Podcast
Questions and Answers
What is the approximate proportion of plasma in the volume of blood?
What is the approximate proportion of plasma in the volume of blood?
- 65%
- 35%
- 45%
- 55% (correct)
How is the separation of blood cells and plasma achieved?
How is the separation of blood cells and plasma achieved?
- By diffusion
- By osmosis
- By centrifugation (correct)
- By filtration
What is the approximate proportion of total blood volume in adults based on body weight?
What is the approximate proportion of total blood volume in adults based on body weight?
- 80 mL/kg in males and 70 mL/kg in females (correct)
- 60 mL/kg in males and 50 mL/kg in females
- 70 mL/kg in males and 60 mL/kg in females
- 90 mL/kg in males and 80 mL/kg in females
What is the role of the bloodstream in maintaining core body temperature?
What is the role of the bloodstream in maintaining core body temperature?
What is the function of blood in transporting antibodies and cells of the immune system?
What is the function of blood in transporting antibodies and cells of the immune system?
How is the continuous circulation of blood achieved throughout the body?
How is the continuous circulation of blood achieved throughout the body?
Which vitamin is essential for the synthesis of factors II, VII, IX, and X?
Which vitamin is essential for the synthesis of factors II, VII, IX, and X?
What is the name of the complex of chemicals released from damaged tissue that initiates coagulation?
What is the name of the complex of chemicals released from damaged tissue that initiates coagulation?
Which pathway of blood coagulation is activated rapidly (within seconds) following tissue damage?
Which pathway of blood coagulation is activated rapidly (within seconds) following tissue damage?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What prevents platelet adhesion in healthy, undamaged blood vessels?
What prevents platelet adhesion in healthy, undamaged blood vessels?
What is the substance that converts plasminogen to plasmin during thrombolysis?
What is the substance that converts plasminogen to plasmin during thrombolysis?
Which factor is responsible for stabilizing fibrin during blood clotting?
Which factor is responsible for stabilizing fibrin during blood clotting?
Antihaemophilic globulin (AHG) is also known as:
Antihaemophilic globulin (AHG) is also known as:
Which type of leukocyte is responsible for producing interleukin 1 and enhancing T-lymphocyte production?
Which type of leukocyte is responsible for producing interleukin 1 and enhancing T-lymphocyte production?
What is the function of basophils in allergic reactions?
What is the function of basophils in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What is the function of platelets in hemostasis?
What is the function of platelets in hemostasis?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is the main function of the mononuclear phagocyte system?
What is the main function of the mononuclear phagocyte system?
What initiates the formation of prothrombin activator in coagulation?
What initiates the formation of prothrombin activator in coagulation?
Where are platelets mainly stored for emergency use?
Where are platelets mainly stored for emergency use?
What do eosinophils release in allergic inflammations?
What do eosinophils release in allergic inflammations?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What is the function of mast cells upon allergen contact?
What is the function of mast cells upon allergen contact?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
What is the primary stimulus for increased erythropoiesis?
What is the primary stimulus for increased erythropoiesis?
Which organ is responsible for producing erythropoietin?
Which organ is responsible for producing erythropoietin?
What type of leukocyte is specialized for the elimination of parasites?
What type of leukocyte is specialized for the elimination of parasites?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
What is the primary oxygen-carrying molecule in red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
Which leukocyte type is the most abundant and contains nuclei?
Which leukocyte type is the most abundant and contains nuclei?
What is produced by erythrocyte breakdown and is used to form new haemoglobin molecules?
What is produced by erythrocyte breakdown and is used to form new haemoglobin molecules?
What type of leukocyte accounts for about 40-75% of all leukocytes?
What type of leukocyte accounts for about 40-75% of all leukocytes?
Which blood cell type has a biconcave shape and a lifespan of approximately 120 days?
Which blood cell type has a biconcave shape and a lifespan of approximately 120 days?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What type of leukocyte is involved in detecting and destroying foreign or abnormal material?
What type of leukocyte is involved in detecting and destroying foreign or abnormal material?
Which component accounts for approximately 55% of the volume of blood?
Which component accounts for approximately 55% of the volume of blood?
What is the primary function of erythrocytes (red blood cells)?
What is the primary function of erythrocytes (red blood cells)?
Which type of blood cell is responsible for blood clotting?
Which type of blood cell is responsible for blood clotting?
What is the main function of albumins in plasma?
What is the main function of albumins in plasma?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What is the function of globulins in plasma?
What is the function of globulins in plasma?
What is the characteristic shape of erythrocytes (red blood cells) suited for?
What is the characteristic shape of erythrocytes (red blood cells) suited for?
What are the main sites of haemopoiesis in adults?
What are the main sites of haemopoiesis in adults?
Which type of blood cell plays a role in the body's immune response?
Which type of blood cell plays a role in the body's immune response?
