Podcast
Questions and Answers
Which of the following is NOT considered a part of the upper gastrointestinal tract?
Which of the following is NOT considered a part of the upper gastrointestinal tract?
- Jejunum (correct)
- Esophagus
- Mouth
- Stomach
Which imaging modality is typically used to initially assess for gallstones?
Which imaging modality is typically used to initially assess for gallstones?
- MRI
- KUB X-ray
- Ultrasound (correct)
- CT scan
When performing an acute abdominal series on a patient who is unable to stand, which of the following views is typically included?
When performing an acute abdominal series on a patient who is unable to stand, which of the following views is typically included?
- AP supine, left lateral decubitus, and AP chest (correct)
- AP supine, PA upright, and lateral decubitus
- AP supine, PA upright, and AP spine
- PA upright, right lateral decubitus, and AP chest
Which of the following best describes the primary indication for performing a KUB (kidneys, ureters, bladder) X-ray?
Which of the following best describes the primary indication for performing a KUB (kidneys, ureters, bladder) X-ray?
In which clinical scenario would a water-soluble contrast be preferred over barium contrast for an upper GI series?
In which clinical scenario would a water-soluble contrast be preferred over barium contrast for an upper GI series?
What is the typical imaging frequency until the contrast reaches the terminal ileum in an upper GI series with small bowel follow-through?
What is the typical imaging frequency until the contrast reaches the terminal ileum in an upper GI series with small bowel follow-through?
What is the primary indication for performing a lower GI series?
What is the primary indication for performing a lower GI series?
In abdominal X-rays, what does 'dense stuff' typically refer to?
In abdominal X-rays, what does 'dense stuff' typically refer to?
What feature differentiates normal small bowel from normal large bowel on abdominal X-ray?
What feature differentiates normal small bowel from normal large bowel on abdominal X-ray?
What is the 'rule of 3-6-9' used for in the context of abdominal imaging?
What is the 'rule of 3-6-9' used for in the context of abdominal imaging?
Extraluminal air is considered rarely normal on abdominal X-ray, except in which scenario?
Extraluminal air is considered rarely normal on abdominal X-ray, except in which scenario?
Which of the following is NOT a typical indication for performing a CT scan of the abdomen?
Which of the following is NOT a typical indication for performing a CT scan of the abdomen?
Why is it important to know a female patient's pregnancy status before performing a CT scan of the abdomen?
Why is it important to know a female patient's pregnancy status before performing a CT scan of the abdomen?
When is it necessary to know a patient's renal function before administering IV iodinated contrast for a CT scan?
When is it necessary to know a patient's renal function before administering IV iodinated contrast for a CT scan?
For ultrasound imaging of the gallbladder, why should patients be NPO (nothing by mouth) for at least 4 hours prior to the examination?
For ultrasound imaging of the gallbladder, why should patients be NPO (nothing by mouth) for at least 4 hours prior to the examination?
Which of the following organs can be readily visualized using abdominal ultrasound?
Which of the following organs can be readily visualized using abdominal ultrasound?
Limitations of ultrasound include:
Limitations of ultrasound include:
A patient presents with dysphagia, unexplained weight loss and intractable cough, which diagnostic test is most appropriate?
A patient presents with dysphagia, unexplained weight loss and intractable cough, which diagnostic test is most appropriate?
Which of the following is NOT and indication for Esophagogastroduodenoscopy (EGD):
Which of the following is NOT and indication for Esophagogastroduodenoscopy (EGD):
A patient has a known history of severe thrombocytopenia. Which of the following procedures would be relatively contraindicated?
A patient has a known history of severe thrombocytopenia. Which of the following procedures would be relatively contraindicated?
A patient has suspected aspiration which may cause dysphagia, select the most appropriate test:
A patient has suspected aspiration which may cause dysphagia, select the most appropriate test:
What is the primary goal of esophageal pH monitoring?
What is the primary goal of esophageal pH monitoring?
Which of the following is a functional issue that gastric emptying study can identify?
Which of the following is a functional issue that gastric emptying study can identify?
For which of the listed conditions is a urea breath test primarily used?
For which of the listed conditions is a urea breath test primarily used?
