Podcast
Questions and Answers
What is the appropriate position for a patient during repositioning to prevent risk for shearing and friction injuries?
What is the appropriate position for a patient during repositioning to prevent risk for shearing and friction injuries?
30-degree lateral position
What stage of pressure ulcer does not require a dressing?
What stage of pressure ulcer does not require a dressing?
- III
- I (correct)
- IV
- II
What should the nurse do to decrease a patient's anxiety when changing a dressing?
What should the nurse do to decrease a patient's anxiety when changing a dressing?
- Explain the procedure (correct)
- Ask the family to leave the room
- Tell the patient to close his eyes
- Turn on the television
Which intervention should be included while cleansing a wound site?
Which intervention should be included while cleansing a wound site?
What is the best explanation for using an abdominal binder after an open abdominal aortic aneurysm repair?
What is the best explanation for using an abdominal binder after an open abdominal aortic aneurysm repair?
Which intervention should the nurse implement for pain management following a postoperative medial meniscus repair?
Which intervention should the nurse implement for pain management following a postoperative medial meniscus repair?
What score on the Braden scale indicates decreasing risk for skin breakdown?
What score on the Braden scale indicates decreasing risk for skin breakdown?
Which consults should always be included for a patient with a stage II pressure ulcer?
Which consults should always be included for a patient with a stage II pressure ulcer?
Which factors influence wound healing by tertiary intention?
Which factors influence wound healing by tertiary intention?
Which nursing assessment questions should be included in a skin integrity assessment?
Which nursing assessment questions should be included in a skin integrity assessment?
Which components should the nurse include in a skin assessment for potential skin breakdown?
Which components should the nurse include in a skin assessment for potential skin breakdown?
What should the nurse do before applying a large abdominal bandage and binder?
What should the nurse do before applying a large abdominal bandage and binder?
Which outcomes indicate progression toward goals for a patient with a stage III pressure ulcer?
Which outcomes indicate progression toward goals for a patient with a stage III pressure ulcer?
Which risk factor predisposes a patient to pressure ulcer development?
Which risk factor predisposes a patient to pressure ulcer development?
What is the major element involved in the development of a decubitus ulcer?
What is the major element involved in the development of a decubitus ulcer?
Which nursing observation indicates a patient is at risk for pressure ulcer formation?
Which nursing observation indicates a patient is at risk for pressure ulcer formation?
How would the nurse stage a healing stage III pressure ulcer?
How would the nurse stage a healing stage III pressure ulcer?
What stage is a shallow open ulcer without slough on the right heel?
What stage is a shallow open ulcer without slough on the right heel?
Which assessment would be used first to assist in staging an ulcer on a patient with darkly pigmented skin?
Which assessment would be used first to assist in staging an ulcer on a patient with darkly pigmented skin?
What type of wound healing occurs for a stage IV pressure ulcer?
What type of wound healing occurs for a stage IV pressure ulcer?
If a wound is kept moist, it can resurface in how many days?
If a wound is kept moist, it can resurface in how many days?
What should the nurse expect to see in a full-thickness repair?
What should the nurse expect to see in a full-thickness repair?
A laparoscopic appendectomy wound heals by which intention?
A laparoscopic appendectomy wound heals by which intention?
A burn wound heals by which intention?
A burn wound heals by which intention?
What indicates a wound healed by secondary intention?
What indicates a wound healed by secondary intention?
What nursing observation indicates a complication of wound healing after a total hysterectomy?
What nursing observation indicates a complication of wound healing after a total hysterectomy?
Which finding in a postoperative patient should the nurse associate with dehiscence?
Which finding in a postoperative patient should the nurse associate with dehiscence?
What laboratory data is important to gather for a patient with a decubitus ulcer?
What laboratory data is important to gather for a patient with a decubitus ulcer?
What is the most important piece of assessment data for wound healing?
What is the most important piece of assessment data for wound healing?
What should the nurse do when noticing signs of infection in a healing stage III pressure ulcer?
What should the nurse do when noticing signs of infection in a healing stage III pressure ulcer?
What is the nurse's assessment related to a patient's psychological response to a wound?
What is the nurse's assessment related to a patient's psychological response to a wound?
After determining that a patient is stable, what is the next best step for a laceration?
After determining that a patient is stable, what is the next best step for a laceration?
When caring for a patient with a wound that needs changing, what should the nurse do first?
When caring for a patient with a wound that needs changing, what should the nurse do first?
What is the next best step if a drainage collection device shows a sudden decrease in drainage?
What is the next best step if a drainage collection device shows a sudden decrease in drainage?