What is the main function of plasma proteins?
What is the main function of plasma proteins?
What is the approximate proportion of plasma in the volume of blood?
What is the approximate proportion of plasma in the volume of blood?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is the primary oxygen-carrying molecule in red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
Where are platelets mainly stored for emergency use?
Where are platelets mainly stored for emergency use?
Which blood cell type has a biconcave shape and a lifespan of approximately 120 days?
Which blood cell type has a biconcave shape and a lifespan of approximately 120 days?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the primary stimulus for increased erythropoiesis?
What is the primary stimulus for increased erythropoiesis?
What is the primary oxygen-carrying molecule in red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What is the approximate proportion of total blood volume in adults based on body weight?
What is the approximate proportion of total blood volume in adults based on body weight?
Which type of leukocyte is involved in detecting and destroying foreign or abnormal material?
Which type of leukocyte is involved in detecting and destroying foreign or abnormal material?
What is primarily responsible for transporting oxygen to the body's tissues?
What is primarily responsible for transporting oxygen to the body's tissues?
How is the continuous circulation of blood achieved throughout the body?
How is the continuous circulation of blood achieved throughout the body?
What is the primary role of vitamin K in blood clotting?
What is the primary role of vitamin K in blood clotting?
What is the primary function of the extrinsic pathway in blood coagulation?
What is the primary function of the extrinsic pathway in blood coagulation?
Which process involves the breakdown of fibrin and is essential for removing a blood clot?
Which process involves the breakdown of fibrin and is essential for removing a blood clot?
What is the primary role of heparin and antithrombin III in blood clotting?
What is the primary role of heparin and antithrombin III in blood clotting?
What is the main function of plasmin in the process of thrombolysis?
What is the main function of plasmin in the process of thrombolysis?
How are activated clotting factors cleared from the blood during blood clotting?
How are activated clotting factors cleared from the blood during blood clotting?
Which blood component is responsible for transporting oxygen to the body's tissues?
Which blood component is responsible for transporting oxygen to the body's tissues?
What is the primary function of thrombolysis in blood clot removal?
What is the primary function of thrombolysis in blood clot removal?
'What stimulates its own production and requires control mechanisms to limit clotting?'
'What stimulates its own production and requires control mechanisms to limit clotting?'
What is primarily responsible for activating the intrinsic pathway of blood clotting?
What is primarily responsible for activating the intrinsic pathway of blood clotting?
What is the primary function of mast cells in allergic reactions?
What is the primary function of mast cells in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What initiates the formation of prothrombin activator in coagulation?
What initiates the formation of prothrombin activator in coagulation?
What is the primary function of the mononuclear phagocyte system?
What is the primary function of the mononuclear phagocyte system?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is the function of globulins in plasma?
What is the function of globulins in plasma?
What is primarily responsible for transporting oxygen to the body's tissues?
What is primarily responsible for transporting oxygen to the body's tissues?
What is the primary function of albumins in plasma?
What is the primary function of albumins in plasma?
Where does the process of blood cell formation primarily occur?
Where does the process of blood cell formation primarily occur?
What is the primary stimulus for increased erythropoiesis?
What is the primary stimulus for increased erythropoiesis?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What is the approximate proportion of total blood volume in adults based on body weight?
What is the approximate proportion of total blood volume in adults based on body weight?
What type of leukocyte is specialized for the elimination of parasites?
What type of leukocyte is specialized for the elimination of parasites?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
What is the main function of globulins in plasma?
What is the main function of globulins in plasma?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
What prevents platelet adhesion in healthy, undamaged blood vessels?
What prevents platelet adhesion in healthy, undamaged blood vessels?
What is the approximate proportion of plasma in the volume of blood?
What is the approximate proportion of plasma in the volume of blood?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the characteristic shape of erythrocytes (red blood cells) suited for?
What is the characteristic shape of erythrocytes (red blood cells) suited for?
What is the primary oxygen-carrying molecule in red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is the main function of albumins in plasma?
What is the main function of albumins in plasma?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is primarily responsible for transporting oxygen to the body's tissues?
What is primarily responsible for transporting oxygen to the body's tissues?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type is responsible for promoting tissue inflammation through toxic chemicals?
Which leukocyte type is responsible for promoting tissue inflammation through toxic chemicals?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
Which cell type is responsible for forming a platelet plug to stop bleeding?
Which cell type is responsible for forming a platelet plug to stop bleeding?
Which type of blood cell is produced from megakaryocytes and plays a key role in blood clotting and haemostasis?
Which type of blood cell is produced from megakaryocytes and plays a key role in blood clotting and haemostasis?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
Which leukocyte type is granulated, fixed in tissues, and degranulates faster than basophils?
Which leukocyte type is granulated, fixed in tissues, and degranulates faster than basophils?
Which leukocyte type makes up 25-50% of the total leukocyte count and has large nuclei and no cytoplasmic granules?
