Podcast
Questions and Answers
Cal destes factores non é considerado un factor de risco para a enfermidade?
Cal destes factores non é considerado un factor de risco para a enfermidade?
- Dolor prodrómico
- Idade superior a 60 anos
- Sexo masculino (correct)
- Rash severo e diseminado
Que tratamento é utilizado para aliviar o dolor asociado á enfermidade?
Que tratamento é utilizado para aliviar o dolor asociado á enfermidade?
- Antihistamínicos
- Antibióticos
- Anticonvulsivantes
- Opioides (correct)
Cales son as características da vacina Zostavax?
Cales son as características da vacina Zostavax?
- Vacuna de subunidades
- Vacuna recombinante
- Vacuna viva atenuada (correct)
- Vacuna inactivada
Canto tempo hai que esperar entre as dúas doses de Shingrix?
Canto tempo hai que esperar entre as dúas doses de Shingrix?
Que situación require derivación a un oftalmólogo?
Que situación require derivación a un oftalmólogo?
Cal dos seguintes factores non é un factor predispoñente para a portación de S. aureus?
Cal dos seguintes factores non é un factor predispoñente para a portación de S. aureus?
Que tratamento é apropiado para un paciente con éctima grave?
Que tratamento é apropiado para un paciente con éctima grave?
Cal é un síntoma característico do ántrax?
Cal é un síntoma característico do ántrax?
Que tipo de infección é Erisipela?
Que tipo de infección é Erisipela?
Que antibiótico non se menciona como tratamento para o ántrax?
Que antibiótico non se menciona como tratamento para o ántrax?
Cal é o tratamento máis adecuado para a foliculitis profunda?
Cal é o tratamento máis adecuado para a foliculitis profunda?
Cales son os síntomas característicos da foliculitis superficial?
Cales son os síntomas característicos da foliculitis superficial?
Cal é a principal causa do forúnculo?
Cal é a principal causa do forúnculo?
Cales son os factores predispoñentes a ter foliculitis?
Cales son os factores predispoñentes a ter foliculitis?
Que tratamento non é apropiado para a foliculitis?
Que tratamento non é apropiado para a foliculitis?
Quais son as condicións asociadas a flácidas e halo costroso?
Quais son as condicións asociadas a flácidas e halo costroso?
Que tipo de herpes está asociado a episodios recurentes?
Que tipo de herpes está asociado a episodios recurentes?
Cal é a forma ulcera do herpes que pode xurdir após unha infección?
Cal é a forma ulcera do herpes que pode xurdir após unha infección?
Cal das seguintes condicións non está mencionada como neoplásica?
Cal das seguintes condicións non está mencionada como neoplásica?
Que tipo de dor se relaciona frecuentemente co herpes post herpético?
Que tipo de dor se relaciona frecuentemente co herpes post herpético?
Que bacterias son responsables do impétigo vulgar?
Que bacterias son responsables do impétigo vulgar?
Que manifestacións son características do impétigo ampollar?
Que manifestacións son características do impétigo ampollar?
Cales son os antibióticos tópicos recomendados para o tratamento do impétigo vulgar?
Cales son os antibióticos tópicos recomendados para o tratamento do impétigo vulgar?
Que sinal clínico é característico do síndrome de pele escaldada estafilocócica (SPEE)?
Que sinal clínico é característico do síndrome de pele escaldada estafilocócica (SPEE)?
Canto tempo normalmente leva a recuperación do impétigo ampollar?
Canto tempo normalmente leva a recuperación do impétigo ampollar?
Que pacientes son máis propensos a desenvolver impétigo ampollar?
Que pacientes son máis propensos a desenvolver impétigo ampollar?
Que tratamento sistémico é eficaz para alérxicos á penicilina no tratamento do impétigo?
Que tratamento sistémico é eficaz para alérxicos á penicilina no tratamento do impétigo?
Que tipo de lesións aparecen primeiro no impétigo vulgar?
Que tipo de lesións aparecen primeiro no impétigo vulgar?
