Podcast
Questions and Answers
Which type of connective tissue is characterized by fibers arranged in a parallel manner, providing strength primarily in one direction?
Which type of connective tissue is characterized by fibers arranged in a parallel manner, providing strength primarily in one direction?
- Adipose tissue
- Dense regular connective tissue (correct)
- Dense irregular connective tissue
- Loose connective tissue
Considering the functions of epithelial tissues, which of the following best describes the primary role of simple squamous epithelium?
Considering the functions of epithelial tissues, which of the following best describes the primary role of simple squamous epithelium?
- Facilitation of diffusion and filtration (correct)
- Protection against abrasion
- Absorption of nutrients
- Secretion of hormones
How does cardiac muscle tissue differ structurally from skeletal muscle tissue?
How does cardiac muscle tissue differ structurally from skeletal muscle tissue?
- Cardiac muscle has spindle-shaped, non-striated fibers.
- Skeletal muscle has branched striated fibers.
- Skeletal muscle is involuntary, whereas cardiac muscle is voluntary.
- Cardiac muscle has branched striated fibers and numerous mitochondria. (correct)
Which type of cell is responsible for releasing histamines during allergic reactions?
Which type of cell is responsible for releasing histamines during allergic reactions?
In the context of nervous tissue, what is the primary function of oligodendrocytes?
In the context of nervous tissue, what is the primary function of oligodendrocytes?
Considering the organization of the cardiovascular system, what is the role of the pulmonary circulation?
Considering the organization of the cardiovascular system, what is the role of the pulmonary circulation?
Which of the following best describes the function of the lymphatic system?
Which of the following best describes the function of the lymphatic system?
During the cardiac cycle, what event occurs during the diastole phase?
During the cardiac cycle, what event occurs during the diastole phase?
How does the atrioventricular (AV) node contribute to the cardiac cycle?
How does the atrioventricular (AV) node contribute to the cardiac cycle?
What does the QRS complex in an electrocardiogram (ECG) represent?
What does the QRS complex in an electrocardiogram (ECG) represent?
Which factor primarily determines the viscosity of blood?
Which factor primarily determines the viscosity of blood?
What is the Fahreus-Lindqvist effect?
What is the Fahreus-Lindqvist effect?
How does fibrinogen concentration affect blood rheology?
How does fibrinogen concentration affect blood rheology?
In a thermodynamic model of the cardiac cycle, what does the term 'end-diastolic volume' (EDV) refer to?
In a thermodynamic model of the cardiac cycle, what does the term 'end-diastolic volume' (EDV) refer to?
A patient with heart failure has a reduced ejection fraction. Which of the following is most likely to be observed in this patient?
A patient with heart failure has a reduced ejection fraction. Which of the following is most likely to be observed in this patient?
Flashcards
Epithelial Tissues
Epithelial Tissues
Layers of cells covering body surfaces for protection, absorption, or secretion.
Simple Epithelium
Simple Epithelium
Single layer of cells; ideal for absorption and filtration.
Stratified Epithelium
Stratified Epithelium
Multiple layers of cells, providing protection.
Squamous Cells
Squamous Cells
Signup and view all the flashcards
Cuboidal Cells
Cuboidal Cells
Signup and view all the flashcards
Connective Tissue
Connective Tissue
Signup and view all the flashcards
Adipose Tissue
Adipose Tissue
Signup and view all the flashcards
Dense Regular Tissue
Dense Regular Tissue
Signup and view all the flashcards
Red Blood Cells (Erythrocytes)
Red Blood Cells (Erythrocytes)
Signup and view all the flashcards
Platelets (Thrombocytes)
Platelets (Thrombocytes)
Signup and view all the flashcards
White Blood Cells (Leukocytes)
White Blood Cells (Leukocytes)
Signup and view all the flashcards
Skeletal Muscle
Skeletal Muscle
Signup and view all the flashcards
Smooth Muscle
Smooth Muscle
Signup and view all the flashcards
Cardiac Muscle
Cardiac Muscle
Signup and view all the flashcards
Nervous Tissue
Nervous Tissue
Signup and view all the flashcards
Study Notes
Epithelial Tissues
- Layers of cells covering body surfaces are epithelium.