Which leukocyte type makes up 25-50% of the total leukocyte count and has large nuclei and no cytoplasmic granules?
Which leukocyte type develops into macrophages and produces interleukin 1?
Which leukocyte type develops into macrophages and produces interleukin 1?
Where does coagulation occur through the extrinsic and intrinsic pathways?
Where does coagulation occur through the extrinsic and intrinsic pathways?
What is the primary role of basophils in allergic reactions?
What is the primary role of basophils in allergic reactions?
Which cell type is responsible for synthesizing and releasing cytokines in the body?
Which cell type is responsible for synthesizing and releasing cytokines in the body?
Which blood cell type develops from pluripotent stem cells into T-lymphocytes and B-lymphocytes?
Which blood cell type develops from pluripotent stem cells into T-lymphocytes and B-lymphocytes?
Which plasma protein is responsible for transporting hormones and mineral salts, and inhibiting some proteolytic enzymes?
Which plasma protein is responsible for transporting hormones and mineral salts, and inhibiting some proteolytic enzymes?
What primarily maintains the normal plasma volume in the body?
What primarily maintains the normal plasma volume in the body?
Where does the process of blood cell formation primarily occur?
Where does the process of blood cell formation primarily occur?
What is primarily responsible for transporting oxygen to the body's tissues?
What is primarily responsible for transporting oxygen to the body's tissues?
What is the main function of clotting factors in plasma?
What is the main function of clotting factors in plasma?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What is the primary function of erythrocytes in the blood?
What is the primary function of erythrocytes in the blood?
What is primarily responsible for maintaining the normal plasma volume in the body?
What is primarily responsible for maintaining the normal plasma volume in the body?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is primarily responsible for converting biliverdin into bilirubin before being excreted in bile?
What is responsible for transporting oxygen in the blood bound to haemoglobin in red blood cells?
What is responsible for transporting oxygen in the blood bound to haemoglobin in red blood cells?
What is the primary site of haemopoiesis in adults?
What is the primary site of haemopoiesis in adults?
What is mainly responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
What is mainly responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
Which vitamin is essential for the synthesis of factors II, VII, IX, and X in the blood clotting process?
Which vitamin is essential for the synthesis of factors II, VII, IX, and X in the blood clotting process?
What is the primary function of tissue factor (thromboplastin) in the blood clotting process?
What is the primary function of tissue factor (thromboplastin) in the blood clotting process?
What is responsible for converting plasminogen to plasmin during thrombolysis in the blood clot removal process?
What is responsible for converting plasminogen to plasmin during thrombolysis in the blood clot removal process?
What is the approximate time duration for the intrinsic pathway to be triggered after blood comes into contact with damaged blood vessel lining?
What is the approximate time duration for the intrinsic pathway to be triggered after blood comes into contact with damaged blood vessel lining?
Which factor is a powerful stimulator of its own production in the process of blood clotting?
Which factor is a powerful stimulator of its own production in the process of blood clotting?
What controls and limits clotting to the affected area and terminates the process at the appropriate time in the blood clotting process?
What controls and limits clotting to the affected area and terminates the process at the appropriate time in the blood clotting process?
What prevents platelet adhesion in healthy, undamaged blood vessels in the blood clotting process?
What prevents platelet adhesion in healthy, undamaged blood vessels in the blood clotting process?
What is primarily responsible for removing the formed clot and healing the damaged blood vessel in the blood clotting process?
What is primarily responsible for removing the formed clot and healing the damaged blood vessel in the blood clotting process?
What is rapidly cleared from the blood by the liver during the blood clotting process?
What is rapidly cleared from the blood by the liver during the blood clotting process?
Which complex of chemicals released from damaged tissue initiates coagulation in the blood clotting process?
Which complex of chemicals released from damaged tissue initiates coagulation in the blood clotting process?
Which factor is primarily responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
Which factor is primarily responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
What primarily maintains the normal plasma volume in the body?
What primarily maintains the normal plasma volume in the body?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
Which leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What is the approximate proportion of plasma in the volume of blood?
What is the approximate proportion of plasma in the volume of blood?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What primarily maintains the normal plasma volume in the body?
What primarily maintains the normal plasma volume in the body?
What is responsible for converting plasminogen to plasmin during thrombolysis in the blood clot removal process?
What is responsible for converting plasminogen to plasmin during thrombolysis in the blood clot removal process?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
What primarily maintains the normal plasma volume in the body?
What primarily maintains the normal plasma volume in the body?
What is responsible for transporting oxygen to the body's tissues?
What is responsible for transporting oxygen to the body's tissues?
Which process involves the breakdown of fibrin and is essential for removing a blood clot?
Which process involves the breakdown of fibrin and is essential for removing a blood clot?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
What is responsible for the breakdown of erythrocytes (haemolysis) in the body?
