Podcast
Questions and Answers
What type of tissue supports the mucosa of the gastrointestinal tract?
What type of tissue supports the mucosa of the gastrointestinal tract?
- Epithelial tissue
- Dense regular connective tissue
- Loose collagenous connective tissue (correct)
- Adipose tissue
What is the function of the muscularis propria in the gastrointestinal tract?
What is the function of the muscularis propria in the gastrointestinal tract?
- Responsible for peristaltic contraction (correct)
- Acts as a barrier to pathogens
- Facilitates nutrient absorption
- Produces digestive enzymes
Which junction is NOT mentioned as an abrupt transition point in the gastrointestinal tract?
Which junction is NOT mentioned as an abrupt transition point in the gastrointestinal tract?
- Gastrooesophageal junction
- Rectoanal junction
- Gastroduodenal junction
- Jejunoileal junction (correct)
How is the adventitia characterized when the gut lies within the abdominal cavity?
How is the adventitia characterized when the gut lies within the abdominal cavity?
What role does the autonomic nervous system play in the gastrointestinal tract?
What role does the autonomic nervous system play in the gastrointestinal tract?
Which layer of the gastrointestinal tract contains the inner oblique layer of muscle?
Which layer of the gastrointestinal tract contains the inner oblique layer of muscle?
What type of muscle contraction follows voluntary muscular action in the gastrointestinal tract?
What type of muscle contraction follows voluntary muscular action in the gastrointestinal tract?
What is the role of goblet cells within the gastrointestinal tract?
What is the role of goblet cells within the gastrointestinal tract?
What hormone is secreted by G cells in the gastric antrum in response to rising gastric pH?
What hormone is secreted by G cells in the gastric antrum in response to rising gastric pH?
Which cells in the gastric glands secrete hydrochloric acid?
Which cells in the gastric glands secrete hydrochloric acid?
What is the primary role of mucous cells in the gastric epithelium?
What is the primary role of mucous cells in the gastric epithelium?
How is acid production by parietal cells physiologically controlled?
How is acid production by parietal cells physiologically controlled?
Which receptor type does acetylcholine act on in parietal cells?
Which receptor type does acetylcholine act on in parietal cells?
In response to increased acid production, which hormone do D cells release to inhibit gastrin secretion?
In response to increased acid production, which hormone do D cells release to inhibit gastrin secretion?
What is essential for the absorption of vitamin B12 in the terminal ileum?
What is essential for the absorption of vitamin B12 in the terminal ileum?
Which cell type in the gastric glands is primarily involved in the secretion of digestive enzymes?
Which cell type in the gastric glands is primarily involved in the secretion of digestive enzymes?
What characterizes the muscularis propria in the oesophagus?
What characterizes the muscularis propria in the oesophagus?
What is the primary role of the myenteric plexus?
What is the primary role of the myenteric plexus?
What initiates the swallowing process?
What initiates the swallowing process?
Which factor does NOT influence sphincter control?
Which factor does NOT influence sphincter control?
What type of epithelium is found at the junction of the oesophagus and the stomach?
What type of epithelium is found at the junction of the oesophagus and the stomach?
What happens to the muscularis mucosae at the oesophago-gastric junction?
What happens to the muscularis mucosae at the oesophago-gastric junction?
What is the primary function of the glandular secretory mucosa in the stomach?
What is the primary function of the glandular secretory mucosa in the stomach?
What structural feature is associated with the muscularis propria in the large intestine?
What structural feature is associated with the muscularis propria in the large intestine?
What initiates the contraction of the smooth muscle in the bowel?
What initiates the contraction of the smooth muscle in the bowel?
Where are parasympathetic ganglia concentrated in the gastrointestinal tract?
Where are parasympathetic ganglia concentrated in the gastrointestinal tract?
Which plexus is responsible for supplying the smooth muscle between the two layers of the muscularis propria?
Which plexus is responsible for supplying the smooth muscle between the two layers of the muscularis propria?
What is the primary mechanism by which food is propelled along the GI tract?
What is the primary mechanism by which food is propelled along the GI tract?
What type of hormones do the diffuse neuroendocrine cells produce?
What type of hormones do the diffuse neuroendocrine cells produce?
Which layer of muscle is responsible for constriction of the luminal diameter in the GI tract?
Which layer of muscle is responsible for constriction of the luminal diameter in the GI tract?
In the enteric nervous system, what structure do parasympathetic efferent fibres primarily synapse with?
In the enteric nervous system, what structure do parasympathetic efferent fibres primarily synapse with?
What role does the longitudinal muscle layer play in the gastrointestinal tract?
What role does the longitudinal muscle layer play in the gastrointestinal tract?
