Podcast
Questions and Answers
What is the primary role of mucous glands found throughout the alimentary canal?
What is the primary role of mucous glands found throughout the alimentary canal?
- Producing hormones that regulate appetite.
- Providing lubrication and protection via mucus secretion. (correct)
- Synthesizing bile for fat emulsification.
- Secreting digestive enzymes for protein breakdown.
How does sympathetic stimulation impact alimentary tract glandular secretion when parasympathetic or hormonal stimulation is already inducing copious secretion?
How does sympathetic stimulation impact alimentary tract glandular secretion when parasympathetic or hormonal stimulation is already inducing copious secretion?
- It has no effect on secretion.
- It selectively increases secretion of mucous cells only.
- It reduces secretion due to vasoconstrictive reduction of blood supply. (correct)
- It further increases secretion due to enhanced glandular cell activity.
What is the underlying mechanism by which gastrointestinal hormones stimulate secretion in the stomach and intestine?
What is the underlying mechanism by which gastrointestinal hormones stimulate secretion in the stomach and intestine?
- Increasing the pH of the intestinal lumen.
- Being transported via the bloodstream to glands after being released from the gastrointestinal mucosa. (correct)
- Directly activating enzyme-producing cells.
- Inhibiting the enteric nervous system.
What key event is triggered by nervous or hormonal control signals to facilitate the extrusion of vesicular contents from glandular cells?
What key event is triggered by nervous or hormonal control signals to facilitate the extrusion of vesicular contents from glandular cells?
Under resting conditions, what ionic characteristic distinguishes saliva from plasma?
Under resting conditions, what ionic characteristic distinguishes saliva from plasma?
How does saliva contribute to oral hygiene by counteracting the deteriorative processes caused by pathogenic bacteria?
How does saliva contribute to oral hygiene by counteracting the deteriorative processes caused by pathogenic bacteria?
Which of the following stimuli would MOST LIKELY result in copious salivation?
Which of the following stimuli would MOST LIKELY result in copious salivation?
What is the physiological rationale behind the vasodilation induced by kallikrein in the salivary glands during salivation?
What is the physiological rationale behind the vasodilation induced by kallikrein in the salivary glands during salivation?
What component of gastric juice is secreted by the parietal cells?
What component of gastric juice is secreted by the parietal cells?
What is the functional significance of the alkaline mucus secreted by surface mucous cells in the stomach?
What is the functional significance of the alkaline mucus secreted by surface mucous cells in the stomach?
How does histamine secretion by ECL cells affect acid secretion in the stomach, and how is this process regulated?
How does histamine secretion by ECL cells affect acid secretion in the stomach, and how is this process regulated?
A patient has lost the ability to secrete normal amounts of acid in the stomach. How would this primarily impact pepsinogen secretion, and why?
A patient has lost the ability to secrete normal amounts of acid in the stomach. How would this primarily impact pepsinogen secretion, and why?
What is the specific role of secretin in the context of intestinal factors inhibiting gastric secretion?
What is the specific role of secretin in the context of intestinal factors inhibiting gastric secretion?
How does the secretion during the 'interdigestive period' differ in composition from that which occurs at the onset of a meal, and which stimuli can alter this?
How does the secretion during the 'interdigestive period' differ in composition from that which occurs at the onset of a meal, and which stimuli can alter this?
What is the role of bicarbonate ions ($HCO_3^−$) in pancreatic secretion, and how is it regulated in response to the acidic chyme entering the duodenum?
What is the role of bicarbonate ions ($HCO_3^−$) in pancreatic secretion, and how is it regulated in response to the acidic chyme entering the duodenum?
Which mechanism prevents the activation of proteolytic enzymes within the pancreas itself, and what condition can result if this mechanism fails?
Which mechanism prevents the activation of proteolytic enzymes within the pancreas itself, and what condition can result if this mechanism fails?
Why is stimulation of the sympathetic nerves going to the gastrointestinal tract considered to have 'dual effect' on alimentary tract glandular secretion rates?
Why is stimulation of the sympathetic nerves going to the gastrointestinal tract considered to have 'dual effect' on alimentary tract glandular secretion rates?
How do acetylcholine and cholecystokinin (CCK) synergistically regulate pancreatic secretion?
How do acetylcholine and cholecystokinin (CCK) synergistically regulate pancreatic secretion?
What is the effect of secretin on bile secretion?
What is the effect of secretin on bile secretion?
How do bile salts facilitate the absorption of digested fats in the small intestine, and what results from deficiency?
How do bile salts facilitate the absorption of digested fats in the small intestine, and what results from deficiency?
What mechanism primarily stimulates the release of bile from the gallbladder into the duodenum during digestion?
What mechanism primarily stimulates the release of bile from the gallbladder into the duodenum during digestion?
How does sympathetic stimulation influence the protective function of Brunner's glands in the duodenum?
How does sympathetic stimulation influence the protective function of Brunner's glands in the duodenum?
What are the two primary cell types found in the epithelium covering the crypts and villi of the small intestine, and what are their respective functions?
What are the two primary cell types found in the epithelium covering the crypts and villi of the small intestine, and what are their respective functions?
What is the proposed mechanism responsible for mucus secretion with moderate amounts of $HCO_3^-$ in the large intestine?
What is the proposed mechanism responsible for mucus secretion with moderate amounts of $HCO_3^-$ in the large intestine?
When excessive mucus secretion occurs in the large intestine due to extremes in parasympathetic stimulation, what is the typical composition of the resulting bowel movement?
When excessive mucus secretion occurs in the large intestine due to extremes in parasympathetic stimulation, what is the typical composition of the resulting bowel movement?
What is the net reaction in the duodenum when gastric acid ($HCl$) is neutralized by pancreatic bicarbonate ($NaHCO_3$), and how does this process aid in preventing duodenal ulcers?
What is the net reaction in the duodenum when gastric acid ($HCl$) is neutralized by pancreatic bicarbonate ($NaHCO_3$), and how does this process aid in preventing duodenal ulcers?