Which type of leukocyte accounts for about 40-75% of all leukocytes?
Which type of leukocyte accounts for about 40-75% of all leukocytes?
Which plasma protein maintains osmotic pressure and acts as a carrier for substances like free fatty acids, drugs, and steroid hormones?
Which plasma protein maintains osmotic pressure and acts as a carrier for substances like free fatty acids, drugs, and steroid hormones?
Where does haemopoiesis occur primarily in adults?
Where does haemopoiesis occur primarily in adults?
What is the lifespan of erythrocytes (red blood cells)?
What is the lifespan of erythrocytes (red blood cells)?
What is the primary function of platelets in the blood?
What is the primary function of platelets in the blood?
Which type of blood cell is responsible for transporting oxygen and some carbon dioxide throughout the body?
Which type of blood cell is responsible for transporting oxygen and some carbon dioxide throughout the body?
What maintains normal plasma volume in the body and carries various substances including proteins, electrolytes, nutrients, waste products, hormones, and gases?
What maintains normal plasma volume in the body and carries various substances including proteins, electrolytes, nutrients, waste products, hormones, and gases?
What is primarily responsible for maintaining blood pH between 7.35 and 7.45?
What is primarily responsible for maintaining blood pH between 7.35 and 7.45?
What is the primary function of plasma proteins?
What is the primary function of plasma proteins?
Which hormone primarily regulates red blood cell production and is mainly stimulated by hypoxia?
Which hormone primarily regulates red blood cell production and is mainly stimulated by hypoxia?
What is the primary site of erythropoietin production in the body?
What is the primary site of erythropoietin production in the body?
What is the approximate normal leukocyte count in adult blood?
What is the approximate normal leukocyte count in adult blood?
Which leukocyte type is involved in promoting tissue inflammation through release of toxic chemicals?
Which leukocyte type is involved in promoting tissue inflammation through release of toxic chemicals?
What is primarily responsible for processing and excreting bilirubin, a byproduct of the destruction of red blood cells?
What is primarily responsible for processing and excreting bilirubin, a byproduct of the destruction of red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
What is the primary oxygen-carrying molecule in red blood cells?
What leukocyte type is primarily responsible for protecting the body against bacterial invasion?
What leukocyte type is primarily responsible for protecting the body against bacterial invasion?
What causes vasoconstriction during hemostasis?
What causes vasoconstriction during hemostasis?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
What leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What leukocyte type contains anticoagulant heparin and inflammatory agent histamine?
What leukocyte type is granulated, fixed in tissues, and degranulates faster than basophils?
What leukocyte type is granulated, fixed in tissues, and degranulates faster than basophils?
What is the primary role of vitamin K in blood clotting?
What is the primary role of vitamin K in blood clotting?
Which blood component is responsible for transporting oxygen to the body's tissues?
Which blood component is responsible for transporting oxygen to the body's tissues?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
What is the enzyme that breaks down fibrin during the process of thrombolysis?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
Which process involves the formation of insoluble threads of fibrin to form a blood clot?
What is mainly responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
What is mainly responsible for maintaining blood pH between 7.35 and 7.45 through a buffering system?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
Which leukocyte type releases toxic chemicals promoting inflammation in allergic reactions?
What initiates hemostasis following blood vessel damage?
What initiates hemostasis following blood vessel damage?
What is the approximate proportion of total blood volume in adults based on body weight?
What is the approximate proportion of total blood volume in adults based on body weight?
Where does haemopoiesis occur in adults?
Where does haemopoiesis occur in adults?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
Which cell type, similar to basophils, contains cytoplasmic granules with heparin, histamine, and other inflammatory substances?
Flashcards are hidden until you start studying
Study Notes
-
Haemopoiesis is the process by which all blood cells originate in the bone marrow.
-
Plasma is the main constituent of blood, accounting for 55% of its volume, and is primarily water carrying various dissolved and suspended substances.
-
Plasma proteins, including albumin and fibrinogen, make up about 7% of plasma and are responsible for maintaining normal plasma osmotic pressure and creating its viscosity.
-
Albumins are the most abundant plasma proteins, maintaining osmotic pressure, and serving as carrier molecules for nutrients, drugs, and hormones.
-
Globulins, which make up about 20% of plasma proteins, function as antibodies, transport hormones and mineral salts, and inhibit some proteolytic enzymes.
-
Clotting factors are responsible for coagulation of blood and are present in plasma, with fibrinogen being the most abundant.
-
Electrolytes, such as calcium, potassium, and sodium, have various functions, including muscle contraction, nerve impulse transmission, and maintaining acid-base balance.
-
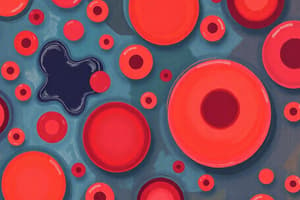
Red blood cells, also known as erythrocytes, are the most abundant type of blood cells, making up around 99% of all blood cells, and their primary function is to transport oxygen and some carbon dioxide.