What is a common indication when ordering lower GI testing?
What is a common indication when ordering lower GI testing?
Choose the structural issue a lower GI differential can diagnose:
Choose the structural issue a lower GI differential can diagnose:
What is the primary advantage of video capsule endoscopy (VCE) over traditional endoscopy?
What is the primary advantage of video capsule endoscopy (VCE) over traditional endoscopy?
Following the detection of a low suspicion serologic test, what action is required?
Following the detection of a low suspicion serologic test, what action is required?
Which finding indicates a positive Fecal occult blood test (FOBT):
Which finding indicates a positive Fecal occult blood test (FOBT):
What is the primary purpose of tumor markers in gastrointestinal cancers?
What is the primary purpose of tumor markers in gastrointestinal cancers?
A patient presents with symptoms suggestive of traveler's diarrhea. Which type of bacteria is the most likely cause?
A patient presents with symptoms suggestive of traveler's diarrhea. Which type of bacteria is the most likely cause?
Which parasite is most common in the US?
Which parasite is most common in the US?
Which describes the laboratory test known as.
Which describes the laboratory test known as.
When assessing liver size with abdominal US:
When assessing liver size with abdominal US:
Functional liver issues include:
Functional liver issues include:
Choose a cause of high liver albumin:
Choose a cause of high liver albumin:
Which test can determine is a patient with hepatic failure has any additional variceal hemorrage:
Which test can determine is a patient with hepatic failure has any additional variceal hemorrage:
How is hepatitis A transfered:
How is hepatitis A transfered:
For the labs listed which is not part of the Viral hepatitis lab panels
For the labs listed which is not part of the Viral hepatitis lab panels
Flashcards
What makes up the Upper GI?
What makes up the Upper GI?
Mouth, salivary glands, pharynx, esophagus, stomach & small intestine-duodenum (proximal to ligament of Treitz)
What makes up the Lower GI?
What makes up the Lower GI?
Small intestine-jejunum & ileum (distal to ligament of Treitz) & Large intestine
What are the accessory organs of the GI tract?
What are the accessory organs of the GI tract?
Liver, gallbladder & pancreas
If a patient can stand, what views should be conducted during an Acute Abdominal Series?
If a patient can stand, what views should be conducted during an Acute Abdominal Series?
Signup and view all the flashcards
If a patient is unable to stand, what views should be conducted during an Acute Abdominal Series?
If a patient is unable to stand, what views should be conducted during an Acute Abdominal Series?
Signup and view all the flashcards
If a patient is unable to stand or turn, what views should be conducted during an Acute Abdominal Series?
If a patient is unable to stand or turn, what views should be conducted during an Acute Abdominal Series?
Signup and view all the flashcards
What are we often looking for during a KUB X-ray?
What are we often looking for during a KUB X-ray?
Signup and view all the flashcards
What are we specifically looking for during an Acute Abdominal Series?
What are we specifically looking for during an Acute Abdominal Series?
Signup and view all the flashcards
What are we assessing for during a KUB?
What are we assessing for during a KUB?
Signup and view all the flashcards
When should doctors be concerned and consider an upper GI series?
When should doctors be concerned and consider an upper GI series?
Signup and view all the flashcards
What does an upper GI series with small bowel follow-through help evaluate?
What does an upper GI series with small bowel follow-through help evaluate?
Signup and view all the flashcards
What are the indications for a lower GI series?
What are the indications for a lower GI series?
Signup and view all the flashcards
What are we looking for during ABDO X-rays?
What are we looking for during ABDO X-rays?
Signup and view all the flashcards
What are some characteristics of a normal small bowel during X-ray?
What are some characteristics of a normal small bowel during X-ray?
Signup and view all the flashcards
What are some characteristics of a normal large bowel during X-ray?
What are some characteristics of a normal large bowel during X-ray?
Signup and view all the flashcards
What is the rule of 3-6-9?
What is the rule of 3-6-9?
Signup and view all the flashcards
Indication for CT Scan
Indication for CT Scan
Signup and view all the flashcards
What are the concerns when performing a CT scan?
What are the concerns when performing a CT scan?
Signup and view all the flashcards
When is an ultrasound indicated?
