Podcast
Questions and Answers
Which of the following is NOT a primary function of the physical barriers found in the GI tract?
Which of the following is NOT a primary function of the physical barriers found in the GI tract?
- Facilitating nutrient absorption into the bloodstream. (correct)
- Modulating the composition of the gut microbiome.
- Limiting access of antigens to the immune system.
- Preventing the entry of harmful pathogens.
What is the primary role of intraepithelial lymphocytes (IELs) in the gut?
What is the primary role of intraepithelial lymphocytes (IELs) in the gut?
- Regulating inflammatory responses initiated by mast cells.
- Providing immediate cytotoxic responses and maintaining epithelial cell integrity. (correct)
- Producing large quantities of secreted IgA.
- Activating systemic immune responses upon pathogen encounter.
Which of the following statements accurately describes the transport of IgA into the gut lumen?
Which of the following statements accurately describes the transport of IgA into the gut lumen?
- IgA is secreted directly into the lumen by plasma cells.
- IgA diffuses passively through the tight junctions of the epithelial cells.
- IgA is transported across the epithelial cells in a vesicle, mediated by the polymeric Ig receptor (pIgR). (correct)
- IgA is actively transported by specialized cells called M cells.
What is the primary mechanism of oral tolerance in the gastrointestinal tract?
What is the primary mechanism of oral tolerance in the gastrointestinal tract?
Which of the following cell types is NOT typically associated with the mucosal immune response in the GI tract?
Which of the following cell types is NOT typically associated with the mucosal immune response in the GI tract?
Where are B cells initially activated in the context of mucosal immunity?
Where are B cells initially activated in the context of mucosal immunity?
Which antibody isotype is primarily associated with mucosal immunity in the gut?
Which antibody isotype is primarily associated with mucosal immunity in the gut?
Which structure is responsible for transporting IgA across the epithelial cell to the mucosal surface?
Which structure is responsible for transporting IgA across the epithelial cell to the mucosal surface?
What is the primary function of IgA antibodies in the gut lumen?
What is the primary function of IgA antibodies in the gut lumen?
After activation in the Peyer's patches, where do B cells travel to next?
After activation in the Peyer's patches, where do B cells travel to next?
What is the role of IgA in relation to small pathogens?
What is the role of IgA in relation to small pathogens?
Where do mature plasma cells that produce IgA ultimately reside?
Where do mature plasma cells that produce IgA ultimately reside?
What is a primary function of mucosal immunity?
What is a primary function of mucosal immunity?
What is a primary function of FcαR binding by eosinophils within the context of gastrointestinal (GI) immunology?
What is a primary function of FcαR binding by eosinophils within the context of gastrointestinal (GI) immunology?
Compared to serum antibody responses, how does mucosal immune memory typically behave?
Compared to serum antibody responses, how does mucosal immune memory typically behave?
Which of the following best describes the typical duration of protection offered by mucosal antibody responses against pathogens like rotavirus or RSV?
Which of the following best describes the typical duration of protection offered by mucosal antibody responses against pathogens like rotavirus or RSV?
What outcome is typically seen when a high dose of an antigen is administered through the gastrointestinal tract?
What outcome is typically seen when a high dose of an antigen is administered through the gastrointestinal tract?
How does a low dose of oral antigen typically influence the immune response?
How does a low dose of oral antigen typically influence the immune response?
After M cells phagocytose an antigen from the gut lumen, where is the antigen initially transported?
After M cells phagocytose an antigen from the gut lumen, where is the antigen initially transported?
What type of cells are primarily stimulated by antigen presenting cells in the Peyer's patches during a mucosal immune response?
What type of cells are primarily stimulated by antigen presenting cells in the Peyer's patches during a mucosal immune response?
Following activation in the Peyer's patch, where do CD4+ T cells traffic next?
Following activation in the Peyer's patch, where do CD4+ T cells traffic next?
What type of cells do CD4+ T cells mature into after trafficking through the bloodstream in the context of the gut immune response?
What type of cells do CD4+ T cells mature into after trafficking through the bloodstream in the context of the gut immune response?
Where do plasma cells that have been stimulated in the gut, ultimately return to?