-
There are three main types of blood cells: erythrocytes (red cells), leukocytes (white cells), and thrombocytes (platelets).
-
Erythrocytes are biconcave discs with no nucleus, and their diameter is about 7 µm. They have a lifespan of approximately 120 days, and there are around 30 trillion in the human body.
-
Leukocytes, or white blood cells, play a role in the body's immune response and are produced in both red bone marrow and lymphoid tissue.
-
Platelets, or thrombocytes, are responsible for blood clotting.
-
In the first few years of life, red marrow completely fills the space within bones, but over the next 20 years, it is largely replaced by fatty yellow marrow, which has no haemopoietic function.
-
In adults, haemopoiesis occurs in flat bones, irregular bones, and the ends of long bones, with the main sites being the sternum, ribs, pelvis, and skull.
-
Different types of blood cells follow separate lines of development and go through several stages before entering the bloodstream.
-
The process of blood cell formation is called haemopoiesis.
-
Oxygen, which is not very soluble in water, is transported in the blood bound to haemoglobin in red blood cells.
-
Red blood cells' characteristic shape, which is suited to their purpose, increases their surface area for gas exchange and allows for fast entry and exit of gases in narrow capillaries.
-
The cellular content of blood includes red blood cells, white blood cells, and platelets.
-
The lifespan and function of erythrocytes involve the transportation of oxygen and some carbon dioxide for approximately 120 days.
-
Haemopoiesis is the process through which blood cells develop, with all blood cells originating from pluripotent stem cells in the bone marrow.
-
Plasma, the liquid component of blood, is mainly water (90-92%) carrying various dissolved and suspended substances, including proteins, electrolytes, nutrients, waste products, hormones, and gases.
-
Plasma proteins, which make up about 7% of plasma, are responsible for maintaining normal plasma volume in the body. They include albumins, globulins, and clotting factors.
-
Albumins, the most abundant plasma proteins, maintain osmotic pressure and act as carrier molecules for substances like free fatty acids, drugs, and steroid hormones.
-
Globulins, which include immunoglobulins (antibodies), transport hormones and mineral salts, and inhibit some proteolytic enzymes.
-
Clotting factors are responsible for coagulation of blood and are present in plasma.
-
Electrolytes, including calcium, potassium, and sodium, play important roles in muscle contraction, nerve impulse transmission, and acid-base balance.
-
Blood pH is maintained between 7.35 and 7.45 by an ongoing buffering system.
-
Nutrients, such as glucose, amino acids, and vitamins, are transported in the bloodstream for immediate use or storage by cells in the body.
-
Waste products, including urea, creatinine, uric acid, and carbon dioxide, are carried in the blood to the kidneys or lungs for excretion.
-
Hormones, which are produced by endocrine glands, are secreted into the blood and transported to target tissues for various physiological functions.
-
Oxygen, which is not very soluble in water, is transported in the blood bound to haemoglobin in red blood cells.
-
The process of blood cell formation is called haemopoiesis and occurs primarily in red bone marrow, with the majority of blood cells being erythrocytes (red blood cells).
-
Erythrocytes, which are biconcave discs with no nucleus, have a diameter of about 7 µm and are primarily responsible for transporting oxygen and some carbon dioxide throughout the body.
-
Most lymphocytes, in addition to red bone marrow, are produced in lymphoid tissue.
-
Platelets, which are responsible for blood clotting, are also present in the blood.
-
Erythrocytes have a lifespan of about 120 days and are replaced by new cells produced in the bone marrow.
-
Red bone marrow produces all blood cells, but over time, it is replaced by fatty yellow marrow, which has no haemopoietic function.
-
Haemopoiesis in adults is primarily confined to flat bones, irregular bones, and the ends of long bones.
-
Red blood cells contain no intracellular organelles, providing maximum space for haemoglobin.
-
Erythrocytes are flexible and can squeeze through narrow capillaries.
-
The cellular content of blood includes red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes), with erythrocytes being the most abundant type.
-
Erythropoiesis is the process of erythrocyte (red blood cell) development from stem cells, taking approximately 7 days.
-
Erythrocytes lose their nuclei as they mature and become incapable of division.
-
Red blood cells are shaped as biconcave disks and have a lifespan of about 120 days.
-
Oxygen binds reversibly to haemoglobin to form oxyhaemoglobin and changes the color of the blood.
-
Oxyhaemoglobin releases oxygen in response to low pH, low oxygen levels, or increased temperature.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism, while erythropoietin is the hormone responsible for red blood cell production.
-
Erythrocytes are destroyed by macrophages in the spleen, bone marrow, and liver.