What are the circularly arranged folds in the mucosa and submucosa called?
What are the circularly arranged folds in the mucosa and submucosa called?
Which cell type is primarily responsible for the absorption of nutrients in the small intestine?
Which cell type is primarily responsible for the absorption of nutrients in the small intestine?
Where do reconstituted triglycerides enter after absorption in the small intestine?
Where do reconstituted triglycerides enter after absorption in the small intestine?
What is the primary function of Goblet cells in the small intestine?
What is the primary function of Goblet cells in the small intestine?
Which cell type is characterized by prominent eosinophilic apical granules?
Which cell type is characterized by prominent eosinophilic apical granules?
What separates the muscularis mucosae from the base of the crypts in the small intestine?
What separates the muscularis mucosae from the base of the crypts in the small intestine?
Which type of cells are mostly T cells and help provide defense against invasive organisms?
Which type of cells are mostly T cells and help provide defense against invasive organisms?
What role do neuroendocrine cells play in the small intestine?
What role do neuroendocrine cells play in the small intestine?
Flashcards are hidden until you start studying
Study Notes
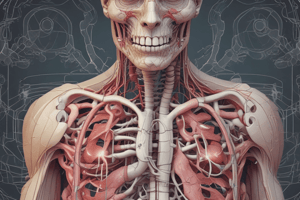
Gastrointestinal Tract Structure
- Abrupt mucosal transitions occur at four junctions: gastrooesophageal, gastroduodenal, ileocaecal, and rectoanal.
- Submucosa consists of loose collagenous connective tissue and houses larger blood vessels, lymphatics, and nerves.
- Muscularis propria features an inner circular and outer longitudinal smooth muscle layer; stomach also includes an inner oblique layer for enhanced peristalsis.
- Adventitia, the outer layer, contains major vessels and nerves and merges with retroperitoneal tissues; lined by serosa (visceral peritoneum) in the peritoneal cavity.
Gastrointestinal Motility
- Food moved primarily by peristalsis, with voluntary muscle action in the mouth, pharynx, and upper oesophagus.
- Peristalsis is involuntary, driven by smooth muscle contractions controlled by the autonomic nervous system and various hormones from neuroendocrine cells.
- The enteric nervous system mediates autonomic regulation, featuring both postganglionic sympathetic and parasympathetic fibers.
Smooth Muscle Control and Function
- Contraction of bowel smooth muscle initiated by interstitial cells of Cajal, primarily modulated by the parasympathetic nervous system.
- Parasympathetic fibers synapse in local ganglia, forming the submucosal (Meissner) and myenteric (Auerbach) plexuses, allowing intricate control of gut motility and secretion.
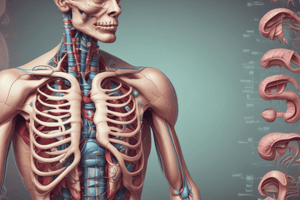
Oesophagus Structure and Function
- Swallowing initiates voluntarily, involving skeletal muscles, followed by peristaltic reflex to push food to the stomach.
- Gastrooesophageal sphincter function is influenced by diaphragmatic contraction, intra-abdominal pressure, and unidirectional peristalsis.
Mucosal Characteristics
- Oesophago-gastric junction features a transition from stratified squamous epithelium to glandular secretory mucosa, enhancing secretion.
- Gastric glands secrete hormones like serotonin, with stem cells in the neck replenishing various cell types continuously.
Gastric Mucosa Details
- Gastric pits lined with surface mucous cells protect the epithelium from digestion by acid.
- Parietal cells secrete hydrochloric acid and intrinsic factor for vitamin B12 absorption.
Gastric Acid Regulation
- Acid secretion is controlled by the autonomic nervous system and hormones: acetylcholine (via vagus nerve), gastrin (from G cells), and histamine (via H2 receptors).
- Somatostatin produced by D cells modulates gastrin secretion in response to gastric pH changes.
Small Intestine Structure and Absorption
- Mucosa has circular folds (plicae circulares) and villi, with enterocytes responsible for absorption through microvilli.
- Peyer’s patches in the lamina propria are significant in immune function within the small intestine.
Cell Types in Small Intestine Epithelium
- Enterocytes (absorptive cells), goblet cells (mucus production), Paneth cells (defense), neuroendocrine cells (motility regulation), and epithelial stem cells (regenerative capacity).
- Intraepithelial lymphocytes (mostly T cells) provide immune defense.
Nutrient Absorption Pathways
- Amino acids and monosaccharides enter capillaries, while triglycerides enter lymphatics (lacteals) bypassing the liver before entering circulation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.