When is an ultrasound indicated?
Signup and view all the flashcards
When is Upper GI diagnostics indicated?
When is Upper GI diagnostics indicated?
Signup and view all the flashcards
What structural issues can Upper GI diagnostics assess?
What structural issues can Upper GI diagnostics assess?
Signup and view all the flashcards
What functional issues can Upper GI diagnostics assess?
What functional issues can Upper GI diagnostics assess?
Signup and view all the flashcards
When is Esophagus diagnostics indicated?
When is Esophagus diagnostics indicated?
Signup and view all the flashcards
What is Upper GI?
What is Upper GI?
Signup and view all the flashcards
What does CT for X-rays look for?
What does CT for X-rays look for?
Signup and view all the flashcards
When do we perform Esophagogastroduodenoscopy (EGD)?
When do we perform Esophagogastroduodenoscopy (EGD)?
Signup and view all the flashcards
What are the contraindications of doing Esophagogastroduodenoscopy (EGD)?
What are the contraindications of doing Esophagogastroduodenoscopy (EGD)?
Signup and view all the flashcards
When do we use Gastric emptying study for functional issues?
When do we use Gastric emptying study for functional issues?
Signup and view all the flashcards
What is the process involved in a Manometry to check function?
What is the process involved in a Manometry to check function?
Signup and view all the flashcards
What is Gastrin labs used for?
What is Gastrin labs used for?
Signup and view all the flashcards
When is lower GI testing indicated?
When is lower GI testing indicated?
Signup and view all the flashcards
If there is indication of Lower GI testing, what are the differential diagnoses?
If there is indication of Lower GI testing, what are the differential diagnoses?
Signup and view all the flashcards
What specific infections must be tested for in Lower-GI/Small Intestine?
What specific infections must be tested for in Lower-GI/Small Intestine?
Signup and view all the flashcards
When imaging in small intestine, what is worth remembering?
When imaging in small intestine, what is worth remembering?
Signup and view all the flashcards
What studies must be lab tested for in order to determine lower GI issues?
What studies must be lab tested for in order to determine lower GI issues?
Signup and view all the flashcards
When doing CT enterography for Lower-GI, what are the main things to consider?
When doing CT enterography for Lower-GI, what are the main things to consider?
Signup and view all the flashcards
When doing Video capsule endoscopy (VCE) for Lower-GI, what are unique things to consider?
When doing Video capsule endoscopy (VCE) for Lower-GI, what are unique things to consider?
Signup and view all the flashcards
What screening test is for colorectal?
What screening test is for colorectal?
Signup and view all the flashcards
What are two types of Salmonella and its common name?
What are two types of Salmonella and its common name?
Signup and view all the flashcards
What are lab markers for Cholangitis?
What are lab markers for Cholangitis?
Signup and view all the flashcards
Study Notes
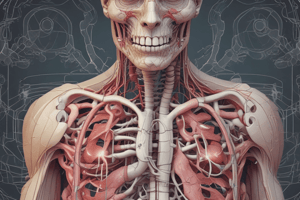
- Explores the anatomy, imaging techniques, and diagnostic procedures related to the gastrointestinal (GI) tract and accessory organs like the liver, gallbladder, and pancreas.
GI Tract Anatomy
- Upper GI includes the mouth, salivary glands, pharynx, esophagus, stomach, and small intestine-duodenum, proximal to the ligament of Treitz.
- Lower GI consists of the small intestine-jejunum & ileum (distal to the ligament of Treitz) and large intestine.
- Accessory organs are the liver, gallbladder, and pancreas.
X-Rays in GI Tract Imaging
- Plain films without contrast are a type of X-ray used.
- Acute abdominal series involves 2-3 views, including AP supine, PA upright, and PA chest if the patient can stand
- If the patient cannot stand, AP supine, left lateral decubitus, and AP spine chest views are taken.
- If the patient cannot stand or turn, AP supine, AP supine chest, and cross-table view (lateral) are used.
- KUB (kidneys, ureters, and bladder) X-rays do not necessarily show the diaphragm
- They are useful for looking for stones or issues in the kidneys, ureters, or bladder.