Where do plasma cells that have been stimulated in the gut, ultimately return to?
Which antibody isotype is primarily produced by plasma cells in the gut lamina propria in response to luminal antigens?
Which antibody isotype is primarily produced by plasma cells in the gut lamina propria in response to luminal antigens?
Which of the following best describes the initial immune response in Ulcerative Colitis (UC)?
Which of the following best describes the initial immune response in Ulcerative Colitis (UC)?
What is the primary role of IgA in the gut lumen?
What is the primary role of IgA in the gut lumen?
What is the primary characteristic of the inflammatory lesions seen in Crohn's Disease?
What is the primary characteristic of the inflammatory lesions seen in Crohn's Disease?
Which cells are responsible for initial phagocytosis of antigens in the gut lumen?
Which cells are responsible for initial phagocytosis of antigens in the gut lumen?
What is the mechanism of action of Infliximab in treating Crohn's disease?
What is the mechanism of action of Infliximab in treating Crohn's disease?
A failure in which cellular process is implicated in the pathogenesis of Crohn's disease?
A failure in which cellular process is implicated in the pathogenesis of Crohn's disease?
Approximately how large is the mucosal surface area of the gastrointestinal tract?
Approximately how large is the mucosal surface area of the gastrointestinal tract?
What is a common surgical intervention for Crohn's disease?
What is a common surgical intervention for Crohn's disease?
Which of the following is NOT a characteristic of the mucosal surface of the GI tract?
Which of the following is NOT a characteristic of the mucosal surface of the GI tract?
Regarding the development of Inflammatory Bowel Disease (IBD), what is the prevailing theory?
Regarding the development of Inflammatory Bowel Disease (IBD), what is the prevailing theory?
What is the approximate number of commensal bacteria that reside in the gut compared to the number of cells in the human body?
What is the approximate number of commensal bacteria that reside in the gut compared to the number of cells in the human body?
Which condition is characterized by relatively superficial inflammation limited to the large bowel?
Which condition is characterized by relatively superficial inflammation limited to the large bowel?
What is a common complication of Crohn's disease related to the formation of abnormal connections?
What is a common complication of Crohn's disease related to the formation of abnormal connections?
Which of the following is NOT a component of the GI lymphoid tissue?
Which of the following is NOT a component of the GI lymphoid tissue?
What is the most abundant antibody isotype found in the GI tract?
What is the most abundant antibody isotype found in the GI tract?
Which of the following is NOT a key factor in the 'perfect storm' leading to Inflammatory Bowel Disease?
Which of the following is NOT a key factor in the 'perfect storm' leading to Inflammatory Bowel Disease?
Why might immunosuppressants be necessary when using Infliximab?
Why might immunosuppressants be necessary when using Infliximab?
Which mechanism does NOT help to limit uncontrolled bacterial growth in the gut?
Which mechanism does NOT help to limit uncontrolled bacterial growth in the gut?
What does GALT stand for regarding the immune system?
What does GALT stand for regarding the immune system?
Which of the following is NOT a component of the Gut-associated Lymphoid Tissue (GALT)?
Which of the following is NOT a component of the Gut-associated Lymphoid Tissue (GALT)?
What is the primary function of Peyer's patches?
What is the primary function of Peyer's patches?
Which specialized epithelial cell type is responsible for transporting antigens from the gut lumen to the Peyer's patches?
Which specialized epithelial cell type is responsible for transporting antigens from the gut lumen to the Peyer's patches?
What is a key characteristic of M cells in the Peyer's patches?
What is a key characteristic of M cells in the Peyer's patches?
Which process do M cells use to uptake antigens from the gut lumen?
Which process do M cells use to uptake antigens from the gut lumen?
Which of the following pathogens can enter through M cells to cause disease?
Which of the following pathogens can enter through M cells to cause disease?
Intraepithelial lymphocytes (IELs) are primarily what type of cells?
Intraepithelial lymphocytes (IELs) are primarily what type of cells?
What is the primary function of CD8+ intraepithelial lymphocytes (IELs)?
What is the primary function of CD8+ intraepithelial lymphocytes (IELs)?