-
Iron is released during the destruction of erythrocytes and is used to form new haemoglobin molecules, and biliverdin is converted into bilirubin before being excreted in bile.
-
Leukocytes (white blood cells) are responsible for defence and immunity, and they detect and destroy foreign or abnormal material.
-
Leukocytes are the largest blood cells and contain nuclei, with granulocytes and agranulocytes being the two main types.
-
Neutrophils are the most abundant type of granulocytes, being responsible for protecting the body against bacterial invasion and removing debris, and are highly mobile.
-
Eosinophils are less active in phagocytosis but are specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Normal leukocyte counts in adult blood consist of 5-9 x 10^7/L, with granulocytes accounting for 40-75% and agranulocytes accounting for 20-50%, with monocytes and lymphocytes being the most common agranulocytes.
-
Erythrocytes remain fairly constant in number due to the bone marrow producing them at the rate of destruction, with the primary stimulus for increased erythropoiesis being hypoxia.
-
Erythrocytes have a lifespan of about 120 days, and their breakdown, or haemolysis, is carried out by macrophages in the spleen, bone marrow, and liver.
-
Haemolysis releases iron, which is returned to the bone marrow to form new haemoglobin molecules, and biliverdin is converted to bilirubin before being excreted in bile.
-
The liver converts bilirubin from a fat-soluble to a water-soluble form to be excreted in bile.
-
The kidney produces erythropoietin, which regulates red blood cell production and is primarily stimulated by hypoxia.
-
Granulocytes are the largest and most abundant type of leukocytes, with neutrophils being the most common type, making up 40-75% of all leukocytes.
-
Neutrophils are the first line of defense against bacterial invasion, being attracted to the site of infection by chemotaxins and engulfing and killing bacteria by phagocytosis.
-
Eosinophils are specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Eosinophils take up alkaline methylene blue when stained in the laboratory, and their name comes from the red acid dye, eosin, which they take up.
-
Neutrophils take up both dyes, eosin and methylene blue, and are purple in color.
-
Neutrophils have complex, multilobed nuclei and lysosomes containing enzymes in their granules for digesting engulfed material.
-
Neutrophils live for 6-9 hours in the bloodstream.
-
Granulocytes are the largest blood cells, accounting for about 1% of the blood volume.
-
Leukocytosis, or rising white cell numbers in the bloodstream, can indicate a physiological problem, such as infection, trauma, or malignancy.
-
Leukocytes are important for defence and immunity and are involved in detecting and destroying foreign or abnormal material.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism and is primarily stimulated by hypoxia.
-
Erythrocytes are responsible for transporting oxygen to the body's tissues, and their oxygen-carrying capacity is affected by factors such as pH and oxygen levels.
-
Erythrocytes undergo haemolysis, or destruction, by macrophages in the spleen, bone marrow, and liver, and the iron and biliverdin released during this process are recycled for new haemoglobin and bilirubin production.
-
Erythropoietin is the hormone that regulates red blood cell production and is primarily produced by the kidney in response to hypoxia.
-
Leukocytes are the most abundant type of blood cells and are involved in defence and immunity, detecting and destroying foreign or abnormal material.
-
Erythrocytes are the most abundant type of blood cells and are responsible for transporting oxygen to the body's tissues.
-
The red blood cell has a biconcave shape, with a lifespan of approximately 120 days, and undergoes haemolysis in the spleen, bone marrow, and liver.
-
Haemoglobin is the primary oxygen-carrying molecule in red blood cells, and its affinity for oxygen is influenced by factors such as pH, temperature, and oxygen concentration.
-
Oxyhaemoglobin releases oxygen in response to low pH, low oxygen levels, or increased temperature.
-
The liver is responsible for processing and excreting bilirubin, which is a byproduct of the destruction of red blood cells.
-
Erythropoietin is the hormone that regulates red blood cell production, and its production is primarily stimulated by hypoxia.
-
The kidney is the primary site of erythropoietin production.
-
Granulocytes are the largest type of leukocytes and are involved in defence and immunity by detecting and destroying foreign or abnormal material.
-
Neutrophils are the most common type of granulocyte and are responsible for protecting the body against bacterial invasion.
-
Eosinophils are a type of granulocyte that is specialized for the elimination of parasites.
-
Leukocytes are the largest blood cells and are involved in defence and immunity, making up about 1% of the blood volume.
-
Erythropoiesis is the process by which red blood cells are produced from stem cells, taking approximately 7 days, and involves the loss of the nucleus and the development of a biconcave shape.
-
Oxygen binds reversibly to haemoglobin to form oxyhaemoglobin and changes the color of the blood.
-
Erythrocytes have a lifespan of about 120 days and undergo haemolysis, or destruction, in the spleen, bone marrow, and liver.
-
Haemoglobin plays a crucial role in the transport of oxygen to the body's tissues and is influenced by factors such as pH, temperature, and oxygen concentration.