How does the secretion of intestinal digestive juices (via the crypts of Lieberkühn) differ between the crypts and the villi, and what is the overall effect?
How does the secretion of intestinal digestive juices (via the crypts of Lieberkühn) differ between the crypts and the villi, and what is the overall effect?
A surgeon removes the distal 20% of a patient's stomach. Which of the following is a direct, immediate consequence?
A surgeon removes the distal 20% of a patient's stomach. Which of the following is a direct, immediate consequence?
Which of these statements best captures why a patient with chronic gastritis might develop pernicious anemia?
Which of these statements best captures why a patient with chronic gastritis might develop pernicious anemia?
Which of the following statements captures intestinal secretions in the duodenum?
Which of the following statements captures intestinal secretions in the duodenum?
What is the primary mechanism by which the alimentary tract glands, specifically mucous cells, are stimulated to secrete mucus?
What is the primary mechanism by which the alimentary tract glands, specifically mucous cells, are stimulated to secrete mucus?
In the context of gastrointestinal secretion, which of the following best defines the structural organization of the salivary glands and pancreas?
In the context of gastrointestinal secretion, which of the following best defines the structural organization of the salivary glands and pancreas?
How do the enteric nervous system's responses to activation stimuli (tactile, chemical, distention) MOST DIRECTLY influence digestive processes in the gut wall?
How do the enteric nervous system's responses to activation stimuli (tactile, chemical, distention) MOST DIRECTLY influence digestive processes in the gut wall?
Which of the following represents the MOST COMPLETE description of the dual effect of sympathetic stimulation on alimentary tract glandular secretion?
Which of the following represents the MOST COMPLETE description of the dual effect of sympathetic stimulation on alimentary tract glandular secretion?
What is the physiological significance of gastrointestinal hormones in the digestive process?
What is the physiological significance of gastrointestinal hormones in the digestive process?
What is the primary role of ribosomes adherent to the endoplasmic reticulum in glandular cells?
What is the primary role of ribosomes adherent to the endoplasmic reticulum in glandular cells?
Which of the following best describes the process of exocytosis in glandular cells, leading to the release of vesicular contents?
Which of the following best describes the process of exocytosis in glandular cells, leading to the release of vesicular contents?
How does the secretion of water and electrolytes support glandular function, specifically related to the secretion of organic substances?
How does the secretion of water and electrolytes support glandular function, specifically related to the secretion of organic substances?
What structural and functional characteristics of mucus make it well-suited as a protectant for the gut wall?
What structural and functional characteristics of mucus make it well-suited as a protectant for the gut wall?
Why is saliva considered essential for maintaining oral hygiene, and what are the specific mechanisms involved?
Why is saliva considered essential for maintaining oral hygiene, and what are the specific mechanisms involved?
What specific role do taste stimuli, particularly sour tastes, play in the regulation of salivary secretion, and how does this compare to the effect of tactile stimuli?
What specific role do taste stimuli, particularly sour tastes, play in the regulation of salivary secretion, and how does this compare to the effect of tactile stimuli?
In the stomach, how do mucous neck cells, peptic cells, and parietal cells each contribute to the gastric secretions, and how does their location within the oxyntic glands influence their function?
In the stomach, how do mucous neck cells, peptic cells, and parietal cells each contribute to the gastric secretions, and how does their location within the oxyntic glands influence their function?
What is the role of enterochromaffin-like (ECL) cells in the gastric glands, and how do gastrin and histamine interact to regulate hydrochloric acid secretion?
What is the role of enterochromaffin-like (ECL) cells in the gastric glands, and how do gastrin and histamine interact to regulate hydrochloric acid secretion?
How does the production of $HCO_3^-$ in parietal cells directly contribute to gastric venous blood having a higher pH than arterial blood when the stomach is secreting acid?
How does the production of $HCO_3^-$ in parietal cells directly contribute to gastric venous blood having a higher pH than arterial blood when the stomach is secreting acid?
If the gastric barrier is damaged, what is the immediate consequence, and what substances commonly cause such damage?
If the gastric barrier is damaged, what is the immediate consequence, and what substances commonly cause such damage?
What role does secretin play in the 'intestinal phase' of gastric secretion, and what other hormonal and neural factors contribute to this phase?
What role does secretin play in the 'intestinal phase' of gastric secretion, and what other hormonal and neural factors contribute to this phase?
How does gastric secretion change during the 'interdigestive period' compared to during active digestion, and how can interdigestive secretion be altered?
How does gastric secretion change during the 'interdigestive period' compared to during active digestion, and how can interdigestive secretion be altered?
Why is activation of trypsinogen limited to only after it is secreted into the intestinal tract, and what protective mechanisms are in place to prevent premature activation within the pancreas?
Why is activation of trypsinogen limited to only after it is secreted into the intestinal tract, and what protective mechanisms are in place to prevent premature activation within the pancreas?
Describe the specific cellular mechanism by which bicarbonate ions are secreted into the pancreatic ductules and ducts.
Describe the specific cellular mechanism by which bicarbonate ions are secreted into the pancreatic ductules and ducts.
What are the principal digestive outcomes that arise from the combined actions of trypsin, chymotrypsin, and carboxypolypeptidase, and how do they compare to the action of pancreatic amylase?
What are the principal digestive outcomes that arise from the combined actions of trypsin, chymotrypsin, and carboxypolypeptidase, and how do they compare to the action of pancreatic amylase?
How do acetylcholine and cholecystokinin (CCK) independently and cooperatively affect pancreatic secretion, and how does this differ from the action of secretin?
How do acetylcholine and cholecystokinin (CCK) independently and cooperatively affect pancreatic secretion, and how does this differ from the action of secretin?
What mechanisms regulate bile secretion and flow, and how do they coordinate with fat digestion in the duodenum?
What mechanisms regulate bile secretion and flow, and how do they coordinate with fat digestion in the duodenum?