Flashcards
Mucosal Immunity
Mucosal Immunity
The immune system's response to pathogens in the gut, characterized by specialized cells and mechanisms that protect against infection.
Gut-Associated Lymphoid Tissue (GALT)
Gut-Associated Lymphoid Tissue (GALT)
The collection of lymphoid tissues in the gut including Peyer's patches, mesenteric lymph nodes, and isolated lymphoid follicles.
Peyer's Patches
Peyer's Patches
Specialized lymphoid tissues in the small intestine that sample antigens from the gut lumen and initiate immune responses.
IgA (Immunoglobulin A)
IgA (Immunoglobulin A)
Signup and view all the flashcards
Oral Tolerance
Oral Tolerance
Signup and view all the flashcards
Immune Memory
Immune Memory
Signup and view all the flashcards
Immunization via the GI tract
Immunization via the GI tract
Signup and view all the flashcards
Regulatory T Cells (Treg)
Regulatory T Cells (Treg)
Signup and view all the flashcards
Mucosal Immunity of the GI Tract
Mucosal Immunity of the GI Tract
Signup and view all the flashcards
IgA Transcytosis
IgA Transcytosis
Signup and view all the flashcards
IgA
IgA
Signup and view all the flashcards
How IgA Protects the GI Tract
How IgA Protects the GI Tract
Signup and view all the flashcards
IgA Trafficking
IgA Trafficking
Signup and view all the flashcards
Food-Induced Allergic Reactions
Food-Induced Allergic Reactions
Signup and view all the flashcards
What is the surface area of the GI tract?
What is the surface area of the GI tract?
Signup and view all the flashcards
How many kinds of bacteria are in the GI tract?
How many kinds of bacteria are in the GI tract?
Signup and view all the flashcards
What are the characteristics of the GI tract epithelium?
What are the characteristics of the GI tract epithelium?
Signup and view all the flashcards
What are the key immune cells found in the GI lymphoid tissue?
What are the key immune cells found in the GI lymphoid tissue?
Signup and view all the flashcards
What is the main function of the GI lymphoid tissue?
What is the main function of the GI lymphoid tissue?
Signup and view all the flashcards
Where are effector T cells and plasma cells located?
Where are effector T cells and plasma cells located?
Signup and view all the flashcards
Compare the lymphocyte count in the GI tract with other lymphoid organs.
Compare the lymphocyte count in the GI tract with other lymphoid organs.
Signup and view all the flashcards
Which antibody is most prevalent in the GI tract?
Which antibody is most prevalent in the GI tract?
Signup and view all the flashcards
How does the GI tract physically control bacterial growth?
How does the GI tract physically control bacterial growth?
Signup and view all the flashcards
What are the elements of the GI tract's barrier?
What are the elements of the GI tract's barrier?
Signup and view all the flashcards
What are the components of GALT?
What are the components of GALT?
Signup and view all the flashcards
What is the function of M cells in Peyer's patches?
What is the function of M cells in Peyer's patches?
Signup and view all the flashcards
What are M cells and where are they found?
What are M cells and where are they found?
Signup and view all the flashcards
How do M cells initiate immune responses?
How do M cells initiate immune responses?
Signup and view all the flashcards
How do pathogens enter the gut?
How do pathogens enter the gut?
Signup and view all the flashcards
What are M cells?
What are M cells?
Signup and view all the flashcards
What are Peyer's patches?
What are Peyer's patches?
Signup and view all the flashcards
What role do CD4+ T cells play in gut immunity?
What role do CD4+ T cells play in gut immunity?
Signup and view all the flashcards
What is the role of the lymph nodes in gut immunity?
What is the role of the lymph nodes in gut immunity?
Signup and view all the flashcards
What are IgA-producing plasma cells?
What are IgA-producing plasma cells?
Signup and view all the flashcards
What is oral tolerance?
What is oral tolerance?
Signup and view all the flashcards
What is the role of IgA in gut immunity?
What is the role of IgA in gut immunity?
Signup and view all the flashcards
What is the mucosal immune response?
What is the mucosal immune response?
