Podcast
Questions and Answers
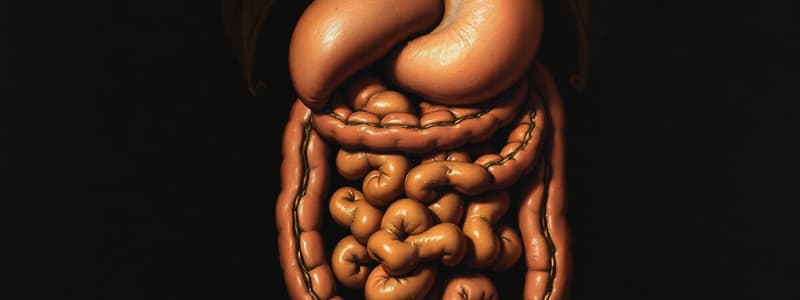
What are the two main functions of the gastrointestinal tract?
What are the two main functions of the gastrointestinal tract?
To digest food and lubricate and protect the mucosa.
What are the two main types of materials secreted in the gastrointestinal tract?
What are the two main types of materials secreted in the gastrointestinal tract?
- Organic materials (correct)
- Inorganic materials
- Water and electrolytes (correct)
- All of the above
What are the two main divisions of the autonomic nervous system that play a role in regulating glanduar secretion?
What are the two main divisions of the autonomic nervous system that play a role in regulating glanduar secretion?
Parasympathetic and sympathetic nervous systems.
Hormones only play a role in stimulating glands to increase secretions.
Hormones only play a role in stimulating glands to increase secretions.
Define the term 'secretion' as it applies to the digestive system.
Define the term 'secretion' as it applies to the digestive system.
What is the essential role of acinar cells in salivary gland secretion?
What is the essential role of acinar cells in salivary gland secretion?
Which salivary gland secretes primarily serous saliva?
Which salivary gland secretes primarily serous saliva?
What is the key event responsible for the initiation of active transport of Cl- ions across the basal membrane of acinar cells?
What is the key event responsible for the initiation of active transport of Cl- ions across the basal membrane of acinar cells?
What causes the flushing of water, electrolytes, and organic materials into the lumen of the acinar cells?
What causes the flushing of water, electrolytes, and organic materials into the lumen of the acinar cells?
Why is the final saliva composition hypotonic?
Why is the final saliva composition hypotonic?
Which of these is NOT a factor that contributes to the control of salivary secretion?
Which of these is NOT a factor that contributes to the control of salivary secretion?
What is the primary trigger for the unconditioned salivary reflex?
What is the primary trigger for the unconditioned salivary reflex?
What is the primary function of salivary amylase?
What is the primary function of salivary amylase?
What are two key functions of saliva that aid in swallowing?
What are two key functions of saliva that aid in swallowing?
Describe one mechanism by which saliva exhibits antibacterial actions.
Describe one mechanism by which saliva exhibits antibacterial actions.
Explain the key function of the simple mucus glands located in the esophagus.
Explain the key function of the simple mucus glands located in the esophagus.
What specific function does the compound mucus glands near the Esophago-Gastric Junction serve?
What specific function does the compound mucus glands near the Esophago-Gastric Junction serve?
Which of these is NOT a function of the viscid mucus secreted by the stomach?
Which of these is NOT a function of the viscid mucus secreted by the stomach?
What is the name given to the tubular glands found in the stomach that produce gastric juice?
What is the name given to the tubular glands found in the stomach that produce gastric juice?
Which type of cell in the oxyntic glands is responsible for secreting hydrochloric acid (HCl)?
Which type of cell in the oxyntic glands is responsible for secreting hydrochloric acid (HCl)?
What is the key mechanism by which Cl- ions are actively transported into the canaliculus of parietal cells?
What is the key mechanism by which Cl- ions are actively transported into the canaliculus of parietal cells?
What is the source of H+ ions that are used to form HCl in the stomach?
What is the source of H+ ions that are used to form HCl in the stomach?
What is the primary mechanism by which H+ ions are actively secreted into the canaliculus of parietal cells?
What is the primary mechanism by which H+ ions are actively secreted into the canaliculus of parietal cells?
Why is the pH in the canaliculus of parietal cells significantly lower than the pH of blood?