Which process facilitates the emulsification of large fat particles for effective action by lipase enzymes, and what are the primary components of bile responsible for this process?
Which process facilitates the emulsification of large fat particles for effective action by lipase enzymes, and what are the primary components of bile responsible for this process?
What is the function of micelles in the context of fat digestion and absorption, and what results from a deficit in the micelle formation?
What is the function of micelles in the context of fat digestion and absorption, and what results from a deficit in the micelle formation?
How are bile salts recirculated in the enterohepatic circulation, and why is this recirculation important for overall bile secretion?
How are bile salts recirculated in the enterohepatic circulation, and why is this recirculation important for overall bile secretion?
How does secretion contribute to the two main functions of Bile?
How does secretion contribute to the two main functions of Bile?
Describe the effect that secretion has on the duodenal wall's protective measures from the effects of highly acidic gastric juices emptying from the stomach.
Describe the effect that secretion has on the duodenal wall's protective measures from the effects of highly acidic gastric juices emptying from the stomach.
A surgeon removes the gastrin-secreting portion of the stomach. Which of the following is a direct, immediate consequence?
A surgeon removes the gastrin-secreting portion of the stomach. Which of the following is a direct, immediate consequence?
What is the precise order that the water and electrolytes are moved between compartments during secretion of isosmotic sodium bicarbonate solution by the pancreatic ductules?
What is the precise order that the water and electrolytes are moved between compartments during secretion of isosmotic sodium bicarbonate solution by the pancreatic ductules?
Which of the following statements best captures how the stomach is able to absorb alcohol?
Which of the following statements best captures how the stomach is able to absorb alcohol?
What is the name and function of the 'pits' that are parts of the small intestine, located on the surfaces?
What is the name and function of the 'pits' that are parts of the small intestine, located on the surfaces?
In the small intestine, water is drawn into what region due to high concentration of electrolytes, which allows flow to the villi?
In the small intestine, water is drawn into what region due to high concentration of electrolytes, which allows flow to the villi?
What are the roles from a regulatory and functional state of secretion in the Small Intestine?
What are the roles from a regulatory and functional state of secretion in the Small Intestine?
What is removed from the bile as it concentrates in the gallbladder?
What is removed from the bile as it concentrates in the gallbladder?
How exactly is secretion performed to lubricate feces, and regulate the bowel from acids, in the Large Intestine?
How exactly is secretion performed to lubricate feces, and regulate the bowel from acids, in the Large Intestine?
Secretion can influence the bowel, in what ways?
Secretion can influence the bowel, in what ways?
Why are pancreatic secretions activated only after entering the intestinal tract?
Why are pancreatic secretions activated only after entering the intestinal tract?
What part does secretin provide to the intestinal secretion rates when acid chyme enters from the stomach?
What part does secretin provide to the intestinal secretion rates when acid chyme enters from the stomach?
Which selection provides the correct amount of juices secreted daily in a human alimentary system and their mean?
Which selection provides the correct amount of juices secreted daily in a human alimentary system and their mean?
What key property enables mucus to protect the gut wall from chemical damage, in addition to its role as a lubricant?
What key property enables mucus to protect the gut wall from chemical damage, in addition to its role as a lubricant?
If the duct cells of the salivary glands were damaged, compromising their ability to reabsorb sodium ions, what effect would this have on saliva composition during maximal salivation?
If the duct cells of the salivary glands were damaged, compromising their ability to reabsorb sodium ions, what effect would this have on saliva composition during maximal salivation?
How does the enteric nervous system respond to distension of the gut wall to mediate an increase in secretion?
How does the enteric nervous system respond to distension of the gut wall to mediate an increase in secretion?
How does the production of bicarbonate ($HCO_3^−$) in parietal cells relate to the acidity levels of venous blood leaving the stomach during hydrochloric acid secretion?
How does the production of bicarbonate ($HCO_3^−$) in parietal cells relate to the acidity levels of venous blood leaving the stomach during hydrochloric acid secretion?
Which sequence accurately reflects the steps in hydrochloric acid production by parietal cells?
Which sequence accurately reflects the steps in hydrochloric acid production by parietal cells?
In situations where the gastric barrier is compromised due to excessive alcohol consumption, what immediate physiological response is likely to occur?
In situations where the gastric barrier is compromised due to excessive alcohol consumption, what immediate physiological response is likely to occur?
Upon entry of chyme into the small intestine, what integrated responses are initiated to modulate gastric secretion?
Upon entry of chyme into the small intestine, what integrated responses are initiated to modulate gastric secretion?
What mechanism prevents pancreatic self-digestion by proteolytic enzymes before they reach the intestinal tract?
What mechanism prevents pancreatic self-digestion by proteolytic enzymes before they reach the intestinal tract?
How does the activation of trypsinogen contribute to the overall digestion process once it enters the intestinal lumen?
How does the activation of trypsinogen contribute to the overall digestion process once it enters the intestinal lumen?
If the pancreas is stimulated to secrete copiously, resulting in a bicarbonate concentration of 145 mEq/L in the pancreatic juice, how does this high concentration facilitate duodenal neutralization of gastric acid?
If the pancreas is stimulated to secrete copiously, resulting in a bicarbonate concentration of 145 mEq/L in the pancreatic juice, how does this high concentration facilitate duodenal neutralization of gastric acid?
What mechanisms are involved in the secretion of isosmotic sodium bicarbonate solution by pancreatic ductules, ensuring fluid balance?
What mechanisms are involved in the secretion of isosmotic sodium bicarbonate solution by pancreatic ductules, ensuring fluid balance?
How do secretin and cholecystokinin (CCK) interact at the pancreas to regulate overall digestive function?
How do secretin and cholecystokinin (CCK) interact at the pancreas to regulate overall digestive function?
How does the disruption of enterohepatic circulation of bile salts impact overall fat absorption, and why?
How does the disruption of enterohepatic circulation of bile salts impact overall fat absorption, and why?