- Plain films with contrast include upper GI series and upper GI series with small bowel follow-through.
- Contrast X-rays include lower GI series (barium enema +/- air).
Acute Abdominal Series
- Assesses the entire GI tract, specifically looking for gas patterns and areas of potential obstruction.
- Technique depends on the patient's ability to stand or turn.
- If patient can stand, use AP supine, PA upright, and PA chest views
- If patient is unable to stand, use AP supine, left lateral decubitus, AP supine chest views
- If patient is unable to stand and unable to turn, use AP supine, AP supine chest, cross table view (lateral)
Kidneys, Ureters, and Bladder (KUB) Imaging
- Assesses the urogenital tract and specifically looks for calcifications.
- The technique used is the AP supine view.
Upper GI Series
- Indications include mechanical esophageal stricture concern, upper abdominal pain that may be gastric or duodenal, and surgical or duodenal procedure.
- Barium contrast is typically used
- Water-soluble contrast can be used if there is a concern for perforation
- The location of the area of concern dictates the images taken.
Upper GI Series with Small Bowel Follow-Through
- Used for further evaluation of strictures, obstruction, masses, and abnormal motility.
- Limitations include mild strictures and small masses.
- Can be obtained with or without an upper GI series.
- Images are taken every 15-30 minutes until the contrast reaches the terminal ileum.
- The process usually takes 30-120 minutes.
Lower GI Series
- Used to look for colonic strictures (position and length), colonic fistulas, and postoperative leaks after surgery.
- A rectal tube or barium enema is inserted, and contrast is given.
- Multiple images are taken to view all areas of the large intestine from the ileocecal valve to the rectum.
Interpretation of Abdominal X-rays
- Includes identity (patient identifiers like name and date of birth, and study identifiers like date of study) and quality (visibility of lateral edges and vertebrae, centered spinous processes, visualization from diaphragms to pubic symphysis).
- ABDO X components: A (air - intra and extraluminal), B (bowel - position and structure), D (dense stuff - bones and calcification), O (organs and soft tissues), E (external structures/artifacts).
Air Assessment in Abdominal X-Rays
- Intraluminal air is normally found in the stomach, small intestine, and large intestine, with a diffuse, irregular pattern.
- Abnormal intraluminal air presents as distended bowels and air-fluid levels.
- Extraluminal air is rarely normal, except shortly after abdominal surgery when air is used to inflate the abdomen or is introduced during open surgery.
Bowel Assessment
- Normal small bowel is located centrally within the abdomen, with folds running across the lumen's diameter and small air volume.
- Normal large bowel is located peripherally, with folds running part way across the lumen's diameter (haustral folds) and some air or fecal matter.
- Rule of 3-6-9: normal diameters are 3 cm for the small bowel, 6 cm for the large bowel, and 9 cm for the cecum.
Dense Structures, Organs, and Soft Tissues
- Bones assessed include ribs, vertebrae, pelvis, and femur.
- Calcifications may include stones, phleboliths, and vascular structures.
- Organs and soft tissues assessed include the liver, spleen, stomach, kidneys, and psoas muscles.
External Structures/Artifacts on X-rays
- Examples include bladder and NG tubes.
CT Scans of the GI Tract
- Indications include abdominal pain, ascites, jaundice, abnormal liver tests, and renal symptoms.
- Patients must be able to lie flat and still.
- Contrast protocol may be required, depending on the test ordered.
- Rendering options: abdomen only, pelvis only, or abdomen and pelvis.
- Contrast options: without, with oral only, or with IV only.
- Concerns include pregnancy (negative test required for females of childbearing age) and renal function (required if receiving IV iodinated contrast).
Ultrasound of the GI Tract
- Indications include abdominal pain, ascites, jaundice, abnormal liver tests, renal symptoms, and pregnancy.
- RUQ or complete ultrasounds require patients with a gallbladder to be NPO for 4 hours prior.
- Renal/bladder or pelvic ultrasounds need a full bladder.
- Visualization includes organs (liver, gallbladder, pancreas, kidneys/bladder, uterus/ovaries) and vasculature (aorta, renal arteries).
- Studies should be specific : complete abdominal, RUQ, renal, or renal artery US.