Why is the pH in the canaliculus of parietal cells significantly lower than the pH of blood?
What is the key difference between the activities of parietal cells at rest and during high stimulation?
What is the key difference between the activities of parietal cells at rest and during high stimulation?
Besides activating pepsinogen into pepsin, what are two other important functions of HCl in the stomach?
Besides activating pepsinogen into pepsin, what are two other important functions of HCl in the stomach?
What is the inactive form of pepsin, and where is it produced?
What is the inactive form of pepsin, and where is it produced?
What is the primary function of intrinsic factor, and why is it essential for healthy blood formation?
What is the primary function of intrinsic factor, and why is it essential for healthy blood formation?
What are the two main types of cells found in pyloric glands, and what are their functions?
What are the two main types of cells found in pyloric glands, and what are their functions?
Describe the two primary effects of gastrin on the stomach.
Describe the two primary effects of gastrin on the stomach.
Which of these is NOT a mechanism that contributes to the control of gastric secretions?
Which of these is NOT a mechanism that contributes to the control of gastric secretions?
Explain how the parasympathetic nervous system contributes to the stimulation of gastric secretion during the cephalic and gastric phases.
Explain how the parasympathetic nervous system contributes to the stimulation of gastric secretion during the cephalic and gastric phases.
How does the release of gastrin from G cells into the bloodstream impact HCl secretion?
How does the release of gastrin from G cells into the bloodstream impact HCl secretion?
What is the primary stimulus for the release of gastrin from G cells?
What is the primary stimulus for the release of gastrin from G cells?
What is the name of the receptor on parietal cells that gastrin binds to, and what is its effect on the cell?
What is the name of the receptor on parietal cells that gastrin binds to, and what is its effect on the cell?
Explain how histamine contributes to the stimulation of parietal cells to secrete HCl.
Explain how histamine contributes to the stimulation of parietal cells to secrete HCl.
What is the net effect of the combined actions of gastrin, Ach, and histamine on parietal cell HCl secretion?
What is the net effect of the combined actions of gastrin, Ach, and histamine on parietal cell HCl secretion?
What is the primary mechanism by which somatostatin (SS) regulates HCl secretion?
What is the primary mechanism by which somatostatin (SS) regulates HCl secretion?
Describe the two primary ways in which the feedback inhibition of excessive acid production in the stomach occurs.
Describe the two primary ways in which the feedback inhibition of excessive acid production in the stomach occurs.
What is the primary mechanism by which HCl indirectly stimulates pepsinogen secretion by peptic cells?
What is the primary mechanism by which HCl indirectly stimulates pepsinogen secretion by peptic cells?
What are the three key phases that influence the control of gastric secretions?
What are the three key phases that influence the control of gastric secretions?
What are the primary stimuli that trigger the cephalic phase of gastric secretion?
What are the primary stimuli that trigger the cephalic phase of gastric secretion?
Describe the primary stimulus that initiates the gastric phase of gastric secretion.
Describe the primary stimulus that initiates the gastric phase of gastric secretion.
What are the primary stimuli that trigger the intestinal phase of gastric secretion, and what effects do they have?
What are the primary stimuli that trigger the intestinal phase of gastric secretion, and what effects do they have?
What are two of the primary functions of the intestinal epithelium?
What are two of the primary functions of the intestinal epithelium?
Describe the primary function of secretin in the duodenal secretion.
Describe the primary function of secretin in the duodenal secretion.
What is the primary composition of colonic secretions?
What is the primary composition of colonic secretions?
What type of substance are colonic serous secretions particularly rich in?
What type of substance are colonic serous secretions particularly rich in?
What is the primary endocrine function of the islets of Langerhans found in the pancreas?
What is the primary endocrine function of the islets of Langerhans found in the pancreas?
What are the two primary types of secretions produced by the exocrine portion of the pancreas?
What are the two primary types of secretions produced by the exocrine portion of the pancreas?
How are pancreatic secretions delivered to the duodenum?
How are pancreatic secretions delivered to the duodenum?
What are the key characteristics of pancreatic secretions?
What are the key characteristics of pancreatic secretions?
How are pancreatic enzymes initially stored within acinar cells?
How are pancreatic enzymes initially stored within acinar cells?