What mechanisms ensure the gallbladder efficiently empties its contents into the duodenum when stimulated by cholecystokinin (CCK)?
What mechanisms ensure the gallbladder efficiently empties its contents into the duodenum when stimulated by cholecystokinin (CCK)?
Under which conditions would cholesterol be MOST LIKELY to precipitate out of the bile and form gallstones?
Under which conditions would cholesterol be MOST LIKELY to precipitate out of the bile and form gallstones?
In a patient with chronically reduced gastric secretion, what intestinal adaptation is MOST LIKELY to occur and how does it affect overall digestive processes?
In a patient with chronically reduced gastric secretion, what intestinal adaptation is MOST LIKELY to occur and how does it affect overall digestive processes?
What is the coordinated function of the crypts of Lieberkühn and villi in the small intestine to maximize nutrient absorption?
What is the coordinated function of the crypts of Lieberkühn and villi in the small intestine to maximize nutrient absorption?
If the large intestine experiences extreme parasympathetic stimulation due to emotional disturbances, what changes in secretion and bowel movement are MOST likely?
If the large intestine experiences extreme parasympathetic stimulation due to emotional disturbances, what changes in secretion and bowel movement are MOST likely?
What is the critical role of mucus and bicarbonate secretion in the large intestine in protecting the bowel and facilitating waste elimination?
What is the critical role of mucus and bicarbonate secretion in the large intestine in protecting the bowel and facilitating waste elimination?
What feedback mechanisms regulate the liver's production of bile salts based on their availability in the enterohepatic circulation?
What feedback mechanisms regulate the liver's production of bile salts based on their availability in the enterohepatic circulation?
If a patient's duodenum is unable to produce secretin, how would this MOST DIRECTLY impact pancreatic secretions and duodenal environment?
If a patient's duodenum is unable to produce secretin, how would this MOST DIRECTLY impact pancreatic secretions and duodenal environment?
What best explains how the mucous glands in the alimentary canal are different in response to sympathetic vs parasympathetic stimulation?
What best explains how the mucous glands in the alimentary canal are different in response to sympathetic vs parasympathetic stimulation?
Digestive enzymes are only secreted in the stomach and intestines.
Digestive enzymes are only secreted in the stomach and intestines.
Mucous glands, present throughout the alimentary canal, secrete mucus for lubrication and protection.
Mucous glands, present throughout the alimentary canal, secrete mucus for lubrication and protection.
Goblet cells primarily respond to alkaline substances in the alimentary tract.
Goblet cells primarily respond to alkaline substances in the alimentary tract.
Crypts of Lieberkühn are invaginations of the epithelium found mainly in the stomach.
Crypts of Lieberkühn are invaginations of the epithelium found mainly in the stomach.
Salivary glands secrete digestive and emulsification substances for food.
Salivary glands secrete digestive and emulsification substances for food.
The enteric nervous system is activated by tactile stimulation, chemical irritation, and contraction of the gut wall.
The enteric nervous system is activated by tactile stimulation, chemical irritation, and contraction of the gut wall.
Parasympathetic stimulation generally decreases the secretion rate of alimentary tract glands.
Parasympathetic stimulation generally decreases the secretion rate of alimentary tract glands.
Sympathetic stimulation always increases secretion in the alimentary tract glands.
Sympathetic stimulation always increases secretion in the alimentary tract glands.
Gastrointestinal hormones are liberated from the intestinal mucosa in response to the absence of food in the lumen of the gut.
Gastrointestinal hormones are liberated from the intestinal mucosa in response to the absence of food in the lumen of the gut.
The synthesis of organic secretory substances occurs almost entirely in the lysosomes of the glandular cell.
The synthesis of organic secretory substances occurs almost entirely in the lysosomes of the glandular cell.
Saliva contains higher concentrations of sodium and chloride than plasma under normal conditions.
Saliva contains higher concentrations of sodium and chloride than plasma under normal conditions.
Sour taste stimuli typically decrease saliva secretion.
Sour taste stimuli typically decrease saliva secretion.
The compound mucous glands are located near the esophagogastric junction to shield the esophagus from ingested pathogens.
The compound mucous glands are located near the esophagogastric junction to shield the esophagus from ingested pathogens.
Oxyntic glands secrete hydrochloric acid, pepsinogen, intrinsic factor, and mucus.
Oxyntic glands secrete hydrochloric acid, pepsinogen, intrinsic factor, and mucus.
Histamine stimulates acid secretion by peptic cells.
Histamine stimulates acid secretion by peptic cells.
The cephalic phase accounts for about 90% of the gastric secretion associated with eating a meal.
The cephalic phase accounts for about 90% of the gastric secretion associated with eating a meal.
Secretin reduces stomach acidity
Secretin reduces stomach acidity
The pancreas secretes digestive enzymes into the bloodstream for systemic distribution.
The pancreas secretes digestive enzymes into the bloodstream for systemic distribution.
CCK stimulates the pancreas to secrete digestive enzymes.
CCK stimulates the pancreas to secrete digestive enzymes.
The liver secretes digestive enzymes to cause fat digestion.
The liver secretes digestive enzymes to cause fat digestion.
Match each alimentary gland type with its primary means of secretion stimulation:
Match each alimentary gland type with its primary means of secretion stimulation:
Match the phase of gastric secretion with its approximate contribution to the total gastric secretion associated with a meal:
Match the phase of gastric secretion with its approximate contribution to the total gastric secretion associated with a meal:
Match each type of secretory cell in the gastric (oxyntic) glands with its primary secretion:
Match each type of secretory cell in the gastric (oxyntic) glands with its primary secretion:
Associate each substance with its role in hydrochloric acid secretion by parietal cells:
Associate each substance with its role in hydrochloric acid secretion by parietal cells:
Match each pancreatic enzyme with its primary digestive function:
Match each pancreatic enzyme with its primary digestive function:
Match each stimulus with its effect on pancreatic secretion:
Match each stimulus with its effect on pancreatic secretion:
Associate each term with its role in bile secretion and function:
Associate each term with its role in bile secretion and function:
Match the contributing factor that aids saliva for oral hygiene:
Match the contributing factor that aids saliva for oral hygiene:
Match the component of the small intestine secretion's role:
Match the component of the small intestine secretion's role:
Match each type of gastrointestinal hormone:
Match each type of gastrointestinal hormone:
Flashcards
Primary functions of secretory glands in the gastrointestinal tract?