Which specialty bed is most appropriate for a patient with a stage IV pressure ulcer?
Which specialty bed is most appropriate for a patient with a stage IV pressure ulcer?
What is the next step in caring for a patient with a black pressure ulcer?
What is the next step in caring for a patient with a black pressure ulcer?
What order should the nurse question for a patient with a clean stage III pressure ulcer?
What order should the nurse question for a patient with a clean stage III pressure ulcer?
Which assessment is essential when evaluating a patient's skin integrity?
Which assessment is essential when evaluating a patient's skin integrity?
What would be the Braden scale total score for a patient with specific risk factors?
What would be the Braden scale total score for a patient with specific risk factors?
What intervention is most important to decrease the risk of pressure ulcers for an immobile patient?
What intervention is most important to decrease the risk of pressure ulcers for an immobile patient?
What nursing diagnosis is appropriate for a patient with a stage IV pressure ulcer?
What nursing diagnosis is appropriate for a patient with a stage IV pressure ulcer?
What nursing diagnosis should be assigned for a patient with a reddened area on the heel that does not blanch?
What nursing diagnosis should be assigned for a patient with a reddened area on the heel that does not blanch?
What is the most important intervention for a patient with a stage II pressure ulcer at risk for infection?
What is the most important intervention for a patient with a stage II pressure ulcer at risk for infection?
Which professional should the nurse consult for optimal nutrition to promote wound healing?
Which professional should the nurse consult for optimal nutrition to promote wound healing?
What is the best goal for an unconscious and bedridden patient with a stage II pressure ulcer?
What is the best goal for an unconscious and bedridden patient with a stage II pressure ulcer?
What risk does a postpartum patient with an episiotomy face when heat treatment is applied incorrectly?
What risk does a postpartum patient with an episiotomy face when heat treatment is applied incorrectly?
Which intervention assists in managing expenses associated with long-term wound care?
Which intervention assists in managing expenses associated with long-term wound care?
What initial intervention should the nurse select to decrease skin impairment for a patient with mobility problems?
What initial intervention should the nurse select to decrease skin impairment for a patient with mobility problems?
How long should a patient be scheduled to sit in a chair to prevent skin impairment?
How long should a patient be scheduled to sit in a chair to prevent skin impairment?
What is the best method for repositioning a patient at risk for skin impairment?
What is the best method for repositioning a patient at risk for skin impairment?
Flashcards
Confusion and Pressure Ulcers
Confusion and Pressure Ulcers
Confusion or disorientation prevents patients from recognizing and relieving pressure, increasing ulcer risk.
Additional Risk Factors
Additional Risk Factors
Impaired sensory perception, impaired mobility, shear, friction, and moisture are key factors that increase risk.
Primary Cause of Decubitus Ulcers
Primary Cause of Decubitus Ulcers
Pressure is the primary cause of decubitus ulcers, its intensity, duration, and tissue tolerance impacting ulcer development.
Ischemic Injury
Ischemic Injury
Signup and view all the flashcards
Skin Breakdown Time
Skin Breakdown Time
Signup and view all the flashcards
Fecal Incontinence and Risk
Fecal Incontinence and Risk
Signup and view all the flashcards
Healing Pressure Ulcer Staging
Healing Pressure Ulcer Staging
Signup and view all the flashcards
Stage II Ulcer Description
Stage II Ulcer Description
Signup and view all the flashcards
Lighting for Skin Assessment
Lighting for Skin Assessment
Signup and view all the flashcards
Lighting Distortion
Lighting Distortion
Signup and view all the flashcards
Pressure Ulcer Healing
Pressure Ulcer Healing
Signup and view all the flashcards
Tissue Regeneration Healing
Tissue Regeneration Healing
Signup and view all the flashcards
Wound Resurfacing Time
Wound Resurfacing Time
Signup and view all the flashcards
Epithelial Proliferation
Epithelial Proliferation
Signup and view all the flashcards
Granulation Tissue Significance
Granulation Tissue Significance
Signup and view all the flashcards
Wound Complications Indicators
Wound Complications Indicators
Signup and view all the flashcards
Hematoma as a Complication
Hematoma as a Complication
Signup and view all the flashcards
Dehiscence
Dehiscence
Signup and view all the flashcards
Protein and Wound Healing
Protein and Wound Healing
Signup and view all the flashcards
Essential Nutrients for Healing
Essential Nutrients for Healing
Signup and view all the flashcards
Psychological Impact of Wounds
Psychological Impact of Wounds
Signup and view all the flashcards