What enzyme is responsible for activating trypsinogen in the duodenum?
What enzyme is responsible for activating trypsinogen in the duodenum?
What is the primary function of pancreatic amylase in the digestive process, and in what form is it secreted?
What is the primary function of pancreatic amylase in the digestive process, and in what form is it secreted?
What is the primary function of lipase in the digestive process?
What is the primary function of lipase in the digestive process?
Besides lipase, what other factors are typically required for the efficient breakdown of fats in the digestive system?
Besides lipase, what other factors are typically required for the efficient breakdown of fats in the digestive system?
What is the primary physiological role of the bicarbonate ions secreted by the pancreatic duct cells?
What is the primary physiological role of the bicarbonate ions secreted by the pancreatic duct cells?
Describe the mechanism by which bicarbonate ions are secreted by the pancreatic duct cells.
Describe the mechanism by which bicarbonate ions are secreted by the pancreatic duct cells.
What are the primary roles of the parasympathetic and sympathetic nervous systems in regulating pancreatic secretion?
What are the primary roles of the parasympathetic and sympathetic nervous systems in regulating pancreatic secretion?
What is the primary effect of secretin on pancreatic secretion?
What is the primary effect of secretin on pancreatic secretion?
What is the primary effect of CCK on pancreatic secretion?
What is the primary effect of CCK on pancreatic secretion?
What is the role of pancreatic polypeptide in regulating pancreatic secretions?
What is the role of pancreatic polypeptide in regulating pancreatic secretions?
What are the three primary phases involved in regulating pancreatic secretions?
What are the three primary phases involved in regulating pancreatic secretions?
What is the primary function of the liver in the digestive system?
What is the primary function of the liver in the digestive system?
What are five additional functions of the liver besides its role in digestion?
What are five additional functions of the liver besides its role in digestion?
What is the basic functional unit of the liver?
What is the basic functional unit of the liver?
What are three key structures found at the edges of a hepatic lobule?
What are three key structures found at the edges of a hepatic lobule?
What is the primary function of hepatocytes, and where are they located within the hepatic lobule?
What is the primary function of hepatocytes, and where are they located within the hepatic lobule?
What are sinusoids, and what is their significance within the hepatic lobule?
What are sinusoids, and what is their significance within the hepatic lobule?
What is the primary function of the central vein within a hepatic lobule?
What is the primary function of the central vein within a hepatic lobule?
Describe the function of bile canaliculi within a hepatic lobule.
Describe the function of bile canaliculi within a hepatic lobule.
What is the Space of Disse, what is its location, and why is it important?
What is the Space of Disse, what is its location, and why is it important?
Describe the path of blood flow through a hepatic lobule.
Describe the path of blood flow through a hepatic lobule.
What is the primary source of bilirubin, and how is it ultimately excreted?
What is the primary source of bilirubin, and how is it ultimately excreted?
What is jaundice, and what causes it?
What is jaundice, and what causes it?
How does bile aid in the digestion and absorption of lipids in the small intestine?
How does bile aid in the digestion and absorption of lipids in the small intestine?
What are the two primary types of bile acids, and how are they synthesized?
What are the two primary types of bile acids, and how are they synthesized?
What is the enterohepatic circulation, and why is it important?
What is the enterohepatic circulation, and why is it important?
About 80% of bile salts are lost daily in feces.
About 80% of bile salts are lost daily in feces.
Flashcards
What is salivary secretion?
What is salivary secretion?
The movement of water, electrolytes, and proteins (like amylase and glycoproteins) from the salivary gland into the salivary duct.
What are acinar cells?
What are acinar cells?
Specialized cells in salivary glands responsible for secreting the primary saliva solution, containing water, electrolytes, and organic materials.
What is the first step of salivary secretion?
What is the first step of salivary secretion?
The process by which Cl⁻ is actively transported across the basal membrane of acinar cells, creating a negative potential that draws Na⁺ into the cell.
What is the third step of salivary secretion?
What is the third step of salivary secretion?
Signup and view all the flashcards
What is the fourth step of salivary secretion?
What is the fourth step of salivary secretion?
Signup and view all the flashcards
How are protein components of saliva synthesized and secreted?
How are protein components of saliva synthesized and secreted?