- Epithelial cells cover outer skin surfaces (skin, airways).
- Endothelial cells cover inner surfaces (blood vessels).
- Cells form sheets for protection or absorption or form glands for secretion.
Epithelial Tissue Functions
- Absorption in the lining of the small intestine
- Secretion in glands
- Transport in kidney tubules
- Protection in the skin
- Sensory reception in taste buds
Epithelial Tissue Structure: Layer Arrangement
- Simple arrangement: single layer of cells for absorption and filtration
- Pseudostratified arrangement: single layer with varying cell heights
- Stratified arrangement: multiple layers of cells, providing protection
Epithelial Tissue Structure: Cell Shape
- Squamous cells are flat and allow for diffusion and filtration in areas such as lungs and blood vessels.
- Cuboidal cells are cube shaped and function in secretion and absorption, such as in kidney tubules.
- Columnar cells are tall and rectangular, specialized for secretion and absorption, found in intestines.
Pseudostratified Epithelium
- Single layer of cells where nuclei are at the basal end of the cells
- Nuclei appear at different levels because cells are tightly packed, displacing nuclei
- Cilia on the surface help move mucus and trapped particles in respiratory tract
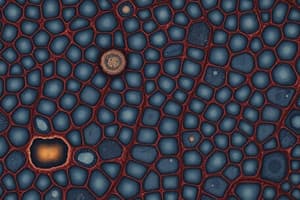
Connective Tissue
- The most abundant and widely distributed tissue characterized by low cell density and large extracellular matrix in the body
- Loose connective tissue: adipose tissue (fat storage) has loosely woven fibers that surround and cushion organs
- Dense regular connective tissue: found in ligaments and tendons with fibers arranged in parallel for strength
- Dense irregular connective tissue: found in dermis and protective capsules around organs with randomly arranged fibers for stress resistance in multiple directions
- Supportive connective tissues: Cartilage and Bone
Supportive Connective Tissue
- Cartilage: Hyaline cartilage provides support and flexibility.
- Bone: Compact bone gives structural support and mineral storage.
Fluid Connective Tissue
- Blood and lymph are involved in transporting nutrients, oxygen, and immune cells.
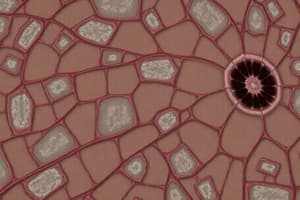
Connective Tissue: Blood
- Red blood cells (erythrocytes): transport oxygen using hemoglobin and are disc-shaped without a nucleus
- Platelets (thrombocytes): are responsible for blood clotting and are small and irregularly shaped
- White blood cells (leukocytes): play a critical role in immune response and defence
White Blood Cells (Leukocytes)
- Agranulocytes: Monocytes engulf pathogens; lymphocytes produce antibodies and destroy infected cells
- Granulocytes: Eosinophils defend against parasites and allergic reactions; basophils release histamines during allergic reactions; neutrophils are first responders to infections, engulfing bacteria
Muscle Tissue
- Skeletal muscle: voluntary, attached to bones, provides motion, heat, and protection, consists of long cylindrical fibers
- Smooth muscle: involuntary, found in walls of hollow organs and blood vessels, causes slow, rhythmical contractions, has spindle-shaped, non-striated fibers
- Cardiac muscle: involuntary, found only in the heart, contains many mitochondria, resistant to fatigue, consists of branched striated fibers
Nervous Tissue
- Responsible for sensing stimuli and transmitting signals throughout the body.
Neurons
- Dendrites: receive signals from other neurons
- Cell Body: contains the nucleus and processes information
- Axon: transmits signals to other neurons, muscles, or glands
Neuroglia
- Oligodendrocytes (CNS) and Schwann cells (PNS): surround axons and secrete myelin
- Myelin: fatty insulating sheath that wraps around axons which increases the speed of electrical impulses
Types of Neurons
- Sensory (afferent) neurons send sensory information from receptors to the central nervous system.
- Motor (efferent) neurons send information from the CNS to muscles.
- Interneurons relay signals between sensory and motor neurons within the CNS
Nervous System
- Cranial nerves: connect brain to periphery.
