Podcast
Questions and Answers
What is the primary purpose of performing an endoscopic gastric mucosal biopsy in the context of gastritis?
What is the primary purpose of performing an endoscopic gastric mucosal biopsy in the context of gastritis?
- To evaluate the patient's psychological state and assess the impact of stress on gastric function.
- To measure the stomach's pH levels and determine the appropriate dosage of antacids.
- To identify and monitor various gastric conditions, assess H. pylori presence, and evaluate atrophy-related lesions. (correct)
- To assess the patient's overall nutritional status and identify dietary deficiencies.
When performing an endoscopic mucosal biopsy for gastritis, which of the following represents the MOST comprehensive approach to sample collection?
When performing an endoscopic mucosal biopsy for gastritis, which of the following represents the MOST comprehensive approach to sample collection?
- Submitting all biopsies in a single container to ensure efficient processing.
- Taking biopsies from the antrum and body only when lesions are present.
- Collecting biopsies exclusively from endoscopically visible lesions to target suspicious areas.
- Collecting biopsies from the greater and lesser curvatures in both the antrum and corpus, along with the incisura. (correct)
Which of the following statements accurately describes the defining characteristic of gastritis?
Which of the following statements accurately describes the defining characteristic of gastritis?
- Gastritis is characterized by inflammation of the gastric mucosa irrespective of the underlying cause. (correct)
- Gastritis is characterized by the accumulation of cholesterol plaques within the gastric arteries.
- Gastritis is solely determined by the presence of visible ulcers in the stomach lining.
- Gastritis is specifically caused by bacterial infections, primarily Helicobacter pylori.
Which of the following factors differentiates pangastritis from other forms of gastritis?
Which of the following factors differentiates pangastritis from other forms of gastritis?
A patient presents with gastritis that is described as occupying the entire mucosal thickness. Which of the following best characterizes this condition?
A patient presents with gastritis that is described as occupying the entire mucosal thickness. Which of the following best characterizes this condition?
A patient undergoing treatment for a chronic condition develops acute gastritis. Which of the following factors would MOST strongly suggest that the gastritis is acute rather than chronic?
A patient undergoing treatment for a chronic condition develops acute gastritis. Which of the following factors would MOST strongly suggest that the gastritis is acute rather than chronic?
Which of the following factors distinguishes acute erosive gastritis from other types of acute gastritis?
Which of the following factors distinguishes acute erosive gastritis from other types of acute gastritis?
A patient is diagnosed with acute hemorrhagic gastritis following a severe trauma. Which of the following pathogenic mechanisms is MOST likely contributing to the development of this condition?
A patient is diagnosed with acute hemorrhagic gastritis following a severe trauma. Which of the following pathogenic mechanisms is MOST likely contributing to the development of this condition?
A patient who has experienced a stressful event reports symptoms suggestive of acute gastritis. How long after the event does bleeding typically begin in these cases?
A patient who has experienced a stressful event reports symptoms suggestive of acute gastritis. How long after the event does bleeding typically begin in these cases?
Which of the following conditions is MOST closely associated with the development of Curling ulcers?
Which of the following conditions is MOST closely associated with the development of Curling ulcers?
What is the primary distinguishing feature between Curling and Cushing ulcers in acute hemorrhagic gastritis?
What is the primary distinguishing feature between Curling and Cushing ulcers in acute hemorrhagic gastritis?
Where are the lesions of acute hemorrhagic gastritis typically located within the stomach?
Where are the lesions of acute hemorrhagic gastritis typically located within the stomach?
What histopathological finding defines chronic gastritis?
What histopathological finding defines chronic gastritis?
Which cellular changes are commonly observed in the gastric mucosa of patients with chronic gastritis?
Which cellular changes are commonly observed in the gastric mucosa of patients with chronic gastritis?
Which of the following structural changes is typically associated with chronic gastritis?
Which of the following structural changes is typically associated with chronic gastritis?
What cellular feature characterizes intestinal metaplasia in the context of chronic gastritis?
What cellular feature characterizes intestinal metaplasia in the context of chronic gastritis?
Which type of intestinal metaplasia is associated with an increased risk of malignancy in chronic gastritis?
Which type of intestinal metaplasia is associated with an increased risk of malignancy in chronic gastritis?
In fundic (autoimmune) chronic gastritis (Type A), what specific region of the stomach is primarily affected by inflammation?
In fundic (autoimmune) chronic gastritis (Type A), what specific region of the stomach is primarily affected by inflammation?
