Podcast
Questions and Answers
What is the primary risk factor for the development of Ms. Pimm's stage 3 pressure injury?
What is the primary risk factor for the development of Ms. Pimm's stage 3 pressure injury?
- Pressure from the knee brace (correct)
- Prolonged immobility
- Poor dietary habits
- Recent surgery
Which dietary concern should be monitored closely for Ms. Pimm?
Which dietary concern should be monitored closely for Ms. Pimm?
- Inadequate calories
- Low calcium levels
- High sodium intake (correct)
- High fiber intake
What behavior might impact Ms. Pimm's recovery negatively?
What behavior might impact Ms. Pimm's recovery negatively?
- Seeking emotional support
- Eating a balanced diet
- Regular physical exercise
- Smoking tobacco (correct)
What psychosocial factor may affect Ms. Pimm's emotional well-being during recovery?
What psychosocial factor may affect Ms. Pimm's emotional well-being during recovery?
What should be the priority focus for the home health agency nurse during Ms. Pimm's visits?
What should be the priority focus for the home health agency nurse during Ms. Pimm's visits?
What common misconception about pressure injuries might Ms. Pimm hold?
What common misconception about pressure injuries might Ms. Pimm hold?
Which statement best reflects Ms. Pimm's current health risk profile?
Which statement best reflects Ms. Pimm's current health risk profile?
Given Ms. Pimm's current living situation, what is an important consideration for the nurse?
Given Ms. Pimm's current living situation, what is an important consideration for the nurse?
What is a primary benefit of maintaining or improving patient activity levels?
What is a primary benefit of maintaining or improving patient activity levels?
Which dietary components are noted to be associated with the development of pressure injuries?
Which dietary components are noted to be associated with the development of pressure injuries?
What should the nurse do if a patient's dietary intake remains inadequate after interventions?
What should the nurse do if a patient's dietary intake remains inadequate after interventions?
How can compromised dignity affect a patient who is immobile?
How can compromised dignity affect a patient who is immobile?
What is an important initial action that nurses should take regarding patient dignity?
What is an important initial action that nurses should take regarding patient dignity?
What is the recommended frequency for evaluating a treatment plan for patients who are immobile?
What is the recommended frequency for evaluating a treatment plan for patients who are immobile?
Which strategy should nurses not use to help maintain a patient's dignity?
Which strategy should nurses not use to help maintain a patient's dignity?
What approach should nurses take if they identify barriers to a patient's adequate nutrition?
What approach should nurses take if they identify barriers to a patient's adequate nutrition?
What is a possible consequence of poorly hydrated skin?
What is a possible consequence of poorly hydrated skin?
Which practice should be avoided to prevent deep tissue trauma?
Which practice should be avoided to prevent deep tissue trauma?
What should be done to minimize skin exposure to moisture?
What should be done to minimize skin exposure to moisture?
What type of injury occurs when the skin remains still while the underlying tissue shifts?
What type of injury occurs when the skin remains still while the underlying tissue shifts?
What is the recommended repositioning frequency for an at-risk patient?
What is the recommended repositioning frequency for an at-risk patient?
Which of the following devices should not be used for pressure relief?
Which of the following devices should not be used for pressure relief?
What is a key factor in maintaining skin integrity and promoting wound healing?
What is a key factor in maintaining skin integrity and promoting wound healing?
What change in patient condition should prompt immediate contact with a healthcare provider?
What change in patient condition should prompt immediate contact with a healthcare provider?
What should be avoided to reduce friction injuries?
What should be avoided to reduce friction injuries?
Which positioning strategy increases the risk of pressure injury?
Which positioning strategy increases the risk of pressure injury?
What is a suggested practice for patients who are chair-bound?
What is a suggested practice for patients who are chair-bound?
Which professional is commonly involved in care for patients at risk for pressure injuries?
Which professional is commonly involved in care for patients at risk for pressure injuries?
What main aspect should be included in patient education regarding pressure injuries?
What main aspect should be included in patient education regarding pressure injuries?
What is the role of assistive devices in patient care?
What is the role of assistive devices in patient care?
What characterizes a stage 3 pressure ulcer?
What characterizes a stage 3 pressure ulcer?
Which of the following interventions should be included when teaching Ms. Pimm about wound care?
Which of the following interventions should be included when teaching Ms. Pimm about wound care?
What is an appropriate over-the-counter medication for Ms. Pimm's postoperative and ulcer pain?
What is an appropriate over-the-counter medication for Ms. Pimm's postoperative and ulcer pain?
What should be a primary goal for Ms. Pimm in her care plan?
What should be a primary goal for Ms. Pimm in her care plan?
Which of the following is NOT a potential diagnosis for Ms. Pimm's condition?
Which of the following is NOT a potential diagnosis for Ms. Pimm's condition?
What is the purpose of a hydrocolloid dressing?
What is the purpose of a hydrocolloid dressing?
How often should Ms. Pimm's hydrocolloid dressing be changed after one month of treatment?
How often should Ms. Pimm's hydrocolloid dressing be changed after one month of treatment?
What important aspect should be included in Ms. Pimm’s diet to promote wound healing?
What important aspect should be included in Ms. Pimm’s diet to promote wound healing?
Which of the following factors is NOT listed as contributing to Ms. Pimm's impaired skin integrity?
Which of the following factors is NOT listed as contributing to Ms. Pimm's impaired skin integrity?
What should be performed to minimize the risk of pressure injuries?
What should be performed to minimize the risk of pressure injuries?
What is an advised method for cleaning Ms. Pimm's skin?
What is an advised method for cleaning Ms. Pimm's skin?