Signup and view all the flashcards
What are duct cells?
What are duct cells?
Signup and view all the flashcards
What is the Na⁺/K⁺ pump?
What is the Na⁺/K⁺ pump?
Signup and view all the flashcards
What are the mechanisms of HCO₃⁻ secretion into saliva?
What are the mechanisms of HCO₃⁻ secretion into saliva?
Signup and view all the flashcards
What is the first step of HCl secretion?
What is the first step of HCl secretion?
Signup and view all the flashcards
What is the second step of HCl secretion?
What is the second step of HCl secretion?
Signup and view all the flashcards
What is the third step of HCl secretion?
What is the third step of HCl secretion?
Signup and view all the flashcards
What is the fourth step of HCl secretion?
What is the fourth step of HCl secretion?
Signup and view all the flashcards
What is the importance of HCl in the stomach?
What is the importance of HCl in the stomach?
Signup and view all the flashcards
What is pepsinogen?
What is pepsinogen?
Signup and view all the flashcards
What is pepsin?
What is pepsin?
Signup and view all the flashcards
What is intrinsic factor?
What is intrinsic factor?
Signup and view all the flashcards
What is gastrin?
What is gastrin?
Signup and view all the flashcards
What is the cephalic phase of gastric secretion?
What is the cephalic phase of gastric secretion?
Signup and view all the flashcards
What is the gastric phase of gastric secretion?
What is the gastric phase of gastric secretion?
Signup and view all the flashcards
What is the intestinal phase of gastric secretion?
What is the intestinal phase of gastric secretion?
Signup and view all the flashcards
What is secretin?
What is secretin?
Signup and view all the flashcards
How are pancreatic enzymes secreted?
How are pancreatic enzymes secreted?
Signup and view all the flashcards
What are proteolytic enzymes, and how are they activated?
What are proteolytic enzymes, and how are they activated?
Signup and view all the flashcards
How does pancreatic juice reach the duodenum?
How does pancreatic juice reach the duodenum?
Signup and view all the flashcards
What is the role of water and bicarbonate in pancreatic secretion?
What is the role of water and bicarbonate in pancreatic secretion?
Signup and view all the flashcards
How are bile salts synthesized?
How are bile salts synthesized?
Signup and view all the flashcards
How are bile salts stored and concentrated?
How are bile salts stored and concentrated?
Signup and view all the flashcards
How is bile released into the duodenum during a meal?
How is bile released into the duodenum during a meal?
Signup and view all the flashcards
Study Notes
Gastrointestinal Secretion
- Secretions in the GI tract are a response to food, varying with food type.
- Secretions digest food and protect the mucosa.
Composition of Secretions
- Organic Materials: Synthesized by cells, stored in vesicles, released upon stimulation.
- Water and Electrolytes: Taken from blood vessels, secreted by cells.
Types of Secretory Glands
- Single-cell: Goblet cells
- Pits: Crypts of Lieberkühn (small intestine), Tubular glands (stomach)
- Complex: Mucus glands (lower esophagus)
- Organs: Salivary glands, Pancreas, Liver
Regulation of Glandular Secretion
- Food presence stimulates glandular secretions.
- Mechanical or chemical stimulation activates secretory reflexes.
Role of the Autonomic Nervous System
- Parasympathetic stimulation increases glandular secretions.
- Sympathetic stimulation moderately increases secretion by increasing vesicular transport and reducing water and electrolyte secretion by lowering blood flow.
Hormonal Regulation
- Certain hormones respond to food presence in digestive organs to increase secretions.
Salivary Glands Secretion
- Defined as the net movement of water, electrolytes, and proteins (amylase, glycoproteins) into the lumen of the salivary duct.
- Acinar cells secrete water and electrolytes from extracellular fluid.
Proposed Steps of Secretion
- Active transport of Cl- increases membrane negativity.
- Attracts Na+ ions.
Osmotic Pressure Increase
- Elevated osmotic pressure draws water into acinar cells, increasing hydrostatic pressure.
- Rupture of apical membrane flushes water, electrolytes, and organic materials into the lumen.
Synthesis and Secretion of Protein Components
- Proteins (ptyalin, lingual lipase, mucin) are synthesized in the endoplasmic reticulum and transferred to the apical membrane by exocytosis.