Primary functions of secretory glands in the gastrointestinal tract?
Digestive enzymes are secreted from the mouth to the distal ileum. Mucous glands provide mucus for lubrication and protection throughout the alimentary tract.
What are mucous or goblet cells?
What are mucous or goblet cells?
Single-cell mucous glands that extrude mucus directly onto the epithelial surface, acting as a lubricant and protecting against excoriation and digestion.
What are the crypts of Lieberkühn?
What are the crypts of Lieberkühn?
Invaginations of the epithelium into the submucosa in the small intestine, containing specialized secretory cells.
What are tubular glands?
What are tubular glands?
Signup and view all the flashcards
What are the alimentary tract's complex glands?
What are the alimentary tract's complex glands?
Signup and view all the flashcards
What stimuli activate the enteric nervous system?
What stimuli activate the enteric nervous system?
Signup and view all the flashcards
What does parasympathetic stimulation do?
What does parasympathetic stimulation do?
Signup and view all the flashcards
What is the dual effect of sympathetic stimulation?
What is the dual effect of sympathetic stimulation?
Signup and view all the flashcards
Gastrointestinal hormone function?
Gastrointestinal hormone function?
Signup and view all the flashcards
Basic mechanism of secretion by glandular cells?
Basic mechanism of secretion by glandular cells?
Signup and view all the flashcards
What are the properties of mucus?
What are the properties of mucus?
Signup and view all the flashcards
What is saliva composed of?
What is saliva composed of?
Signup and view all the flashcards
What are primary glands of salivation?
What are primary glands of salivation?
Signup and view all the flashcards
How are ions secreted in saliva?
How are ions secreted in saliva?
Signup and view all the flashcards
What stimulates the salivatory nuclei?
What stimulates the salivatory nuclei?
Signup and view all the flashcards
Nervous regulation of salivary secretion?
Nervous regulation of salivary secretion?
Signup and view all the flashcards
Oral hygiene function of saliva?
Oral hygiene function of saliva?
Signup and view all the flashcards
Esophageal secretions?
Esophageal secretions?
Signup and view all the flashcards
What are the two types of tubular glands in the stomach?
What are the two types of tubular glands in the stomach?
Signup and view all the flashcards
Three main cell types in oxyntic glands?
Three main cell types in oxyntic glands?
Signup and view all the flashcards
Basic mechanism of hydrochloric acid secretion?
Basic mechanism of hydrochloric acid secretion?
Signup and view all the flashcards
What stimulates gastric acid secretion?
What stimulates gastric acid secretion?
Signup and view all the flashcards
Secretions role?
Secretions role?
Signup and view all the flashcards
What happens without intrinsic factor?
What happens without intrinsic factor?
Signup and view all the flashcards
Pyloric glands?
Pyloric glands?
Signup and view all the flashcards
Surface mucous cells?
Surface mucous cells?
Signup and view all the flashcards
enterochromaffin-like cells (ECL cells)
enterochromaffin-like cells (ECL cells)
Signup and view all the flashcards
Is when HCl is secreted?
Is when HCl is secreted?
Signup and view all the flashcards
What does acetylcholine excite?
What does acetylcholine excite?
Signup and view all the flashcards
What are the three phases of gastric secretion?
What are the three phases of gastric secretion?
Signup and view all the flashcards
Neurogenic Signals
Neurogenic Signals
Signup and view all the flashcards
Gastric secretion?
Gastric secretion?
Signup and view all the flashcards
Pancreatic Secretion
Pancreatic Secretion
Signup and view all the flashcards
enzymes for digesting proteins?
enzymes for digesting proteins?
Signup and view all the flashcards
Trypsinogen activated?
Trypsinogen activated?
Signup and view all the flashcards
Trypsin inhibitor?
Trypsin inhibitor?
Signup and view all the flashcards
Secretion Bicarbonate lons
Secretion Bicarbonate lons
Signup and view all the flashcards
3 Basic Stimuli?
3 Basic Stimuli?
Signup and view all the flashcards
Secretin do?
Secretin do?
Signup and view all the flashcards
Local epithelial stimulation
Local epithelial stimulation
Signup and view all the flashcards
Function of saliva for oral hygiene?
Function of saliva for oral hygiene?
Signup and view all the flashcards
What are gastric glands?
What are gastric glands?
Signup and view all the flashcards
What are GI hormones?
What are GI hormones?
Signup and view all the flashcards
What does pepsin do?
What does pepsin do?
Signup and view all the flashcards
Cholecystokinin?
Cholecystokinin?
Signup and view all the flashcards
Bile acids
Bile acids
Signup and view all the flashcards
What are the function of bile salts?
What are the function of bile salts?
Signup and view all the flashcards
What is Duodenum?
What is Duodenum?
Signup and view all the flashcards
What are brunner's glands
What are brunner's glands
Signup and view all the flashcards
mucosa of the large intestine
mucosa of the large intestine
Signup and view all the flashcards
What is exocytosis?
What is exocytosis?
Signup and view all the flashcards
What is the enterogastric reflex?
What is the enterogastric reflex?
Signup and view all the flashcards
Concentrates Bile
Concentrates Bile
Signup and view all the flashcards
What is the gastric barrier
What is the gastric barrier
Signup and view all the flashcards
What is bile?
What is bile?
Signup and view all the flashcards
What does diarrhea do?
What does diarrhea do?
Signup and view all the flashcards
Inactive forms of enzymes
Inactive forms of enzymes
Signup and view all the flashcards
What is the Cephalic Phase?