Which of the following laboratory findings is MOST characteristic of fundic (autoimmune) chronic gastritis (Type A)?
Which of the following laboratory findings is MOST characteristic of fundic (autoimmune) chronic gastritis (Type A)?
What is the annual risk of adenocarcinoma associated with fundic (autoimmune) chronic gastritis (Type A)?
What is the annual risk of adenocarcinoma associated with fundic (autoimmune) chronic gastritis (Type A)?
In diffuse antral chronic gastritis (type B), which region of the stomach is predominantly involved?
In diffuse antral chronic gastritis (type B), which region of the stomach is predominantly involved?
Which of the following factors is MOST strongly associated with diffuse antral chronic gastritis (type B)?
Which of the following factors is MOST strongly associated with diffuse antral chronic gastritis (type B)?
Which of the following accurately describes the gastrin levels typically observed in diffuse antral chronic gastritis (type B)?
Which of the following accurately describes the gastrin levels typically observed in diffuse antral chronic gastritis (type B)?
Which type of chronic gastritis is associated with the highest risk of developing gastric adenocarcinoma?
Which type of chronic gastritis is associated with the highest risk of developing gastric adenocarcinoma?
What is the estimated prevalence of H. pylori infection in the developing world?
What is the estimated prevalence of H. pylori infection in the developing world?
What is the primary mechanism by which H. pylori contributes to tissue damage in the gastric mucosa?
What is the primary mechanism by which H. pylori contributes to tissue damage in the gastric mucosa?
Following successful eradication of H. pylori infection, which type of inflammatory cell infiltration resolves more quickly?
Following successful eradication of H. pylori infection, which type of inflammatory cell infiltration resolves more quickly?
Which virulence factor of H. pylori is associated with a greater risk of developing both adenocarcinoma and peptic ulcers?
Which virulence factor of H. pylori is associated with a greater risk of developing both adenocarcinoma and peptic ulcers?
Why is identification of H. pylori important in managing symptomatic gastritis patients?
Why is identification of H. pylori important in managing symptomatic gastritis patients?
Which of the following diagnostic methods involves administering radioactive carbon orally to detect H. pylori infection?
Which of the following diagnostic methods involves administering radioactive carbon orally to detect H. pylori infection?
What does a positive serology test for H. pylori antibodies (IgG) indicate?
What does a positive serology test for H. pylori antibodies (IgG) indicate?
Which of the following diseases is associated with H. pylori infection of the stomach?
Which of the following diseases is associated with H. pylori infection of the stomach?
In the context of gastritis, what information does an endoscopic gastric mucosal biopsy NOT provide?
In the context of gastritis, what information does an endoscopic gastric mucosal biopsy NOT provide?
Which of the following conditions is a direct indication for performing an endoscopic gastric mucosal biopsy?
Which of the following conditions is a direct indication for performing an endoscopic gastric mucosal biopsy?
Which of the following agents is least likely to cause gastritis?
Which of the following agents is least likely to cause gastritis?
Which of the following statements accurately describes the characteristics of acute gastritis?
Which of the following statements accurately describes the characteristics of acute gastritis?
Which diagnostic test can identify H. pylori based on urease production?
Which diagnostic test can identify H. pylori based on urease production?
Flashcards
Gastritis
Gastritis
Inflammation of the gastric mucosa, caused by chemicals, infections, radiation, or immunological factors.
Endoscopic Gastric Mucosal Biopsy
Endoscopic Gastric Mucosal Biopsy
For initial identification and monitoring of gastritis, peptic ulcer disease and gastric neoplasms.
Biopsy Locations in Gastritis
Biopsy Locations in Gastritis
Biopsies are usually taken from the body, antrum, and any endoscopically visible lesions.
