factors
- Genetics
- Brain-gut signal problems
- Hypersensitivity to bowel stretching
- Bacterial gastroenteritis
- Overgrowth of normal gut flora
- Altered levels of neurotransmitters
IBS can be related to mental health problems
- Panic disorder
- anxiety
- depression
- post-traumatic stress disorder
- Often found in people who have reported past physical or sexual abuse
- People who have been abused tend to express psychological stress through physical symptoms
- Diagnosed when a person has had abdominal pain or discomfort at least three times a month for the last 3 months without other disease or injury that could explain the pain
- Pain or discomfort affects stool frequency or consistency or be relieved by bowel movement
- Persistent or recurrent abdominal pain, altered bowel function without GI damage, varying complaints of flatulence, bloating, nausea, anorexia, constipation or diarrhea
- Can accompany anxiety or depression
- Treatment: Dietary management is being focused on “FODMAP” foods that seem to cause hyperstimulation of the intestines
- General diet recommendations are to eat smaller, more frequent meals, reduce fat content, avoid dairy/alcohol/caffeine, avoid gas-producing foods
- Other treatment: Stress management, medications (laxatives or antidiarrheal medications as needed; Antidepressants)
Inflammatory Bowel Diseases (IBD)
- Crohn's Disease and Ulcerative Colitis
- “umbrella term” that includes Crohn's Disease (CD) and Ulcerative Colitis (UC) since both diseases produce bowel inflammation
Crohn's Disease
- Textbook, pg 959
- Painful autoimmune disorder with inflammatory lesions anywhere in the G.I. tract that results in malabsorption of vitamins/minerals
- More often found in the ascending colon and terminal ileum
- Lesions involve all layers of the bowel wall and can cause fistulas (tunnels) to other organs or other parts of the body
- Fluid and electrolyte imbalances can result
- Skip lesions are characteristic, where some areas of the bowel are involved, but not all
- “Cobblestone” appearance of intestinal lining is also a characteristic
- Bowel wall becomes congested, thickened, leading to abscesses and fistulas
- Scar tissue interferes with movement of chyme through the intestine.
- Can lead to perforation or obstruction
- Can lead to:
- Malabsorption (folic acid causing anemia, calcium/vitamin D causing bone weakness),
- Fluid and electrolyte imbalance
- Diarrhea and dehydration
- Anal fissures
Ulcerative Colitis
- Autoimmune disease
- Textbook, pg 961
- Manifests as lesions only in the colon, causing chronic dehydration (decreased water reabsorption) and malnutrition
- Affects mucosal layer
- May lead to cavity formation with small hemorrhages and abscesses
- Causes wall of bowel thickens and ulcerations that are fibrotic in later stages
- Ulcerative Colitis may result in:
- Intestinal obstruction
- Dehydration, Fluid, and electrolyte imbalances
- Malabsorption
- Iron deficiency anemia
- Chronic bloody diarrhea mixed with mucus
- Weight loss
- Abdominal cramping and pain
- Nausea, vomiting, and the urge to defecate
- hemorrhage
- toxic megacolon
- High risk for colorectal cancer is increased due to development of dysplasia, which requires frequent colonoscopy screening
Crohn Disease vs. Ulcerative Colitis
- Have similar S/S like abdominal pain, diarrhea, malabsorption of nutrients, dehydration (colon not absorbing water)
- Diagnosed with Colonoscopy and tissue biopsies
- Ulcerative Colitis affects the Large Intestine only to the mucosal layer, no "skip" lesions
- Crohn's Disease affects both the large and small bowel through "skip" lesions and affects the entire bowel wall thickness
- Anal/perianal fistulas are rare with Ulcerative Colitis but common with Crohn's, may require a colostomy
- Bloody stools are common in Ulcerative Colitis but uncommon with Crohn's
- Ulcerative Colitis is treated with Steroids & “-mab” drugs and possibly surgery
- Crohn's Disease can be treated with steroids and "-mab" drugs
- Surgery to remove portions of nonfunctioning colon is common for Crohn's
Colorectal Cancer
- PG. 973
- The second leading cause of cancer-related deaths in the United States and the third most common cancer in men and in women
- https://www.cdc.gov/cancer/colorectal/statistics/index.htm
Colorectal Cancer Risk Factors
- 1 in 20 people will be diagnosed with colon cancer and 1/3 die from this cancer.