Study Notes
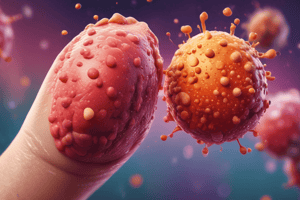
Herpes Zoster Risk Factors
- Age (50% in patients over 60 years old)
- Female sex
- Prodromal pain
- Severe pain
- Severe, widespread rash
Herpes Zoster Treatment
- General: Loose cotton clothing, maintain social activities
- Medications:
- Tricyclic antidepressants
- Gabapentin/Pregabalin
- Opioids
- Lidocaine 5% patches
- Referral to pain management specialist
Herpes Zoster Prevention and Referral
- Zostavax: Live attenuated vaccine, more concentrated than varicella vaccine (now discontinued)
- Shingrix: Recombinant zoster virus vaccine
- Can be given to immunosuppressed patients
- 2 doses separated by 2-6 months
- Referral to specialist if:
- More than 1 dermatome affected
- Hemorrhagic or necrotic lesions
- Involvement of the ophthalmic branch (refer to ophthalmologist, leave ointment)
- Widespread lesions
- Immunocompromised patient
Impetigo Vulgar
- Caused by Staphylococcus aureus and Streptococcus pyogenes
- Frequently seen in exposed areas (face), periorificial (mouth, nose)
- Clinical Presentation:
- Erythematous macule → vesicle → pustule → erosion
- Superficial crust with yellow crust (melicerica)
- Differential Diagnosis:
- Herpes simplex
- Eczema
- Insect bites
- Chickenpox
Impetigo Vulgar Treatment
- Local Management:
- Local cleansing and debridement
- Topical Antibiotics:
- Mupirocin 2% 3 times a day
- Fusidic acid 2% twice a day for 1 week, chloramphenicol
- Systemic Antibiotics:
- First-generation cephalosporins: cefadroxil (30 mg/kg/day divided every 12 hours for 10 days)
- Flucloxacillin (50 mg/kg/day divided every 8 hours)
- Penicillin allergy:
- Erythromycin (30-50 mg/kg/day divided every 6 hours)
- Azithromycin (10 mg/kg/day for 5 days)
Bullous Impetigo
-
More common in skin folds, especially in young children
-
Caused by Staphylococcus aureus
-
Clinical Presentation:
- Vesicles rapidly transform into flaccid, transparent bullae
- Sharp margins without an erythematous halo
- Halo of scales
- Bullae rupture easily, leaving a dry, shiny erosion with a thin crust
- Heals faster than impetigo vulgaris
-
Complications:
- If epidermolytic toxin spreads hematogenously, it can lead to Staphylococcal Scalded Skin Syndrome (SSSS), a generalized form of bullous impetigo
Staphylococcal Scalded Skin Syndrome (SSSS)
- Clinical Presentation:
- Patient has impaired general state: abrupt onset of irritability and fever
- Macular erythema starts on the face (periorificial) and folds
- Sensitive skin, generalized rash, Nikolsky sign (+) (skin peels off with friction)
- Wrinkled skin, 24-48 hours: flaccid bullae detach, large erosive areas with moisture that dries → thin crust, desquamation (in folds) 3-5 days
- Includes hands and feet, crusts and fissures (radiating) around the mouth
- Pathology: Necrosis of keratinocytes
SSSS Treatment
- Primary Goal: Eradicate the infectious focus
- Treatment:
- Intravenous antibiotics (cloxacillin, vancomycin if MRSA)
- Skin and electrolyte management
- Diagnosis and management of carriers (mupirocin nasal)
SSSS Differential Diagnosis
- Scarlet fever
- Kawasaki disease
- Staphylococcal toxic shock syndrome
- Toxic Epidermal Necrolysis (TEN) (due to medications)
Folliculitis
- Superficial Folliculitis:
- Involves the distal portion of the hair follicle
- Papules or pustules 1-4 mm in diameter on an erythematous base, pruritic
- Deep Folliculitis:
- Involves the deeper portion of the hair follicle
- Erythematous, tender papules of larger size with central pustules
- Can extend to surrounding tissue → furuncle
- Differential Diagnosis:
- Acne
- Pilonidal cyst
- Sycosis
Folliculitis Treatment
- Reduce Predisposing Factors:
- Hygiene
- Medications (e.g., corticosteroids)
- Local Measures:
- Washing with antibacterial soaps (triclosan or chlorhexidine 1%)
- Topical Antibiotics:
- Mupirocin 2%, fusidic acid for 7-10 days
- Oral Antibiotics:
- Flucloxacillin → for extensive, resistant, or recurrent cases
Abscess, Furuncle, Carbuncle
- Abscess: Located in any area, whereas furuncle involves hair follicle, and carbuncle is a cluster of furuncles.