-
Eosinophils are a type of granulocyte that is specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Erythrocytes are the most abundant type of blood cells, responsible for transporting oxygen to the body's tissues and making up about 40-45% of the blood volume.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism, with erythropoietin being the primary hormone responsible for red blood cell production.
-
Erythrocytes are destroyed by macrophages in the spleen, bone marrow, and liver, and the iron and biliverdin released during this process are recycled for new haemoglobin and bilirubin production.
-
Neutrophils are the most abundant type of leukocytes and are responsible for protecting the body against bacterial invasion, making up about 40-75% of all leukocytes.
-
Neutrophils are the most common type of granulocyte, accounting for about 40-75% of all leuk
-
Haemopoiesis is the process through which blood cells develop, with all blood cells originating from pluripotent stem cells in the bone marrow.
-
Plasma, the liquid component of blood, is mainly water (90-92%) carrying various dissolved and suspended substances, including proteins, electrolytes, nutrients, waste products, hormones, and gases.
-
Plasma proteins, which make up about 7% of plasma, are responsible for maintaining normal plasma volume in the body. They include albumins, globulins, and clotting factors.
-
Albumins, the most abundant plasma proteins, maintain osmotic pressure and act as carrier molecules for substances like free fatty acids, drugs, and steroid hormones.
-
Globulins, which include immunoglobulins (antibodies), transport hormones and mineral salts, and inhibit some proteolytic enzymes.
-
Clotting factors are responsible for coagulation of blood and are present in plasma.
-
Electrolytes, including calcium, potassium, and sodium, play important roles in muscle contraction, nerve impulse transmission, and acid-base balance.
-
Blood pH is maintained between 7.35 and 7.45 by an ongoing buffering system.
-
Nutrients, such as glucose, amino acids, and vitamins, are transported in the bloodstream for immediate use or storage by cells in the body.
-
Waste products, including urea, creatinine, uric acid, and carbon dioxide, are carried in the blood to the kidneys or lungs for excretion.
-
Hormones, which are produced by endocrine glands, are secreted into the blood and transported to target tissues for various physiological functions.
-
Oxygen, which is not very soluble in water, is transported in the blood bound to haemoglobin in red blood cells.
-
The process of blood cell formation is called haemopoiesis and occurs primarily in red bone marrow, with the majority of blood cells being erythrocytes (red blood cells).
-
Erythrocytes, which are biconcave discs with no nucleus, have a diameter of about 7 µm and are primarily responsible for transporting oxygen and some carbon dioxide throughout the body.
-
Most lymphocytes, in addition to red bone marrow, are produced in lymphoid tissue.
-
Platelets, which are responsible for blood clotting, are also present in the blood.
-
Erythrocytes have a lifespan of about 120 days and are replaced by new cells produced in the bone marrow.
-
Red bone marrow produces all blood cells, but over time, it is replaced by fatty yellow marrow, which has no haemopoietic function.
-
Haemopoiesis in adults is primarily confined to flat bones, irregular bones, and the ends of long bones.
-
Red blood cells contain no intracellular organelles, providing maximum space for haemoglobin.
-
Erythrocytes are flexible and can squeeze through narrow capillaries.
-
The cellular content of blood includes red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes), with erythrocytes being the most abundant type.
-
Erythropoiesis is the process of erythrocyte (red blood cell) development from stem cells, taking approximately 7 days.
-
Erythrocytes lose their nuclei as they mature and become incapable of division.
-
Red blood cells are shaped as biconcave disks and have a lifespan of about 120 days.
-
Oxygen binds reversibly to haemoglobin to form oxyhaemoglobin and changes the color of the blood.
-
Oxyhaemoglobin releases oxygen in response to low pH, low oxygen levels, or increased temperature.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism, while erythropoietin is the hormone responsible for red blood cell production.
-
Erythrocytes are destroyed by macrophages in the spleen, bone marrow, and liver.
-
Iron is released during the destruction of erythrocytes and is used to form new haemoglobin molecules, and biliverdin is converted into bilirubin before being excreted in bile.
-
Leukocytes (white blood cells) are responsible for defence and immunity, and they detect and destroy foreign or abnormal material.
-
Leukocytes are the largest blood cells and contain nuclei, with granulocytes and agranulocytes being the two main types.
-
Neutrophils are the most abundant type of granulocytes, being responsible for protecting the body against bacterial invasion and removing debris, and are highly mobile.
-
Eosinophils are less active in phagocytosis but are specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Normal leukocyte counts in adult blood consist of 5-9 x 10^7/L, with granulocytes accounting for 40-75% and agranulocytes accounting for 20-50%, with monocytes and lymphocytes being the most common agranulocytes.
-
Erythrocytes remain fairly constant in number due to the bone marrow producing them at the rate of destruction, with the primary stimulus for increased erythropoiesis being hypoxia.