What is the Cephalic Phase?
Signup and view all the flashcards
What are Micelles?
What are Micelles?
Signup and view all the flashcards
Bile salts recirculation
Bile salts recirculation
Signup and view all the flashcards
Gastrin
Gastrin
Signup and view all the flashcards
Ptyalin
Ptyalin
Signup and view all the flashcards
Proteolytic enzymes
Proteolytic enzymes
Signup and view all the flashcards
Bicarbonate
Bicarbonate
Signup and view all the flashcards
Bile salts
Bile salts
Signup and view all the flashcards
Brunner's glands
Brunner's glands
Signup and view all the flashcards
Crypts of Lieberkühn
Crypts of Lieberkühn
Signup and view all the flashcards
Fluid of HCO3
Fluid of HCO3
Signup and view all the flashcards
Second Portion of Liver Secretion
Second Portion of Liver Secretion
Signup and view all the flashcards
Bile Salts functions?
Bile Salts functions?
Signup and view all the flashcards
Enterohepatic Circulation of Bile Salts
Enterohepatic Circulation of Bile Salts
Signup and view all the flashcards
Secretin's Role in Bile Secretion
Secretin's Role in Bile Secretion
Signup and view all the flashcards
Three Factors That Stimulate Gastric Secretion
Three Factors That Stimulate Gastric Secretion
Signup and view all the flashcards
Interdigestive Period in the Stomach
Interdigestive Period in the Stomach
Signup and view all the flashcards
Study Notes
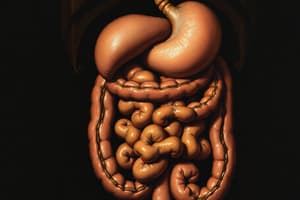
- Glands in the gastrointestinal tract secrete digestive enzymes and mucus for lubrication and protection.
- Secretions are formed in response to food presence, with the quantity varying in each tract segment.
- Enzyme types and secretion constituents change based on food types.
- The distal end of the ileum and the mouth to the anus are sites of digestive enzymes and mucous glands, respectively
Types of Alimentary Tract Glands
- Mucous cells (goblet cells) extrude mucus for lubrication and protection, responding to local irritation.
- Crypts of Lieberkühn invaginate into the submucosa and contain specialized secretory cells.
- Tubular glands, in the stomach and upper duodenum, secrete acid and pepsinogen.
- Complex glands; salivary glands, pancreas, and liver secrete for digestion or emulsification, comprised of acini lined with glandular cells that empty into ducts.
- Salivary glands and the pancreas lie outside the walls of the alimentary tract.
Stimulation of Alimentary Tract Glands
- Food stimulates glands to secrete juices in the region and adjacent areas.
- Mucous cell secretion results from direct contact stimulation.
- The enteric nervous system is activated by tactile stimulation, chemical irritation, and gut wall distention.
- This stimulates mucous cells and deep glands to increase secretion.
- Gut epithelium activates the enteric nervous system.
Autonomic Stimulation
- Parasympathetic stimulation increases glandular secretion rates in the upper tract, like salivary glands and the duodenum, and in the distal large intestine.
- Sympathetic stimulation causes a slight secretion increase and vasoconstriction, which reduces secretion if parasympathetic or hormonal stimulation is already causing copious secretion.
- Secretion in the small intestines occur mainly in response to local neutral and hormonal stimuli
Hormonal Regulation
- Gastrointestinal hormones regulate secretion volume and composition, liberated from the mucosa in response to food.
- These hormones, polypeptides or derivatives, stimulate secretion after absorption into the blood.
- Hormones are valuable to increase the amount of gastric and pancreatic juice when food enters the duodenum or stomach
Basic Mechanism of Secretion by Glandular Cells
- Nutrient material is diffused or actively transported into the glandular cell via capillaries.
- Mitochondria form adenosine triphosphate (ATP) with oxidative energy.
- Energy from ATP synthesizes organic secretory substances in the endoplasmic reticulum and Golgi complex.
- Ribosomes are responsible for secreted protein formation.
- Secretory materials pass through the endoplasmic reticulum tubules to Golgi complex vesicles in about 20 minutes.
- In the Golgi complex, materials are modified, concentrated, and discharged into vesicles stored in secretory cells.
- Hormonal or nervous control signals extrude vesicular contents, releasing calcium into the cell to fuse vesicles with the cell membrane, which breaks open in exocytosis.
Water and Electrolyte Secretion
- Hormones that act on the cell's membrane cause secretory effects, similar to nervous stimulation.
- Secretion necessitates sufficient water and electrolytes for organic substances to pass through.
Lubricating and Protective Properties of Mucus
- Mucus contains water, electrolytes, and glycoproteins for lubrication and protection.
- Mucus adheres to food and spreads as a film over surfaces.
- It coats the gut wall, preventing food contact with the mucosa.
- Mucus allows easy slippage with low resistance and causes fecal particles to adhere with resistance to digestion.
- Glycoproteins buffer acids or bases, often containing HCO3- to neutralize acids.
Secretion of Saliva
- Saliva contains serous secretion (ptyalin for digesting starches) and mucus secretion (mucin for lubrication and protection) from parotid, submandibular, sublingual, and buccal glands.
- Daily secretion ranges from 800 to 1500 ml with a pH between 6.0 and 7.0.
- Serous and mucous secretions differ, with parotid glands secreting serous secretion and submandibular/sublingual glands secreting both, while buccal glands secrete mucus.
Secretion of Ions in Saliva
- Saliva secretion occurs in two stages: acini and salivary ducts.
- The acini secrete ptyalin or mucin in an ionic solution.
- The salivary ducts reabsorb Na+ actively and secrete K+ actively, reducing Na+ concentration and increasing K+ concentration.
- Passive reabsorption of Cl- and secretion of HCO3- by the ductal epithelium occurs.
- Under resting conditions, saliva contains low Na+ and Cl- and high K+ and HCO3-.
