Podcast
Questions and Answers
What is the primary function of the gallbladder?
What is the primary function of the gallbladder?
- To detoxify blood
- To absorb nutrients
- To produce bile
- To receive and concentrate bile (correct)
Which structure directly connects the gallbladder to the common hepatic duct?
Which structure directly connects the gallbladder to the common hepatic duct?
- Cystic duct (correct)
- Common bile duct
- Hepatic vein
- Pancreatic duct
What surrounds the terminal parts of the bile duct and pancreatic duct in the duodenum?
What surrounds the terminal parts of the bile duct and pancreatic duct in the duodenum?
- Connective tissue
- Circular muscle (correct)
- Mucosal layer
- Smooth muscle
Which artery supplies blood to the gallbladder?
Which artery supplies blood to the gallbladder?
What structure is located near the neck of the gallbladder and is involved in lymph drainage?
What structure is located near the neck of the gallbladder and is involved in lymph drainage?
Where does the common bile duct typically open into?
Where does the common bile duct typically open into?
Which of the following is NOT a part of the gallbladder?
Which of the following is NOT a part of the gallbladder?
Which part of the liver is the gallbladder associated with?
Which part of the liver is the gallbladder associated with?
What hormone is responsible for the contraction of the gallbladder in response to fatty food?
What hormone is responsible for the contraction of the gallbladder in response to fatty food?
Which part of the pancreas lies within the concavity of the duodenum?
Which part of the pancreas lies within the concavity of the duodenum?
Which duct of the pancreas directly joins the common bile duct?
Which duct of the pancreas directly joins the common bile duct?
Which part of the pancreas is considered retroperitoneal?
Which part of the pancreas is considered retroperitoneal?
What is the primary function of the exocrine portion of the pancreas?
What is the primary function of the exocrine portion of the pancreas?
Which arteries supply blood to the pancreas?
Which arteries supply blood to the pancreas?
Which statement correctly describes the pancreatic ducts?
Which statement correctly describes the pancreatic ducts?
The tail of the pancreas ends as it passes between which structures?
The tail of the pancreas ends as it passes between which structures?
What is the primary function of the portal vein?
What is the primary function of the portal vein?
From which veins does the portal vein form?
From which veins does the portal vein form?
Where does the portal vein enter the liver?
Where does the portal vein enter the liver?
What occurs during portosystemic anastomosis?
What occurs during portosystemic anastomosis?
Which of the following is NOT a tributary of the portal vein?
Which of the following is NOT a tributary of the portal vein?
Which part of the body contains anastomoses between the portal and systemic circulation?
Which part of the body contains anastomoses between the portal and systemic circulation?
Where are lymph nodes primarily located in relation to the spleen?
Where are lymph nodes primarily located in relation to the spleen?
What anatomical feature allows the spleen to connect to the stomach?
What anatomical feature allows the spleen to connect to the stomach?
How does the body compensate for increased portal vein pressure?
How does the body compensate for increased portal vein pressure?
What is the significance of Caput Medusae related to portal hypertension?
What is the significance of Caput Medusae related to portal hypertension?
What is the primary role of the splenic hilum?
What is the primary role of the splenic hilum?
Which organ lies along the medial border of the spleen?
Which organ lies along the medial border of the spleen?
How does the splenic artery travel in relation to the pancreas?
How does the splenic artery travel in relation to the pancreas?
Which structure is NOT part of the greater omentum as it relates to the spleen?
Which structure is NOT part of the greater omentum as it relates to the spleen?
Which vessels drain lymphatic fluid from the spleen?
Which vessels drain lymphatic fluid from the spleen?
What anatomical position describes the spleen's relation to the diaphragm?
What anatomical position describes the spleen's relation to the diaphragm?