- Age: 50 years old or older
- Gender: Greater in men than in women
- Race: Black and Caucasian
- Family History: 25% of colon cancer
- History of Crohn disease or ulcerative colitis
- Diet: Unhealthy fats, refined sugars and flour, low fiber, and low vitamins
- Obesity, lack of exercise, smoking, alcohol consumption
- Rectal cancer is increasing rapidly in the 40 to 50-year age range
Pathophysiology of Colorectal Cancer
- Most colorectal cancers start as a polyp on the inner lining of the colon or rectum
- There are two main types of polyps:
- Adenomatous polyps (adenomas) that sometimes change into cancer which is considered a pre-cancerous condition because of this tendency
- Hyperplastic polyps and inflammatory polyps that are more common, and not pre-cancerous
Signs and Symptoms of Colorectal Cancer in Later Stages
- Changes in bowel movements including constipation or diarrhea
- Feeling unable to empty bowels completely or needing to urgently have a bowel movement
- Rectal bleeding or cramping
- Dark patches of blood in or on stool or long, thin, "pencil stools"
- Abdominal discomfort or bloating
- Unexplained fatigue, loss of appetite, and weight loss
- Pelvic pain
- These later stages may require a diagnosis using fecal occult blood test and colonoscopy
Hepatic Pathologies
Prehepatic Conditions
- Prevent blood from flowing to portal vein
- Thrombosis
- Cancer
- Enlarged Lymph nodes
- Compression
Intrahepatic Conditions
- Occur with the liver itself and cause obstruction of blood flow
- Alcoholic Cirrhosis
Post Hepatic Conditions
- Occur after liver lobules and through hepatic veins
- Right sided heart failure
- Thrombosis of hepatic veins
Mnemonic to Describe Liver Functions
- "People Drink So Much"
Liver Functions
- Produces Albumin that synthesize the oncotic/osmotic pressure in the blood veins, causing Ascites and Portal Hypertension
- Detoxes drugs and medications, causes buildup of bilirubin resulting in jaundice causes transport of bilirubin [blood breakdown byproduct], and cholesterol
- Biliary buildups cause jaundice or hyperlipidemia
- Coagulation Factors: Insufficient clotting factors causes bleeding problems
- Liver stores glycogen and metabolizes protein digested through small intestine so that ammonia byproduct gets metabolized to urea to be excreted by kidneys
Cirrhosis
- Textbook, pg 999
- Scarred liver tissue that does not function normally
- Most common cause is chronic alcohol use resulting in Alcoholic Hepatitis, where production of acetaldehyde from liver damage and ethly alcohol directly damages haptocytes
- Also can be caused by viral Hepatitis and hepatotoxic drugs ie: Acetaminophen
- Cirrhosis prevents proper blood flow through the portal hypertension, causing fluid backup and potential Ascites
Clinical Manifestations of Liver Failure
- Portal hypertension causes obstructive flow in liver, backing up fluids in Portal Veins, resulting in vein and organ engorgement
- As a result, esophageal/stomach varices, splenomegaly, ascites and hemorrhoids manifest
- Free Fluid in the abdomen in cases of ascites causes:
- #1 Portal hypertension increasing capillary hydrostatic pressure, pushing fluid out of the guts of vessels and or,
- Distension, displace diaphragm leading to dyspnea or peritonitis which can be treated through paracentesis
- Hepatitc encephalopathy results in brain changes due to increased levels of toxic ammonia, toxins cross the blood brain barrier and cause disturbances
- Jaundice causes sclera and skin to yellow, and potential anorexia, fatigue, and pruritis, dark urine
- Depleted circulating systems reduces renal function which trigggers angiotensin increases and can cause retention of waste fluids
Diagnostics
- Ascites: Paracentesis procedure that helps draw fluids and relieve intraabdominal pressure or pain
- Lab Test:
- Liver Enzymes being high such as LFT or AST
- Low levels of ammonia can cause encephalopathy
- Abnormal levels of bilirubin and albumin may result in liver damages
- Blood tests can be drawn to test coagulation
Viral Hepatitis
- Pg 991
- Chronic viral hepatitis slowly attacks the liver over many years without causing symptoms
- Signs and symptoms are vague and nonspecific so Hepatitis can go undetected until significant liver damage is present
- An estimated 4.4 million Americans are living with lifelong chronic hepatitis, but are not aware that they are infected
- Signs and symptoms include: fatigue, nausea, vomiting, anorexia, darkened urine, intense icterus/jaundice and related pruritis
- Can be chronic and may cause potential liver cancer
- Liver Damage is therefore more common when testing blood too late
Types of Viral Hepatitis
Hepatitis A
- Most common that comes from oral/fecal transmission through contaminated food
- Vaccine should be given three weeks to contamination, antibody immunoglobulin IgG given after to prevent contracting
Hepatitis B
- Caused by blood-body exposure such as mother-baby contact or shared needles
- Heptavax vaccine* (must complete series of 3); IgGimmunoglobulin and Interferon (Intron-A) can be given to unvaccinated patient
Hepatitis C
- No vaccine available treated most commonly by medicine such as Interferon
- 25 percent are cured from virus
- 75 continue which may be complicated and require the hepatitis C virus
- Note* vaccine should be given to prevent virus and short term IgG antibiotics can also be given to stregthen
Pancreatic Disease
- Pancreatitis
- pg 1008
- Pancreatic injuries where emzymes cause ruptures
- Most common cause alcohol abuse or formation of cists
- Can be stimulated by obstruction and the presence of alcohol where duct becomes damaged and gallstones further cause blockage
- Can cause pain or fever, mimic heartattack or have changed bowel functions
Key Notes
- Most common treatment is not eatting with NG tube and may involve antibiotics
- Bulky fatty stool and oil droplets are very common with this diagnosis
Cholecystitis and the Gallbladder
Cholecystitis
- pg 1006
- Associated with cholethiasis with stores of either bile or cholestoral
- May be inflamed depending on presence of a stone where GB becomes inflamed
Risk Factors
- Fair
- Fat
- Fertile
- Female
- HallMark pain with GB
- Forty
- Pain will occure with GB obstruction
- Family
- Pain caused by inflammation
Signs and Synptons
- Pain as caused by fats, triggering the GB and causing inflammation in the intestine
- Mimmics attacks that cause liver distention and light stools may occure
Treatment
- Change diet, avoid infection
- In severe circumstances may involve Cholecystectomy surgery
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.