-
Erythrocytes have a lifespan of about 120 days, and their breakdown, or haemolysis, is carried out by macrophages in the spleen, bone marrow, and liver.
-
Haemolysis releases iron, which is returned to the bone marrow to form new haemoglobin molecules, and biliverdin is converted to bilirubin before being excreted in bile.
-
The liver converts bilirubin from a fat-soluble to a water-soluble form to be excreted in bile.
-
The kidney produces erythropoietin, which regulates red blood cell production and is primarily stimulated by hypoxia.
-
Granulocytes are the largest and most abundant type of leukocytes, with neutrophils being the most common type, making up 40-75% of all leukocytes.
-
Neutrophils are the first line of defense against bacterial invasion, being attracted to the site of infection by chemotaxins and engulfing and killing bacteria by phagocytosis.
-
Eosinophils are specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Eosinophils take up alkaline methylene blue when stained in the laboratory, and their name comes from the red acid dye, eosin, which they take up.
-
Neutrophils take up both dyes, eosin and methylene blue, and are purple in color.
-
Neutrophils have complex, multilobed nuclei and lysosomes containing enzymes in their granules for digesting engulfed material.
-
Neutrophils live for 6-9 hours in the bloodstream.
-
Granulocytes are the largest blood cells, accounting for about 1% of the blood volume.
-
Leukocytosis, or rising white cell numbers in the bloodstream, can indicate a physiological problem, such as infection, trauma, or malignancy.
-
Leukocytes are important for defence and immunity and are involved in detecting and destroying foreign or abnormal material.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism and is primarily stimulated by hypoxia.
-
Erythrocytes are responsible for transporting oxygen to the body's tissues, and their oxygen-carrying capacity is affected by factors such as pH and oxygen levels.
-
Erythrocytes undergo haemolysis, or destruction, by macrophages in the spleen, bone marrow, and liver, and the iron and biliverdin released during this process are recycled for new haemoglobin and bilirubin production.
-
Erythropoietin is the hormone that regulates red blood cell production and is primarily produced by the kidney in response to hypoxia.
-
Leukocytes are the most abundant type of blood cells and are involved in defence and immunity, detecting and destroying foreign or abnormal material.
-
Erythrocytes are the most abundant type of blood cells and are responsible for transporting oxygen to the body's tissues.
-
The red blood cell has a biconcave shape, with a lifespan of approximately 120 days, and undergoes haemolysis in the spleen, bone marrow, and liver.
-
Haemoglobin is the primary oxygen-carrying molecule in red blood cells, and its affinity for oxygen is influenced by factors such as pH, temperature, and oxygen concentration.
-
Oxyhaemoglobin releases oxygen in response to low pH, low oxygen levels, or increased temperature.
-
The liver is responsible for processing and excreting bilirubin, which is a byproduct of the destruction of red blood cells.
-
Erythropoietin is the hormone that regulates red blood cell production, and its production is primarily stimulated by hypoxia.
-
The kidney is the primary site of erythropoietin production.
-
Granulocytes are the largest type of leukocytes and are involved in defence and immunity by detecting and destroying foreign or abnormal material.
-
Neutrophils are the most common type of granulocyte and are responsible for protecting the body against bacterial invasion.
-
Eosinophils are a type of granulocyte that is specialized for the elimination of parasites.
-
Leukocytes are the largest blood cells and are involved in defence and immunity, making up about 1% of the blood volume.
-
Erythropoiesis is the process by which red blood cells are produced from stem cells, taking approximately 7 days, and involves the loss of the nucleus and the development of a biconcave shape.
-
Oxygen binds reversibly to haemoglobin to form oxyhaemoglobin and changes the color of the blood.
-
Erythrocytes have a lifespan of about 120 days and undergo haemolysis, or destruction, in the spleen, bone marrow, and liver.
-
Haemoglobin plays a crucial role in the transport of oxygen to the body's tissues and is influenced by factors such as pH, temperature, and oxygen concentration.
-
Eosinophils are a type of granulocyte that is specialized for the elimination of parasites, releasing toxic chemicals when they bind to infecting organisms.
-
Erythrocytes are the most abundant type of blood cells, responsible for transporting oxygen to the body's tissues and making up about 40-45% of the blood volume.
-
Erythropoiesis is regulated by a homeostatic negative feedback mechanism, with erythropoietin being the primary hormone responsible for red blood cell production.
-
Erythrocytes are destroyed by macrophages in the spleen, bone marrow, and liver, and the iron and biliverdin released during this process are recycled for new haemoglobin and bilirubin production.
-
Neutrophils are the most abundant type of leukocytes and are responsible for protecting the body against bacterial invasion, making up about 40-75% of all leukocytes.
-
Neutrophils are the most common type of granulocyte, accounting for about 40-75% of all leuk
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.