Emotional Response to Wounds
Emotional Response to Wounds
Signup and view all the flashcards
Initial Laceration Assessment
Initial Laceration Assessment
Signup and view all the flashcards
Further Laceration Assessment
Further Laceration Assessment
Signup and view all the flashcards
Pain Management Before Dressing Changes
Pain Management Before Dressing Changes
Signup and view all the flashcards
Decreased Drainage
Decreased Drainage
Signup and view all the flashcards
Low-Air-Loss Therapy
Low-Air-Loss Therapy
Signup and view all the flashcards
Débridement for Pressure Ulcers
Débridement for Pressure Ulcers
Signup and view all the flashcards
Skin Integrity Assessment
Skin Integrity Assessment
Signup and view all the flashcards
Braden Scale
Braden Scale
Signup and view all the flashcards
Primary Infection Prevention
Primary Infection Prevention
Signup and view all the flashcards
Pain Control and Mobility
Pain Control and Mobility
Signup and view all the flashcards
Patient Involvement in Wound Care
Patient Involvement in Wound Care
Signup and view all the flashcards
Cleaning Wound Direction
Cleaning Wound Direction
Signup and view all the flashcards
Clean Techniques in Home Care
Clean Techniques in Home Care
Signup and view all the flashcards
Study Notes
Risk Factors for Pressure Ulcers
- Confusion or disorientation prevents patients from recognizing and relieving pressure, increasing ulcer risk.
- Key additional predisposing factors: impaired sensory perception, impaired mobility, shear, friction, and moisture.
- Diet low in calories and fat, muscular pain, and shortness of breath are not recognized risk factors.
Primary Causes of Decubitus Ulcers
- Pressure remains the primary cause, with intensity, duration, and tissue tolerance critical in ulcer development.
- Ischemic injury can occur when pressure exceeds 12 to 32 mm Hg on capillaries.
- Skin breakdown may arise from both high pressure over a short period and low pressure over longer durations.
Indicators of Pressure Ulcer Risk
- Fecal incontinence significantly heightens the risk due to prolonged moisture on the skin.
- Other observations, such as food intake or mild skin irritations, do not indicate imminent risk for pressure ulcers.
Staging of Pressure Ulcers
- A healing pressure ulcer retains its stage designation (e.g., a stage III ulcer that is healing is termed a "healing stage III pressure ulcer").
- Stage II ulcers exhibit partial-thickness skin loss without slough, presenting as abrasions or blisters.
Importance of Lighting in Skin Assessment
- Halogen or natural light is essential for accurate skin assessments, especially on patients with darkly pigmented skin.
- Incorrect lighting can distort assessment findings, preventing proper identification of skin issues.
Types of Wound Healing
- Pressure ulcers are examples of full-thickness wounds healing by scar formation.
- Wounds healing primarily through tissue regeneration involve minimal tissue loss and include procedures like laparoscopic surgeries.
Resurfacing of Wounds
- Wounds that are kept moist can resurface within 4 days, while those exposed to air may take up to 6-7 days.
- The timeframe for epithelial proliferation varies based on the type of wound care provided.
Healing Characteristics
- Granulation tissue indicates positive healing progression in full-thickness wounds.
- Presence of eschar, slough, or purulent drainage signifies complications such as infection or improper healing.
Complications in Wound Healing
- A hematoma, characterized by bluish discoloration and swelling, indicates possible complications and requires careful monitoring.
- Dehiscence is signaled by patient complaints of a sensation of something "giving way."
Nutritional Support for Wound Healing
- Protein is crucial for effective wound healing; it supports physiological processes involved in tissue repair.
- Vitamins A and C, along with zinc and copper, are also essential for optimal healing, while fats and carbohydrates do not require special increases.
Psychological Impact of Wounds
- Patients' concerns about appearance and odor from wounds can affect self-concept, indicating psychological distress.
- Responses to wound conditions can reveal underlying feelings about body image and healing progress.
Emergency Care for Lacerations
- Initial action should focus on inspecting the wound for bleeding.
- Subsequent assessments should include checking for foreign bodies and assessing the need for tetanus prophylaxis.
Priorities in Wound Care
- Before changing dressings or managing drainage, it’s vital to gather all necessary supplies to ensure an efficient and organized approach to wound care.### Wound Care and Pressure Ulcer Management
- Administer analgesics 30 minutes prior to dressing changes to minimize pain associated with removal.
- Sudden decrease in wound drainage requires assessment for blockage; notify the physician if suspected.
- Low-air-loss therapy units are effective for patients with stage IV pressure ulcers to prevent skin breakdown.