Study Notes
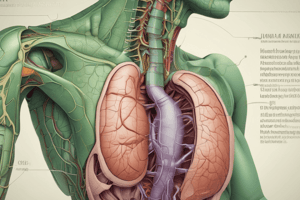
Gallbladder
- Pear-shaped sac located on the right lobe of the liver
- Divided into the fundus, body, and neck
- Receives, concentrates, and stores bile from the liver
- Surrounded by peritoneum
- Anteriorly related to the anterior abdominal wall and the inferior surface of the liver
- Posteriorly related to the transverse colon and the first and second parts of the duodenum
- Neck connects to the cystic duct, joining the common hepatic duct to form the common bile duct
Common Bile Duct
- Approximately 8 cm long
- Lies in the right free margin of the lesser omentum
- Pierces the medial wall of the second part of the duodenum
- Joins the main pancreatic duct to form the hepatopancreatic ampulla (ampulla of Vater)
- Terminal parts of both ducts and the ampulla are surrounded by the sphincter of the hepatopancreatic ampulla (sphincter of Oddi)
Gallbladder Blood Supply
- Supplied by the cystic artery, a branch of the right hepatic artery
- Drained by the cystic vein, which empties into the portal vein
- Lymph drains into a cystic lymph node near the neck, then to hepatic nodes, and finally to celiac nodes
- Innervated by sympathetic and parasympathetic vagal fibers forming the celiac plexus
Pancreas
- Both an exocrine and endocrine gland
- Exocrine portion produces enzymes for digesting proteins, fats, and carbohydrates
- Endocrine portion, the pancreatic islets (islets of Langerhans), produces insulin and glucagon, which regulate carbohydrate metabolism
- Located mostly posterior to the stomach
- Extends across the posterior abdominal wall from the duodenum to the spleen
- Retroperitoneal except for a small part of the tail
- Divided into head, uncinate process, neck, body, and tail
- Head lies within the C-shaped concavity of the duodenum
- Uncinate process projects from the lower part of the head
- Neck sits anterior to the superior mesenteric vessels
- Tail ends between layers of the splenorenal ligament
Pancreatic Duct
- Begins in the tail, runs through the body, and turns inferiorly in the head
- Joins the bile duct in the lower part of the head
- Forms the hepatopancreatic ampulla (ampulla of Vater) with the common bile duct, which enters the descending duodenum at the major duodenal papilla
- Accessory pancreatic duct opens into the duodenum above the major duodenal papilla at the minor duodenal papilla
- Main and accessory pancreatic ducts often communicate
Pancreas Blood Supply
- Supplied by the splenic and superior and inferior pancreaticoduodenal arteries
- Drained by corresponding veins into the portal system
- Lymph nodes are situated along the arteries, draining into celiac and superior mesenteric lymph nodes
Spleen
- Largest single mass of lymphoid tissue in the body
- Develops as part of the vascular system in the dorsal mesentery
- Red, oval-shaped with a notched anterior border
- Located beneath the left diaphragm, close to the 9th, 10th, and 11th ribs
- Lower pole extends to the mid-axillary line
- Surrounded by peritoneum and connected to:
- Greater curvature of the stomach by the gastrosplenic ligament, containing short gastric and gastro-omental vessels
- Left kidney by the splenorenal ligament, containing splenic vessels and tail of pancreas
- Both ligaments are parts of the greater omentum
- Surrounded by visceral peritoneum, except at the hilum on the medial surface
- Hilum is the entry point for splenic vessels and the tail of the pancreas
Spleen Location
- Anteriorly related to:
- Stomach
- Tail of the pancreas
- Left colic flexure
- Left kidney along its medial border
- Posteriorly related to:
- Diaphragm
- Left pleura (left costodiaphragmatic recess)
- Left lung
- 9th, 10th, and 11th ribs
Spleen Blood Supply
- Supplied by the splenic artery, the largest branch of the celiac artery
- Splenic vein leaves the hilum, runs behind the tail and body of the pancreas
- Joins the superior mesenteric vein behind the neck of the pancreas to form the portal vein
- Lymph vessels from the hilum drain into nodes along the splenic artery and then into the celiac nodes
Spleen Functions
- Mechanical filtration of red blood cells
- Active immune response
- Produces all types of blood cells during fetal life
- Stores red blood cells, lymphocytes, and other formed elements
Portal Venous System
- Final common pathway for venous blood from the abdominal part of the gastrointestinal tract, spleen, pancreas, and gallbladder
- About 2 in. (5 cm) long
- Formed by the union of the splenic vein and the superior mesenteric vein posterior to the neck of the pancreas at the level of vertebra L2
- Ascends toward the liver, passes behind the first part of the duodenum and enters the right margin of the lesser omentum
- Sits anterior to the omental foramen and posterior to the bile duct and the hepatic artery proper
- Enters the liver after dividing into right and left branches
Portal Vein Tributaries
- Splenic vein
- Left gastric vein
- Right gastric vein
- Cystic vein
- Inferior mesenteric vein
- Superior mesenteric vein
Portosystemic Anastomosis
- Connections between veins of the portal circulation and those of the systemic circulation
- Allows for blood flow to bypass the liver during elevated portal vein pressure (e.g. cirrhosis)
- Collateral channels drain into the systemic circulation at specific points:
- Lower part of the esophagus (left gastric and azygos veins)
- Rectum (superior and inferior rectal veins)
- Paraumbilical (paraumbilical and superficial epigastric veins)
- Retroperitoneal (splenic and renal veins)
- Intrahepatic (left branch of portal vein and inferior vena cava)
Caput Medusae
- Distinctive pattern of dilated veins around the umbilicus, indicative of portal hypertension
- Occurs due to the paraumbilical portosystemic anastomosis
- Systemic blood flow is rerouted through these veins due to increased pressure in the portal system
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the anatomy of the gallbladder and common bile duct with this quiz. Learn about their structure, blood supply, and relational anatomy with surrounding organs. Perfect for students studying human anatomy and physiology.