- Secretory cells are rich in ER and mitochondria, providing energy for process.
- Acinar cells secrete a primary solution of ptyalin, mucin, and electrolytes.
- Comparable to extracellular fluid.
Role of Duct Cells in Saliva Composition
- Modification of ionic composition as saliva passes through ducts.
- Na+ reabsorption and K+ secretion.
Secretion into the Duct
- Exchange of HCO3- for Cl- ions.
- Active transport of HCO3-.
Final Saliva Composition
- Hypotonic due to Na+ and Cl- reabsorption exceeding K+ and HCO3- secretion.
- Reduced Na+ and Cl- concentrations, increased K+ and HCO3- concentrations compared to plasma.
Salivary Gland Contribution
- Parotid glands (~25%): Serous saliva
- Submandibular glands (~70%): Mixed saliva (serous and mucous)
- Sublingual glands (~5%): Mucous saliva.
pH of Saliva
- Resting secretion: ~7.0
- Active secretion: ~8.0
Changes in Saliva During Stimulation
- Primary saliva production can increase up to 20-fold due to heightened acinar cell activity.
- Increased flow reduces reabsorptive and secretory activity of duct cells.
Impact on Secondary Saliva Composition
- Higher Na+, Cl- concentrations; lower K+ concentrations compared to lower flow rates.
Control of Salivary Secretion
- Aldosterone
- Unconditioned reflex: Triggered by chemo/pressure receptors in the oral cavity (eating, dental procedures). Receptors send signals, and autonomic nerves increase salivation.
- Conditioned reflex: Triggered by stimuli like thinking about food (learned responses).
- Nervous regulation: Both sympathetic and parasympathetic systems stimulate, but via different mechanisms. High sympathetic activity might reduce salivation.
Functions of Saliva
- Carbohydrate digestion: Salivary amylase breaks down polysaccharides to maltose
- Swallowing: Moistens food, lubrication to reduce friction during swallowing.
Antibacterial Actions
- Lysozyme: Destroys bacteria
- Continuous saliva flow: Rinses away debris
- Immunoglobulin A (IgA): Contributes to bacterial destruction
Taste Facilitation
- Saliva is a solvent for taste bud stimulation.
Speech Aid and Neutralisation of Acids
- Enables smooth lip/tongue movements.
- Bicarbonate neutralizes acidic food/bacteria, helping prevent dental caries.
Esophageal Secretion
- Simple mucus glands lubricate and protect the mucosa from damage during swallowing.
- Compound mucus glands (near esophagogastric junction) secrete alkaline mucus to protect against gastric reflux.
Gastric Secretion
- Mucus-secreting cells line the stomach surface. Lubricates, protects, and neutralizes HCl, preventing injury.
Tubular Glands (Oxyntic Glands)
- Secrete HCl, intrinsic factor, and mucus.
- Contains mucus neck cells, peptic cells, parietal cells.
Mechanism of HCl Secretion
- Chloride active transport creates negative potential, driving K+ diffusion primarily.
- Formation of H+ from water/CO2 reaction catalyzed by carbonic anhydrase.
- Bicarbonate exchanged for chloride.
- H+ actively secreted via the H+/K+ pump.
- Water enters via osmosis.
Net Reaction
- Water, CO2, and NaCl form NaHCO3 (blood) and HCl (lumen).
Importance of HCl
- Activates pepsinogen to pepsin
- Decomposes connective tissue
- Kills microorganisms
Pepsinogen Secretion
- Secreted by chief/mucus cells, inactive
- Converted to pepsin in acidic environments (pH 1.8-3.5)
Importance of Pepsin
- Breaks down polypeptides into smaller peptides.
Intrinsic Factor Secretion
- Secreted by parietal cells, necessary for vitamin B12 absorption.
- Its insufficiency causes pernicious anemia (impaired RBC maturation).
Pyloric Glands
- Contain mucus cells (similar to gastric glands) and G cells (secrete gastrin).
Gastrin
- Released into blood, acting on the stomach to increase HCl and pepsinogen secretion and maintain gastric mucosal growth.
Control of Gastric Secretion
-
Neural: Enteric nervous system and parasympathetic (vagal) activation during cephalic and gastric phases; releasing ACh, VIP, GRP.