- Débridement is essential for necrotic tissue to promote healing and prevent infection in pressure ulcers.
- Use noncytotoxic cleansers like normal saline for clean granulating wounds to avoid harming healing tissue.
Skin Integrity Assessment
- Regularly assess skin for signs of ulcer development; monitor pressure points and bony prominences.
- Braden scale scores assist in assessing a patient's risk for skin breakdown based on sensory perception and mobility.
- Nursing diagnoses related to skin include "Impaired skin integrity" for patients with stage IV pressure ulcers and "Ineffective tissue perfusion" for areas with redness that does not blanch.
Infection Risk and Prevention
- Hand hygiene is the primary intervention to prevent infection in patients with pressure ulcers.
- Consult a registered dietitian to optimize the diet for wound healing.
- Educate families about infection signs and wound care, particularly for unconscious or bedridden patients.
Patient Mobility and Repositioning
- Encourage adequate pain control to increase patient comfort and mobility, thus reducing pressure ulcer risk.
- Limit chair sitting time to 2 hours, using cushions to alleviate pressure.
- When repositioning, utilize safe methods like a transfer sliding board to avoid shearing forces.
Dressing Changes and Patient Comfort
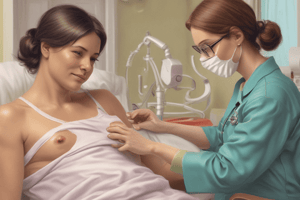
- Explain dressing change procedures to alleviate patient anxiety and involve them in their care.
- Clean wounds in a direction from least to most contaminated to minimize infection risk.
- Abdominal binders support large incisions post-surgery, particularly during movement and coughing.
General Care Strategies
- Employ clean techniques for dressing changes in home care to manage costs and reduce infection risk.
- Position patients appropriately to reduce pressure and improve comfort, adjusting care based on individual capabilities and needs.### Postoperative Care for Medial Meniscus Repair
- Pain management post-surgery includes elevating the knee and applying ice to minimize edema and control bleeding.
- Brace application is supportive but does not directly manage pain.
- Vital signs monitoring is routine but not a direct pain intervention.
- Pulses should be checked to ensure circulation, not specifically for pain management.
Braden Scale Assessment
- Braden scale scores range from 6 (high risk) to 23 (low risk); a score of 18 indicates pressure ulcer risk.
- A score of 23 signifies optimal skin integrity and a decreasing risk for skin breakdown after interventions.
Multi-disciplinary Approach for Pressure Ulcers
- Consults for patients with stage II pressure ulcers should include:
- Registered dietitian for nutritional support.
- Wound care nurse specializing in wound management.
- Physical therapist to enhance mobility and minimize risk.
- Case management for arranging outside care.
- Spiritual or medication needs are generally secondary and not core consults unless necessary.
Factors Influencing Wound Healing
- Key influencing factors include:
- Nutrition: Essential for repair.
- Tissue perfusion: Adequate oxygen significantly aids healing.
- Infection: Delays healing and increases tissue damage.
- Age: Older patients experience delayed healing.
- Evisceration and hemorrhage are complications but not direct influences on the healing process.
Skin Integrity Assessment Questions
- Important questions during skin integrity assessment include:
- Ability to change positions to reduce pressure.
- Sensitivity to temperature for self-protection.
- Frequency of toileting to assess incontinence risk.
- Pain during movement indicating mobility issues.
Components of Skin Assessment
- Skin assessment involves evaluating:
- Hyperemia: Observing abnormal reactions post blood flow obstruction.
- Induration: Detecting hard areas on the skin.
- Blanching: Testing reddened areas for circulation recovery.
- Skin temperature: Monitoring for blood flow changes.
- Mobility and nutritional status are crucial but are overall assessment aspects rather than direct skin assessment components.
Responsibilities Before Applying Bandages
- Inspect for abrasions, edema, and skin integrity.
- Cover exposed wounds with sterile dressings.
- Assess current dressing conditions for needed changes.
- Evaluate the skin beneath the bandage for circulatory integrity.
Outcomes Indicating Progress in Pressure Ulcer Care
- Positive outcomes toward improving skin integrity include:
- Preventing injury to skin and tissues.
- Reducing various levels of skin and tissue injury.
- Restoring skin integrity.
- Patient expectations and perceptions provide useful feedback but are not direct measurable outcomes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge on skin integrity and wound care with these practice questions. This quiz focuses on key concepts and risk factors related to pressure ulcers as discussed in Chapter 48 of the Fundamentals of Nursing. Improve your understanding and readiness for the clinical application of wound care principles.