- Furuncle:
- Occurs more frequently in adolescents and young adults, due to S. aureus
- More frequent in areas of friction, face, neck (nape), armpits, buttocks, thighs and perineum
- Predisposing factors: S. aureus carriage, diabetes mellitus (DM), obesity, immunosuppression, tight clothing, hyperhidrosis, poor hygiene
- Carbuncle:
- Involves subcutaneous tissue, firm swelling with openings that drain pus on the surface
- More commonly found in the nape, back, and thighs.
- Symptoms: Fever, pain
- Complications: Scarring
- More common in: Diabetics
Abscess, Furuncle, Carbuncle Treatment
- Local Management:
- Local heat and drainage
- Systemic Antibiotics:
- Cloxacillin or flucloxacillin
- First-generation cephalosporin
- Amoxicillin-clavulanate
- Penicillin allergy: macrolide or clindamycin
Ecthyma
- Clinical Presentation:
- Ulcerative form of non-bullous impetigo, involvement of epidermis and dermis
- More frequently seen on the lower extremities (dorsum of the feet and anterior legs)
- Few lesions
- Treatment:
- Mild cases: topical macrolides or clindamycin
- Severe or facial cases: IV antibiotics
- Penicillin sodium (2-4 million units every 6 hours) + cloxacillin (1 g every 6 hours) OR
- First-generation cephalosporin (cefazolin 1-2 g every 8 hours) OR
- If responds well after 72 hours: cefadroxil (1 g every 12 hours) orally
- Penicillin allergy: lincomycin IV and then orally
- Chronic ulcer associated with Ecthyma: Cover for anaerobes and gram-
- Metronidazole + ciprofloxacin
- Recurrences:
- Benzathine penicillin (1.2 million units monthly) for 6 months or erythromycin (250 mg every 12 hours) for 3 months
Erysipelas
-
Clinical Presentation:
- Infection of the dermis and superficial lymphatic plexus (more superficial than cellulitis)
- Caused by S. pyogenes (usually group A beta-hemolytic streptococcus)
-
Risk Factors:
- Age (more common in elderly)
- Underlying medical conditions (diabetes, alcoholism, malnutrition)
- Impaired immune system
- Skin trauma (cuts, scratches, insect bites)
- Recent surgery or invasive procedures
- Lymphedema
-
Clinical Presentation:
- Well-demarcated, raised, erythematous plaque
- Tenderness and pain
- Edema
- Often involves the face, lower legs, and arms
-
Treatment:
- Penicillin V (250-500 mg orally four times a day)
- Patients with penicillin allergy: cephalexin (250-500 mg by mouth four times a day)
- For severe cases: intravenous penicillin or ceftriaxone
- The duration of treatment is typically 10 days.
Erysipelas Complications
- Cellulitis
- Lymphangitis
- Sepsis
- Brain abscess (rare)
Skin Infections: Summary of Organisms
- Impetigo vulgaris: Staphylococcus aureus (most common) and Streptococcus pyogenes.
- Bullous impetigo: Staphylococcus aureus.
- Ecthyma: Streptococcus pyogenes, but Staphylococcus aureus can also be involved.
- Erysipelas: Streptococcus pyogenes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Este cuestionario aborda os factores de risco, tratamento e prevención do herpes zoster, así como a identificación de síntomas e a importancia de refíos a especialistas. É fundamental entender como tratar e minimizar os riscos asociados a esta condición para mellorar a calidade de vida dos pacientes.