-
Hormonal: Gastrin released from G cells
Histamine
- Secreted by enterochromaffin-like cells, enhancing HCl secretion (paracrine).
Somatostatin
- Released from paracrine cells, inhibiting HCl secretion.
Regulation of Pepsinogen Secretion
- HCl, gastrin stimulate enteric reflexes increasing pepsinogen secretion by peptic cells.
Phases of Gastric Secretion
- Cephalic phase: Thinking about, smelling, or tasting food stimulates parietal and G cells.
- Gastric phase: Food in the stomach causes maximal stimulation of gastric secretions due to distension and protein presence.
- Intestinal phase: Distension of the upper duodenum might slightly stimulate secretion. Presence of fats, acids, and hormones (GIP, CCK, secretin, enterogastrone) inhibit secretions.
Intestinal Secretion
- Cells of mucosal epithelium secrete mucus, water, and electrolytes.
- Tubular glands (crypts of Lieberkühn) secrete serous secretions rich in K+ and HCO3-.
- Local neural mechanisms and hormones (secretin) regulate secretion.
Pancreatic Secretion
- Endocrine portion (Islets of Langerhans): Secretes insulin, glucagon, somatostatin, and pancreatic polypeptide into the blood.
- Exocrine portion (acinus and duct cells): Secretes enzymes (trypsinogen, chymotrypsinogen, procarboxypeptidase, amylase, lipase), water, and bicarbonate into the duodenum through the pancreatic duct.
Secretion of Pancreatic Enzymes
- Synthesised/stored by acinar cells
- Released as inactive forms (e.g. trypsinogen) activated in the duodenum.
- Proteolytic enzymes, pancreatic amylase (polysaccharide breakdown), lipolytic enzymes (lipases - triglycerides breakdown)
Secretion of Water and Bicarbonate
- Water and bicarbonate secreted by duct cells
- Acid neutralization for enzymatic function
Mechanism of Pancreatic Secretion
- Carbonic anhydrase catalyzes water/CO2 to generate H+ and HCO3-
- HCO3- exchanged for Cl- at the luminal border.
- H+ transported by secondary active transport exchanging with Na+..
- Na+ actively transported out of the cell.
- Water follows osmotically.
Regulation of Pancreatic Secretion
- Neural: Parasympathetic (vagal) stimulation is excitatory while sympathetic has an indirect inhibitory effect.
- Hormonal: Secretin major stimulant for water and HCO3- secretion, responding to acid in the duodenum.
CCK (Cholecystokinin)
- Major stimulant for enzyme secretion from acinar cells; responds to fats and proteins; indirectly stimulates enzyme secretion through vagovagal reflex; stimulates contraction of gallbladder and relaxation of Oddi sphincter.
Pancreatic Polypeptide
- Inhibits the release of enzymes through CNS and vagovagal pathway.
Liver Secretions
- Liver is the largest and most metabolically active organ
- Functions include: Detoxification, metabolic processing, protein synthesis, storage, and excretion.
Bile Secretion and Excretion
- Hepatocytes produce bile containing bile acids, salts, cholesterol.
- Bile is stored/concentrated in the gallbladder.
- Bile released into the duodenum, emulsifies fats (increasing surface area), and absorbs fat-soluble vitamins
Bile Synthesis and Secretion
- Liver produces bile acids from cholesterol.
- Primary bile acids (cholic acid, chenodeoxycholic acid) modified into bile salts.
- Bacteria in the intestines modify primary bile acids into secondary bile acids (deoxycholic acid, lithocholic acid).
- Bile salts are reabsorbed and recycled, but a small amount is lost daily, and new synthesis replaces it.
Bile Composition
- Varies with presence of fats and proteins in duodenum triggering CCK and secretin release.
Enterohepatic Circulation
- Bile salts reabsorbed, returned to liver, and reused in bile production.
- Bile salts reenter circulation after digestion, allowing recycling and saving this energy for the body.
Hepatic Lobule Structure
- Functional unit composed of hepatocytes arranged around a central vein with hepatic artery and portal vein branches entering at the edges.
- Special structure and functions of specialized structures such as sinusoids, bile canaliculi, and space of Disse.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.