- During maximal salivation, the acini secretion rate increases, reducing ductal reconditioning.
- Electrical negativity is created at -70mv due to the exchange of sodium and potassium
Function of Saliva for Oral Hygiene
- Saliva plays a key role in maintaining healthy oral tissues and preventing deterioration.
- Its flow washes away pathogenic bacteria and food particles.
- Saliva contains thiocyanate ions and proteolytic enzymes that destroy bacteria.
- It also contains antibodies that can destroy oral bacteria and prevent dental caries.
Nervous Regulation of Salivary Secretion
- The salivary glands are controlled by parasympathetic nervous signals from the brain stem’s salivatory nuclei.
- Taste and tactile stimuli from the mouth and pharynx excite the salivatory nuclei.
- Especially the sour taste elicits copious saliva secretion.
- Salivation can be stimulated or inhibited by signals from higher brain centers, like the appetite area in the hypothalamus.
- Reflexes originating in the stomach and upper small intestine also cause salivation.
- Sympathetic stimulation can cause slight salivation, forming thicker saliva than parasympathetic activity.
Secondary Factors & Blood Supply
- Adequate nutrients for the glands are required because secretion requires blood supply.
- Parasympathetic nerve signals and salivation dilate blood vessels and kallikrein stimulates bradykinin for vasodilation.
Esophageal Secretion
- Esophageal secretions consist entirely of mucus, preventing excoriation and protecting from acidic gastric juices.
Gastric Secretion
- The stomach mucosa has oxyntic glands, which secrete hydrochloric acid, pepsinogen, intrinsic factor, and mucus, and pyloric glands.
- Pyloric glands secrete mucus and gastrin.
- Oxyntic glands are located in the body and fundus, while pyloric glands are located in the antral stomach.
Secretions From Gastric (Oxyntic) Glands
- An oxyntic gland is composed of mucous neck cells, peptic cells, and parietal cells.
- Parietal cells: secrete hydrochloric acid and intrinsic factor.
- Peptic cells: secrete pepsinogen.
- Mucous neck cells: secrete mainly mucus.
- Some oxyntic glands also contain enterochromaffin-like cells (ECL) that secrete histamine.
- Hydrochloric acid secretion by parietal cells involves special mechanisms.
Mechanism of Hydrochloric Acid Secretion
- Parietal cells secrete an acid solution containing 160 mmol/L of hydrochloric acid when stimulated, with a pH of about 0.8.
- High H+ concentration requires energy.
- Bicarbonate diffuses so that gastric blood has a higher pH than that of arterial blood.
- The intracellular canaliculi is where hydrochloric acid forms.
Hydrochloric Acid Secretion
- The canaliculus consists of water, hydrochloric acid (150-160 mEq/L), potassium chloride (15 mEq/L), and sodium chloride.
- Gastric barrier prevents acid leakage to prevent damage to the mucosa
- Alkaline mucus, tight junctions, and toxic substances may damage that barrier
- Production of H+ requires minimal backleak into the mucosa of the secreted acid
Basic Factors That Stimulate Gastric Secretion
- Basic factors which stimulate gastric secretion include acetylcholine, gastrin, and histamine
- Acetylcholine excites secretion by peptic, parietal, and mucous cells.
- Gastrin and histamine strongly stimulate parietal cells’ acid secretion.
Pepsinogen Secretion and Activation
- Activation of pepsinogen depends on multiple types of pepsinogen that perform a specific functions
- Pepsinogen becomes activated when contacting hydrochloric acid, forming active pepsin.
- Pepsin functions as a proteolytic enzyme in an acidic environment.
- Hydrochloric acid is necessary for protein digestion in the stomach, similar to pepsin.
Intrinsic Factor
- The secretion of intrinsic factor is produced by parietal cells of the stomach that is essential for B12 absorption in the ileum
- Destruction of parietal cells may lead to achlorhydria or pernicious anemia.
Pyloric Glands Secretion
- Pyloric glands secrete alkaline and viscid mucus
- They are structurally similar to the oxyntic glands but contain mostly mucous cells and secrete gastrin, unlike other cells
Surface Mucous Cells
- Secrete the thick mucus coat on the stomachs outer surface
- Another characteristics is that they are alkaline that aren't directly exposed to any acidic or proteolytic stomachs
Stimulation of Gastric Acid Secretion
- The acidity of the fluid can be great, where the fluid in the glands can be great
- Parietal cells of the oxyntic glands are the only cells which secrete hydrochloric acid
Acid secretion in the stomach
- Acid secretion is highly regulated with both the endocrine and the nervous signals
- They operate in close association with the enterochromaffin which is to secrete histamine for hydrochloric acid formation
- Hydrochloric acid is only to be secreted if histamine has been released by the ECL cells
Regulation of Small Intestine Secretion
- The secretion of gastric acid stimulates gastrin
- The blood is also transported to the ECL cells of the stomach which transports to the blood
- histamine is what releases into the peptic acid which stimulates more acid secretions
Pepsinogen Secretion
- Pepsinogen is stimulated to be secreted in the stomachs
- They have the acetylcholine that us directly connected to the CNS
- They also rely acid in the stomach to further aid with the acid secretions
Phases of small intestine secretion
- They can occur in three forms, the cephalic, gastric and intestinal phases
- The cephalic phases is occurs when food enters the stomach
- It uses both the sense of smell and tasting for food
- Neurogenic signals originate in parts of the cerebral cortex, hypothalamus, and amygdala.