When should Ms. Pimm effectively use the soft elastic sleeve-type brace?
When should Ms. Pimm effectively use the soft elastic sleeve-type brace?
How is the nurse's frequency of visits to Ms. Pimm adjusted during her recovery?
How is the nurse's frequency of visits to Ms. Pimm adjusted during her recovery?
What should be monitored to identify the development of infection in Ms. Pimm's wound?
What should be monitored to identify the development of infection in Ms. Pimm's wound?
Study Notes
Patient Case Study
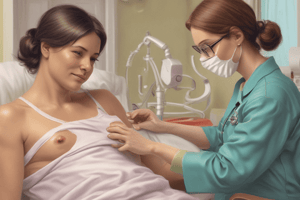
- Agnes Pimm, 74 years old, underwent knee replacement surgery and developed a stage 3 pressure ulcer on her leg due to supportive knee brace irritation.
- Ms. Pimm is independent, lives at home, and has a history of hypertension, smoking, and grief after her husband's death.
- She has a low protein and high sodium diet, struggles with appetite, and has difficulty accessing fresh foods.
- The wound is clean, without necrotic tissue, and exhibits no signs of inflammation or infection.
- Nurse Jessi Fletcher has been assigned to Ms. Pimm's care and assesses the patient's skin integrity.
- Nursing diagnoses include: Potential for infection related to pressure injury, Impaired skin integrity, Acute pain, Undernutrition, and Grieving.
- Ms. Pimm's care plan focuses on wound healing, infection prevention, nutrition, pain management, and smoking cessation.
- The care plan implementation includes teaching Ms. Pimm about medication administration, wound care, and infection prevention, as well as demonstrating the proper method for cleaning and dressing the pressure injury.
- Ms. Pimm is referred to a dietitian to create a wound healing meal plan suitable for her hypertension.
- Ms. Pimm struggles with her diet but shows an understanding of healthy eating and makes an effort to follow the dietitian's meal plan.
- Ms. Pimm struggles with smoking cessation despite trying various methods. She is referred to community resources for smoking cessation support.
- The nurse provides home health visits and the wound improves to stage 2 after a month of treatment.
- Over time, Ms. Pimm takes over wound care responsibilities and the frequency of home visits is reduced to three times a week.
Interventions for Patients at Risk for Impaired Skin Integrity
- Regular skin inspection: At least once a day, paying attention to bony prominences.
- Skin cleansing: Clean the skin when soiled and at routine intervals, using mild cleansing agents and gentle techniques.
- Minimize environmental factors: Avoid hot water, low humidity, and exposure to cold. Use moisturizers to treat dry skin.
- Avoid massage: Avoid massaging over bony prominences to minimize deep tissue trauma.
- Moisture management: Minimize skin exposure to moisture caused by incontinence, perspiration, or wound drainage. Use absorbent underpads and briefs, and change them frequently. Avoid placing plastic directly against the skin.
- Positioning and turning: Use proper positioning, transferring, and turning techniques to reduce friction and shear injuries.
- Pressure relief: Reposition the at-risk patient a minimum of every 2 hours using a written schedule.
- Positioning devices: Use pillows or foam wedges to protect bony prominences.
- Head of bed elevation: Maintain the head of the bed at the lowest degree of elevation consistent with the patient's medical condition.
- Assistive devices: Use assistive devices, such as a trapeze or drawsheet, to move patients who can't assist during transfers and position changes.
- Pressure-reducing devices: Use pressure-reducing devices for chair-bound patients.
- Written plan: Create a written plan for positioning, movement, and the use of positioning devices.
- Collaboration: Collaborate with physical therapists, primary caregivers, and other healthcare professionals.
- Patient and caregiver teaching: Educate patients and caregivers about pressure injuries, risk factors, skin care, and prevention strategies.
- Referral: Refer patients to home health agencies or community health departments for support.
Prevent Infection of Pressure Injuries
- Maintain skin hygiene: Keep the skin clean, dry, and moisturized.
- Maintain appropriate nutrition and hydration: Ensure adequate protein and carbohydrate intake and hydration status.
- Early recognition: Recognize early stages of pressure injuries for immediate intervention.
- Contact healthcare provider: Contact the healthcare provider at the earliest appearance of a pressure injury or change in skin integrity.
- Maintain activity levels: Encourage patients to maintain or improve current activity levels.
Prevent Nutritional Imbalance
- Assess dietary intake: Assess factors related to dietary intake.
- Nutritional supplements: Offer nutritional supplements.
- Mealtime support: Support patients during mealtimes.
- Consult dietitian: Consult with a dietitian if barriers to adequate nutrition exist.
Prevent Compromised Dignity and Situational Low Self-Esteem
- Assess for abuse and neglect: Assess for indicators of abuse or neglect during healthcare interactions.
- Build a trusting relationship: Develop a trusting, caring relationship with the patient.
- Educate patients and family members: Provide essential patient and family teaching to reduce the risk of pressure injury development and promote patient dignity.
- Assist with supportive devices: Assist patients and family members with obtaining supportive devices to help maintain appropriate positioning.
Evaluation
- Monitor skin integrity, comfort, and pain level regularly.
- Evaluate and modify the treatment plan as needed, potentially daily.
- Monitor dietary intake and consult with a nutritionist or dietitian if needed.
- Inform mobile patients when to call the office if they discover a potential pressure injury or change in skin integrity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz focuses on the case study of Agnes Pimm, a 74-year-old patient with a stage 3 pressure ulcer following knee replacement surgery. It covers nursing assessments, diagnoses, care plans, and patient education to promote wound healing and overall health management. Test your understanding of effective nursing care strategies for elderly patients with complex needs.