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
TNF-α
TNF-α
Signup and view all the flashcards
Infliximab
Infliximab
Signup and view all the flashcards
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD)
Signup and view all the flashcards
Study Notes
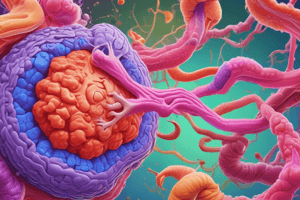
Immunology of the GI Tract
- The GI tract has a large mucosal surface area, approximately equal to a tennis court (300 m²).
- This surface area is covered in moist, nutrient-rich, non-keratinized tissue.
- It is colonized by a diverse bacterial flora.
- The gut's immune system works in balance with the bacteria to prevent infection. There are approximately 400 species of commensal bacteria in the gut, numbering 1014, which is 10 times the number of cells in the human body.
- The GI lymphoid tissue includes T cells, B cells, and antigen-presenting cells involved in immune induction and function.
- Epithelial layers and mucus secretions help limit uncontrolled bacterial growth.
- High acidity in the stomach also contributes to controlling bacteria.
Learning Objectives
-
Understanding the need for mucosal immunity, general characteristics of the GI tract mucosal immune response, and physical mechanisms acting as barriers to infection.
-
Description of the lymphoid tissue in the GALT (gut-associated lymphoid tissue), characterizing the architecture of structures like Peyer's patches, and the role of intraepithelial and lamina propria lymphocytes.
-
The steps involved in the GI tract's immune response, including IgA transport into the lumen and its role in preventing infection.
-
The role of various immune mediators, including γδ T cells, mast cells, cytotoxic T lymphocytes, and mucosal epithelial cells.
-
The significance of oral tolerance to typical food proteins, how self-tolerance is achieved, and potential therapeutic uses of tolerance in autoimmune disease.
-
Overview of common GI diseases with likely immunologic etiologies, including clinical manifestations and their involvement with the immune system.
Gut-Associated Lymphoid Tissue (GALT)
- GALT includes Peyer's patches, appendix, and lymphoid aggregates located in the appendix, large intestine, and lamina propria.
- It consists of distinct B cell follicles and T cell zones, where immune responses are initiated in the gut.
Peyer's Patches
- Located in the lamina propria near specialized epithelial cells.
- These cells transport small amounts of antigens from the gut lumen.
- This allows the immune system to sample antigens passing through the gut.
- Important for promoting IgA production and CTL responses.
M Cells
- Specialized epithelial cells that interface between the gut lumen and Peyer's patches.
- Transfer antigens via endocytosis or phagocytosis.
- Interact directly with underlying antigen-presenting cells (APCs).
- APCs present antigens to T cells to stimulate immune responses.
- Have micro-folds.
Pathogens and M Cells
- Some pathogens (Salmonella, Yersinia, Listeria, and Shigella) enter through M cells.
- They trigger phagocytosis or macropinocytosis.
Intraepithelial Lymphocytes (IELs)
- Found at a ratio of one IEL for every 4–6 epithelial cells.
- Primarily T cells, with >90% being αβ or γδ types.
- CD8+ IELs have cytotoxic function and cell-mediated immunity against intracellular bacteria and viruses.
Gamma Delta T Cells
- A type of T cell bearing a γδ T cell receptor instead of an αβ receptor.
- A significant percentage of IELs in the GI tract.
- Recognize nonpeptide molecules (like antigens, heat-shock proteins, nucleotides, and phospholipids) presented on MHC class I-like molecules (CD1).
Lamina Propria Immune Cells
- The lamina propria contains a diverse array of immune cells, including: CD4+ T cells (including Tregs), B cells and plasma cells, macrophages, dendritic cells, eosinophils, and mast cells.
Dendritic Cells Activating CD4+ T Cells
- Dendritic cells activate CD4+ T cells, which in turn activate B cells.
- This process involves antigen uptake, antigen presentation to T cells, and T cell activation of B cells.
Mast Cells
- Line epithelia (e.g., lungs, GI tract, skin) exposed to the environment.
- Involved in IgE-mediated defense against parasites.
- Elicit food-induced allergic reactions, including diarrhea, anaphylactic shock.
Peyer's Patch Stimulated B Cells
- B cells activated in Peyer's patches or lymph nodes.