Acute Gastritis
Acute Gastritis
Signup and view all the flashcards
Acute Gastritis Causes
Acute Gastritis Causes
Signup and view all the flashcards
Acute Hemorrhagic, Erosive Gastritis
Acute Hemorrhagic, Erosive Gastritis
Signup and view all the flashcards
Key Factors in Acute Hemorrhagic Erosive Gastritis
Key Factors in Acute Hemorrhagic Erosive Gastritis
Signup and view all the flashcards
Acute Gastritis Symptoms
Acute Gastritis Symptoms
Signup and view all the flashcards
Curling/Cushing Ulcers
Curling/Cushing Ulcers
Signup and view all the flashcards
Morphology of Acute Hemorrhagic Gastritis
Morphology of Acute Hemorrhagic Gastritis
Signup and view all the flashcards
Chronic Gastritis (CG)
Chronic Gastritis (CG)
Signup and view all the flashcards
Chronic Gastritis Associations
Chronic Gastritis Associations
Signup and view all the flashcards
Intestinal Metaplasia
Intestinal Metaplasia
Signup and view all the flashcards
Type I Intestinal Metaplasia
Type I Intestinal Metaplasia
Signup and view all the flashcards
Type III Intestinal Metaplasia
Type III Intestinal Metaplasia
Signup and view all the flashcards
Forms of Chronic Gastritis
Forms of Chronic Gastritis
Signup and view all the flashcards
Fundic (Type A) Chronic Gastritis
Fundic (Type A) Chronic Gastritis
Signup and view all the flashcards
Diffuse Antral (Type B) Chronic Gastritis
Diffuse Antral (Type B) Chronic Gastritis
Signup and view all the flashcards
Multifocal Chronic Atrophic (AB) Gastritis
Multifocal Chronic Atrophic (AB) Gastritis
Signup and view all the flashcards
H. pylori Gastritis
H. pylori Gastritis
Signup and view all the flashcards
H. Pylori Infection
H. Pylori Infection
Signup and view all the flashcards
H. pylori and Epithelial Cells
H. pylori and Epithelial Cells
Signup and view all the flashcards
H. pylori Virulence Factors
H. pylori Virulence Factors
Signup and view all the flashcards
H. pylori Detection Methods
H. pylori Detection Methods
Signup and view all the flashcards
H. pylori Related Diseases
H. pylori Related Diseases
Signup and view all the flashcards
Study Notes
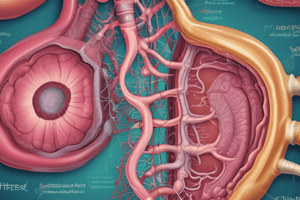
- Gastritis is the inflammation of the gastric mucosa, caused by chemicals, infectious agents, radiation, or immunological factors.
- Gastritis can manifest as pangastritis, antral, or corpus-specific issues, and it may be focal, diffuse, superficial, or affect the entire mucosal thickness.
Endoscopic Gastric Mucosal Biopsy
- It's used for identifying and monitoring various gastric conditions like gastritis, peptic ulcer disease, and gastric neoplasms.
- H pylori presence can be determined in the stomach using this biopsy.
- The grade, extent, and topography of gastritis and atrophy-related lesions can be assessed to determine the risk of gastric carcinoma.
- Biopsies are commonly taken from the body, antrum, and endoscopically visible lesions.
- Biopsies should be collected from five locations: greater and lesser curvatures in the antrum and corpus, and the incisura.
- Samples should be submitted in separate containers.
Classification of Gastritis
- Gastritis can be classified into acute and chronic types.
- Other classifications include:
- Aetiological: e.g., H pylori, mycobacterial, gastric syphilis, or fungal gastritis.
- Morphological: e.g., acute, erosive/hemorrhagic, lymphocytic, eosinophilic, or granulomatous gastritis.
- Mechanisms of injury: e.g., chemical or reactive gastropathy (reflux of bile & pancreatic secretion, alcohol, NSAIDs, chemotherapeutic drugs), and immune-mediated gastritis (autoimmune gastritis).
Acute Gastritis
- Frequently accompanied by acute mucosal injury, such as hemorrhagic or non-hemorrhagic, erosive or non-erosive.
- May result from disorders with various causes and diverse histologic patterns.
- Causes include drugs, uremia, ischemia, shock, corrosive agents, radiation, sepsis, trauma, certain infections, acute alcoholism, severe burns, alkaline reflux, bile reflux, major surgery, increased intracranial pressure, respiratory failure, portal hypertension, congestive heart failure, and multiorgan failure.
Acute Hemorrhagic, Erosive Gastritis
-
Characterized by necrosis, acute inflammatory response, and hemorrhage.
-
Erosion can extend into deeper tissue and form an ulcer.
-
Complications can include major physiologic disturbances like sepsis, extensive burn injury, head injury, severe trauma, and multiorgan failure.
-
Associated with aspirin, NSAID, alcohol intake and ischemic injuries, which directly damage the mucosa.
-
Breakdown of the mucosal barrier permits acid-induced injury.
-
Major factors implicated are hyperchlorhydria and decreased mucosal protection, such as decreased mucous secretion or mucosal blood flow.