- Limitations include difficulty getting clear pictures in large patients and the need for additional studies.
- A good initial test is for patients when other studies may be contraindicated.
Upper GI Diagnostics
- Indications include nausea, vomiting, hematemesis, melena, anemia, non-cardiac chest pain, dysphagia, unexplained weight loss, and intractable cough.
- Assessment can include structural issues (ulcers, inflammation, varices, strictures, lesions/masses, abscesses, tears/ruptures) and functional issues (impaired motility, secretion, absorption).
- Diagnostic tools include X-rays (upper GI series), CT chest, EGD, modified barium swallow, FEES study, manometry, and pH monitoring.
- CT is seen the best on CT chest
Esophagus Diagnostics
- Indications include dysphagia, globus sensation, non-cardiac chest pain, and hematemesis/melena.
- Assessment includes structural issues.
X-Rays for Diagnosis
- Types include barium swallow (with fluoroscopy) and upper GI series (plain films at different time intervals, used to look for strictures, masses, and dilatation).
Esophagogastroduodenoscopy (EGD)
- An endoscope is inserted into the upper GI tract for direct visualization.
- Indications: Diagnostic for chronic upper abdominal pain, dysphagia, and iron deficiency anemia; Therapeutic for foreign body removal, dilation or stenting of strictures, esophageal variceal ligation, upper GI bleeding control, placement of feeding tubes, and management of achalasia.
- Contraindications: Absolute (perforated bowel, peritonitis, toxic megacolon); Relative (coagulation issues, increased risk of perforation, unstable patient).
- Complications: Sedation related (hypoxemia, hypotension, arrhythmias, aspiration) and Procedural (bleeding, infection, perforation).
Endoscopic Ultrasound (EUS)
- Ultrasound attachment on end of endoscope
- It can evaluate masses/lesions within the wall of the esophagus can assess other organs surrounding tissues.
Modified Barium Swallow (MBS)
- Fluoroscopy assesses swallow/peristalsis with barium liquids/solids.
- Indications: Dysphagia and suspected aspiration; Contraindications: Perforation and GI obstruction; Complications: N/V, hypersensitivity, and constipation/diarrhea.
Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
- Fiberoptic scope in the nares allows evaluation of swallowing.
- Indications: Dysphagia, suspected aspiration, and patients who can't have MBS (pregnant or unable to travel to radiology).
- Contraindications: Inability to tolerate barium, severe agitation/movement disorder, severe bleeding disorders, recent epistaxis/nasal surgery, and bilateral obstruction of nasal passages.
- Complications: Vomiting, epistaxis, mucosal perforation, and laryngospasm.
Manometry
- A probe is inserted through the nares into the esophagus that has pressure sensors.
- Indications: Dysphagia, odynophagia, GERD, and non-cardiac chest pain.
- Contraindications/cautions: Recent esophageal/nasal trauma/surgery, significant epistaxis history, esophageal varices, and coagulation issues.
- Complications: Vomiting, epistaxis, and perforation.
Esophageal pH Monitoring
- A probe is inserted through the nares into the esophagus that contains pH sensors.
- Indications: GERD and non-cardiac chest pain.
- Contraindications/cautions: Recent esophageal/nasal trauma or surgery, significant epistaxis history, esophageal varices, and coagulation issues.
- Complications: Vomiting, epistaxis, and perforation.
Stomach Diagnostics
- Indications: Chronic N/V, hematemesis, melena, GERD, upper abdominal pain (typically epigastric/LUQ), non-cardiac chest pain, and abdominal bloating/distention.
- Assessment includes structural issues (X-ray, CT abdomen, EGD) and functional issues (gastric emptying study, manometry, pH monitoring).
- Labs: H. pylori and pathology.
- CT difficult to asses in stomach
Esophagogastroduodenoscopy (EGD) for Stomach Diagnostics
- Indications: Diagnostic for chronic upper abdominal pain and iron deficiency anemia.
Gastric Emptying Study
- NM study where radionucleotide tracer mixed with food
- It is conducted with images at set intervals.
- Functional: Suspected gastroparesis(early satiety, post-prandial N/V or abdominal pain) and GERD. .