- The phase accounts for 30 percent of all stomach meal
The gastric phases
- Occurs when the food enter in the stomach to increase secretion
- It increases the vasovagal reflexes from the brain to the gut to have for the gastrin mechanism
- Accounts for 60 percent of the small intestine secretes
- It accounts for most of the small intestine secretion
Inhibition of gastric secretin intestinal factors
- The intestinal chyme stimulates smaller amount s for the gastric juices
- It has two influences with at least two
- The duodenum causes the stimulation with the prescence of acids, proteins, foods and hormone releases
- the reverse enterogastric reflex with the myenteric nervouss system for what is located in small
Gastric secretion
- During this time the stomach only secretes nonaxyntix with mucus
- The body of the small intestine secretes over 50 ml each hour
- Emotional stimulate the small intestine and cause it to be highly active for an inter digestion
Composition of gasstrin for the CNS
- Consists of large polypepetides that has molecaular weights as high as 2000 to 4200 by weight
- Function is resides in the terminal 4 of the of the acid groups
- Synthetic gstrin can lead all with the physiological for what is considered natural gastrins
The PancreaticSecretions
- The pancreas, secretes both digestive enzymes and bicarontaes to for digestion
- They flow through the pancreas which is the vatyer to the duodenum
- To break down chyme and or for food to travel in the small instetsines
- The pancreas also secretes insulin into the pancreastic juicer
- However the glands secretes this structure that can be located throughout pancreas
Pancerati enzymes
- Consists of many enzymes that are proteins, carbs and for fats
- Some consits of large amounts of CO3 which help neturazie
- Enterkinsea helps activate enzymes for the intersnetial tratc
- Trypsin is activated by the enzymes cause they secrete more of they
Inibitor for the tryspin for the digsetion
- The digstion has to become actiavted in the interned tracts
- Becuase if it does not then it will digsete into the small isntiens
- Trypsin inhibitor in pancreatic cells prevents trypsin activation inside secretory cells
Secrection of Bicarbonte Ions
- Although has 2 functions whcih will sectret from the cells adn for whater
- The HCO3 and water is the cell from to whihc it will then lead to the acini's
- Copious quantities of pancreatic juice allow the concentration of bicarbonate to rise to 145mEq
Regulation of Pancreatic secretions
- Relegation of the 3 secretions with are importatn during during pancrteic flow
- Acytlcholine has relaesed more and from other choingerl
- Choecytokinin which is located for the duodendeal
Multiplicative effects of secreteions
- when all the stimulus occure with the pancratix
- and if they do not at seperate its does not cause as much secreation
- therfore it must has to be the mutiple for all the stimulas for only that it can affect it
Phases of Pancreataic action
- the phases of with are the 3 which are the cephalci, gastric and intersetnal phases
- During that the cns signals increase secretions of in both the brain and stomachs 2 .During the interstinal phases after the chyme will become coppios which causes secretion within that specific hormones
Intestinal phases during secretion
- Secretins stimulates for Bicarbonata and neutalize acid contents
- With those 3 hormones whcih has around has 34 amino acids and the weight
Cholercistokinin controls eznymes
- Foods in the u[[er smal also causes hormones to relaease dfrom ther small inteatins
- This relaease cause with the fats and amino aids for what enters in to hte stetomachs
Bile to secrete hrugh teh
- One that can many of the fuctions and secretion form the licesr is
- And also play an imputabt role to for fat the desotion nad pasoribtions
Physiogolcal that has secretion
- Bile is serctret in that the two has that form
- is how the cell that consits fo rhte acid bile chlostrol and other stuff this relaeses in the form or in te small intestine
- . then will the bile flow in the small intestiens from the ducts which will then divert hte acid and wht it has int eh small iesnts is how the bile consset
Gaaldder of bile
- Galbradders can secrete form the cell from that the bile has secretred
- However teh volume fo that the gallbadder will has in around 30 o 60 mln for teh can haold
- Becuase ofr watr and electrolytes for what it relaes from the intestens
compsoiiton of biles
- bile is comrpised of the folwoing in the tabele that it displays when and then teh it becomes contested byhte gallbaldddert
- bile acid is the that the bile are sereted that the contednts are half teh solutes htat teh biLe Has
Cholcoykinim that stimules gallbladrd emptyying
- when foods begin to travel adn secrete throughout the body the small instiens will begins to mpty teh fodoss
- but if only emtpty with a small btu if it contains it mpty it quickler
- Gall Bladder is to secrete with the cholecstyimin with relaes a fat into the duodenum
Functions of Bile and fats.
- Liver makes bile salts 6G BY GIVING THE BIELS
- Cholesterol converts by both choeric fats for te cells with gives enrgey the acid
- Bile Salts has many action that cause
Bile salts action
- bile salts actisnos:
- has many actions that has the fats it contedns 2 It Helps with hte absortbions: fats, mono and and lipids 3.. detergent with the fats is for how the intestine tract to also take down the small fats
- the "ferried " will go to intestines ad what hte liver wil lmake bile to secrette
- Without of hte prescence of bile over 40 percents will lost and the metabilloci deficits will occur
- enterohepait circulation is how bile salt with recorculoated back in the bile
secretetion intestine fromt hhe muces
- An array for comopons which it is called brunner glands it lies i nthe wall of the small intstiens between the pyloris and the small testines and where that pancreatice secretinos for also from them
- Brunner glands secrete alkaline mucus to protect the duodenal wall from acidic gastric juice
bruners for secreetion stimulation
- This for which stimulated
- It hleps relaes form stimulas from small intestions in the walls to help reduce or reduce acid compaierds tp others
- Tactile or irtats stimulas from ht emucosa
- Vagal htat cuase increases and the stomach will start to
- Gastro with the secrtin
Secretion for digesetions for te juciers
- located ofr what is called juciers htat the cover the intestiens and the covers
- cells htat will secreted and elrctyes in the intersnes and and will
- Crypts of Lieberkühn are small that the pit calls the is in located throughout the intensines
- Vili's whcih also be the part for hte the surface for what the crypt and to absorb
Brunner’s Glands Stimulation and Inhibition
- Brunner's glands are stimulated by tactile or irritating stimuli, vagal stimulation, and gastrointestinal hormones.
- The glands are inhibited by sympathetic stimulation and protects the duodenal from the HCL acid.
Regulation of Small Intestine Secretion-Local Stimuli
- The most important regulation is through local enteric nervous reflexes that are caused by tactile or other irritating stimuli
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.