-
Acute gastritis often presents as abdominal discomfort and pain, heartburn, nausea, vomiting, and haematemesis.
-
Bleeding begins 3 to 7 days after a stressful event, ranging from occult blood to massive hemorrhage.
Specific Forms of Acute Hemorrhagic Gastritis
- Curling ulcer: develops in severe burn patients within 24-72 hours, likely due to ischemia.
- Cushing ulcer: occurs after accidental or surgical CNS trauma, increased vagal tone leads to increased acid secretion in cerebral injury.
Morphology of Acute Hemorrhagic Gastritis
- Typically appears as multiple lesions in the stomach, predominantly in the oxyntic mucosa.
- It can cause widespread petechial hemorrhages or submucosal bleeding.
- Lesions vary from 1-25mm across and may appear as sharply punched-out ulcers.
- Curling and Cushing ulcers tend to be deep and single.
Chronic Gastritis
- Histopathologic condition marked by inflammation of the gastric mucosa.
- Composed of a heterogeneous group of disorders, each with unique location, causes and resulting complications.
- It's defined by an elevation of lymphocytes and plasma cells in the lamina propria.
- Can range from a mild superficial lesion to severe atrophy.
- The main symptom is dyspepsia, though many are asymptomatic.
- Usually associated with active inflammation (congestion, edema, neutrophils), atrophy (decrease in normal glandular cells), and intestinal metaplasia (replacement of the surface, foveolae, and glandular epithelial cells with intestinal goblet cells).
Types of Intestinal Metaplasia
- Type I (complete): small intestinal type cells with brush borders and goblet cells with acidic mucin, with no malignancy risk.
- Type II (incomplete): colonic type goblet cells with sialomucin, doesn't increase malignancy risk.
- Type III (incomplete): colonic type goblet cells with sulfomucin, associated with potential increased risk of malignancy.
Pathogenesis of Chronic Gastritis
- There are 3 forms:
- Fundic or autoimmune chronic gastritis "Type A": inflammation restricted to the body and fundus, associated with Pernicious anemia, parietal cell and intrinsic factor antibodies, reduced gastric secretion, and increased gastrin secretion; adenocarcinoma risk is 0.5% per year.
- Diffuse antral chronic gastritis "Type B": involves the antrum and is associated with H pylori, peptic duodenitis, chronic peptic ulcers in the duodenum and prepyloric region, hyperchlorhydria, and no parietal or intrinsic antibodies; adenocarcinoma risk is low.
- Multifocal chronic atrophic gastritis "Type AB": associated with H pylori, gastric ulcers, and is at the highest risk for developing gastric adenocarcinoma.
H Pylori-Associated Gastritis
- H pylori is commonly the main cause of chronic gastritis.
- Approximately half the world’s population is affected by H pylori, with a prevalence of 70-90% in developing countries.
- Infection is more common in lower socioeconomic levels, and those affected are largely asymptomatic.
- H pylori colonizes and infects the gastric mucosa, with infections usually begin in childhood.
- Associated with tissue damage, active and chronic gastritis.
- The interaction of H pylori with surface mucosa leads to interleukin-8 release, which recruits polymorphs.
- Gastric epithelial cells express class II molecules, which present H pylori antigens, boosting cytokine release .
- Neutrophilic infiltration leads to elevated leukotriene levels, esp. leukotriene B4, is cytotoxic to gastric epithelium.
- Neutrophilic infiltration reduces quickly, but chronic inflammatory cells resolves more slowly.
Virulence Factors of H Pylori
- Vacuolating toxin A "VacA": H pylori strains that produce VacA are more likely to cause peptic ulcers.
- Coagulating antigen A "CagA": associated with a greater risk of adenocarcinoma and peptic ulcers.
- Strains lacking cagA can still cause adenocarcinoma and peptic ulcers.
Methods for Detecting H Pylori
- Histomorphology: from endoscopic biopsy using H&E, Giemsa, or Warthin-Starry stain; immunohistochemistry.
- Rapid urease test: detects urease produced by the organism acting on urea to generate NH3, with 85% sensitivity.
- Urea breath test: radioactive carbon measured in expired CO2, with 95% sensitivity.
- Serology test: detects H pylori antibodies
- Fecal antigen test: 90% sensitivity.
Diseases Associated with H Pylori Infection
- Gastric adenocarcinoma
- Malignant lymphoma arising in MALT
- Duodenal ulcer and nonulcer dyspepsia
- Gastric ulcer
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.