- Cautions include allergy and Hyperglycemia in diabetes
- Complications include Allergic reaction to tracer and discomfort/nausea associate
Esophageal Manometry
- Functional procedure, a probe places through the nares and endoscopy to the duodenum
- Measurements taken at rest and small mea
- Indications: Gastric motility disorders, cardiac chest pian and GERD
- Cautions: Recent esophageal and nasal trauma
- Complications: Perforation
Lab Studies for gastric problems
- H. pylori: tests for a gram-rod bacteria, often acquired in childhood and colonizes gastric epithelium
- Non-invasive tests for H. Pylori: Urea breath test, stool test and serologic tests (most common)
- Invasive test for H. Pylori: CLO test and PCR test/culture
Duodenum Diagnostics
- Indications: Chronic N/V, hematemesis, melena, GERD, upper abdominal pain, non-cardiac chest pain, and abdominal bloating/distention.
- Assessment includes structural issues (X-ray, CT abdomen, EGD).
Lower GI Testing
- Indications: N/V, hematemesis, melena (with negative EGD), abdominal pain, weight loss, abdominal distention, diarrhea, flatulence, and abnormal imaging.
- Differential diagnosis includes structural issues (strictures, volvulus, intussusception, fistulas, masses, diverticular disease, inflammatory bowel disease, ulcers/lesions, hemorrhoids) and functional issues (malabsorption/maldigestion like Celiac disease, changes in motility like ileus) and infectious issues (Appendicitis, Bacteria, Colitis)
Small Intestine Disorders
- Celiac Disease, Obstruction, GI Bleed, Hernia
- Obstructions inclue Adhesions, Mass and interssussception
- GI bleed. and Ischemic Bowel are also factors
Small Interitis Diagnostics
- Imaging used when diagnostics
Small Bowel Follow Through
- Radiography and use of contrast to visualize the small bowel function
Lower GI Testing: Imaging
- CT, CT enterogrpahy
- Video capsule endoscopy (VCE)
- Lab studies: Malabsorption , fecalat and celiac Labs
Tests
- Modified CT
- CTA contrast
- Video Capsule of small intestine.
Malabsportion Tests
- Fat based tests, fecal fat test
- Not widely avaliable: hydrogeren breath test.
Large Intestine Diagonsics
- Disorders abscess/filstula, constipation and Diverticular disease. Inflammatory Bowel disease and obstruction along with polyps
- Toxic Megacolon
- Plain film, obstruction visualiation.
Tagged RBC Scan
- Colonoscopy and Sigmoidscope
Fecal Occult Blood Test
- Caused by Refluc esophagitis. Reflux Esophagitis or petic ulcer
Pathogen Testing
- Stool and parasites
- Microscopic test of ova in test
Diarrhea Types
- Enterhemorhagin (EHEC)
- Salmonella (never norma)
- Salmoneela enterica"Thyroid"
- Clostriodidies
Diagnostics Evaluation
- GDH Test antigen, Reflex testing and c Diff toxin Assay
Laboratories of Intestines
- antigen in tools
- Protozao of parasite of intestinal amobe
Small Bowel Test
- Nematodes roundworm, hookworm and pinworn,
Colon cancer test
- Stool test, colonoscope and sigmoniscope
Accessory Organ Functions
Gallbladder and pancreas is tested with nauesses, Vomit and Abdominal pain . Structural stones in this area. Tests: Ultrasound and cat scan will run blood and enzyme
Liver Diagnostics
- Structural problems (Masses for example) using Ultrasound
- CT and MRI Used to assesses level of fibroids and changes
Liver labs
- Albumin
- Transaminisess Transanimase: Enzyme that create insulin, the liver and kidney and muscle all help Albumin help control function
Billrubin tests
- Blood urine and Stool
- Urobilin
- Jaundice : BUILPUP of bilirubin in the blood
- Prehepatic Hepatocellalur and post herpatic
Alpha Fetoprotein
- Hepato cellular,
Hepatits Labs
Fecal Oral: A Vaccine vailable HbsG and Hcs AB. Viral hepatitis Labs of Acute. .
pancreatic cancer C19 and assesment response with treamtent
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.