- Drain through mesenteric lymph nodes as plasmablasts, entering the bloodstream.
- Mature plasma cells return to the lamina propria and produce IgA.
- IgA is transported into the gut lumen.
Plasma Cells Producing IgA
- Plasma cells in the lamina propria produce IgA.
- IgA binds to poly-immunoglobulin receptors (pIgR), is transported across the cell, and delivered to the mucosal surface.
- IgA binds to microbes to prevent access to the epithelium and promote clearance.
IgA Facilitating Pathogen Clearance
- Prevents microbial binding to epithelial cells.
- Opsonizes pathogens for phagocytosis by cells like eosinophils.
- Leads to degranulation and anti-parasite immunity.
Mucosal Memory
- Mucosal immune memory is shorter than serum memory.
- Mucosal antibody responses (e.g., to rotavirus, RSV, and rhinoviruses) are typically short-lived (months to years).
- Serum antibody responses may persist for decades (e.g., measles, mumps protections).
Oral Tolerance
- Immunization with antigen via the GI tract can induce systemic unresponsiveness.
- Used to prevent hypersensitivity reactions to ingested food proteins.
- High doses can lead to antigen-specific lymphocyte deletion.
- Low doses can lead to clonal anergy and regulatory T cell suppression.
- Regulatory T cells developed in GALT migrate systemically.
- Human trials are being done for autoimmune diseases (multiple sclerosis, rheumatoid arthritis, type I diabetes, and uveitis).
Selective IgA Deficiency
- Most common immunodeficiency in humans.
- Typically not clinically significant because IgM compensates.
- Associated with a higher risk of autoimmune disease.
Food Hypersensitivities
- Some reactions to food proteins result from IgE-mediated immediate hypersensitivity reactions.
- Symptoms can include nausea, vomiting, abdominal pain, skin rashes, pharyngeal edema, and bronchospasm (potentially fatal anaphylaxis).
- Reactions of some food hypersensitivities causing changes in vascular permeability, massive protein loss, enteropathy, and hypoalbuminemia.
Gluten-Sensitive Enteropathy
- Also known as celiac disease or idiopathic, sprue.
- A disease affecting the small intestine.
- Gluten-sensitive enteropathy is characterized by malabsorption due to villous atrophy.
- Due to hypersensitivity to gliadin (a protein family in wheat gluten).
- Epithelial cell lining (though intact) abnormally functions, which is limited to the small intestine since gliadin isn't broken down.
- Treatment includes a lifelong gluten-free diet, which can lead to increased incidence of lymphoma or carcinoma in untreated cases.
Ulcerative Colitis
- Inflammation is confined to the large intestine.
- Characterized by ulcer formation and loss of mucosal absorptive function.
- Anti-inflammatory or immunosuppressive therapy might not control disease.
- Necessary to perform a total colectomy for some cases.
Crohn's Disease
- Inflammatory and granulomatous lesions can affect various parts of the GI tract (particularly the terminal ileum and ascending colon).
- Characterized by obstructive symptoms, fistula formation, and involvement of other organs (i.e., from bowel to other organs).
- Failure of inflammatory macrophages to die from apoptotic mechanisms can lead to problems.
TNF-α and Crohn's Disease
- TNF-α plays an important role.
- Infliximab (a TNF-α inhibitor) blocks TNF-α activity and can reduce symptoms of disease.
- Treatment requires immunosuppressants.
- Surgery (segmental resection) may be necessary, but disease often recurs.
Immunologic Basis of Inflammatory Bowel Disease (IBD)
- Diffuse lymphocyte infiltrate and, later, granulomatous formation.
- Derangement in mucosal immunoregulation permits the development of immune responses to normally ignored mucosal antigens.
Developing a Mucosal Immune Reaction
- Antigen phagocytosis and its transport into cells (M cells).
- Antigen presentation and activation of CD4+ T cells.
- CD4+ T cell stimulation of B cells.
- B cell traffic to lymph nodes, bloodstream maturation into plasma cells.
- Plasma cells returning to the lamina propria to produce IgA, with subsequent transport to the gut lumen for pathogen neutralization.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.