- Spinal nerves: connect the spinal cord to the periphery
- Tracts: connect neurons in the spinal cord and the brain
Organs and Organ Systems
- Organs are combinations of tissues that perform coordinated, complex task.
- Organs that function together are called organ systems
Major Organ Systems
- Cardiovascular
- Respiratory
- Nervous
- Skeletal
- Muscular
- Integumentary
- Endocrine
- Lymphatic
- Digestive
- Urinary
- Reproductive
Cardiovascular System
- Components: blood, heart, and blood vessels
- Functions: heart pumps blood through blood vessels; blood transports O2 and nutrients to cells, removing CO2 and waste; blood defends against disease and repairs damaged blood vessels
Urinary System
- Components: kidneys, ureters, urinary bladder, and urethra
- Functions: produces, stores, and eliminates urine to eliminate waste; regulates blood volume and chemical composition; helps maintain acid-base balance; maintains body's mineral balance; regulates red blood cell production
Lymphatic System
- Components: lymphatic fluid (lymph) and vessels, spleen, thymus, lymph nodes, and tonsils
- Functions: returns proteins and fluid to blood; carries lipids from the gastrointestinal tract; includes structures with lymphocytes that protect against disease-causing microbes and proliferate
Skeletal System
- Components: bones and joints of the body and their associated cartilages
- Functions: supports and protects the body, provides surface area for muscle attachments, aids body movement, stores minerals and lipids
Integumentary System
- Components: skin and structures associated, such as hair, nails, sweat glands, and oil glands.
- Functions: protects the body; helps regulate body temperature; eliminates some wastes; helps make vitamin D; detects sensations such as touch, pain, warmth, and cold
Anatomical Planes
- Frontal: divides the body into front and back sections
- Mid-Sagittal: divides the body into left and right sections
- Transverse: divides the body into top and bottom sections
Anatomical Directions (Absolute)
- Anterior/Posterior: front vs. back.
- Superior/Inferior: toward head vs. toward feet
- Medial/Lateral: toward midline vs. away from midline.
Anatomical Directions (Relative)
- Proximal/Distal: closer vs. further from the attachment point
- Adduction/Abduction: movement to(ad) or away (abd) from midline.
- Flexion/Extension: decreasing vs. increasing the angle of a joint
Cardiovascular Diseases
- Coronary Artery Disease: Narrowing or blockage of coronary arteries.
- Arrhythmias: Heart rhythm problems.
Functions of the Cardiovascular System
- Delivers nutrients, hormones, and signalling molecules.
- Removes metabolic waste products from tissues.
- Regulates body temperature.
Blood Circulation Facts
- Human body contains 5L of blood
- Every cell within 100 um of a blood vessel.
- This proximity allows for diffusion of CO2, O2, and small solutes.
Pulmonary and Systemic Circulation
- The right side moves deoxygenated blood to lungs.
- The left side moves oxygenated blood to the body
Circulatory Systems
- Pulmonary vessels: transport blood to and from the lungs
- Systemic vessels: transport blood to and from the body
Arteries and Veins
- Arteries: carry blood away from the heart
- Veins: carry blood back to the heart.
- Atria: receives blood
- Ventricles: pump blood
Flow Control in Circulatory System
- One-way flow valves
- Tricuspid, Pulmonary, Mitral, Aortic
Systemic Circulation: Arterial
- Left ventricle ejects ~80ml (bolus) of blood into Aorta (largest artery)
- Blood flows into medium-sized arteries and arterioles that branch off the aorta
- Vessels further divide into capillaries
Blood Vessels Structure
- Arteries and Arterioles
- Venules and Veins
- Vena Cava
Capillaries
- Slow blood flow allows for the exchange of nutrients, metabolic waste products, gases, hormones, between tissue and blood
Systemic Circulation: Venous Return
- Deoxygenated blood collects in venules
- Venules lead to medium-sized, then large veins, then to the vena cava (largest vein)
- Vena Cava delivers deoxygenated blood to heart via right atrium
Process of Blood Flow from the Heart
- Blood is pushed back to the heart by muscle action on veins
- One-way valves in veins prevent backflow due to gravity
Systemic Circulation
- In going to smaller arteries the diameters and velocity decreases, but the overall area of the vascular bed increases
Cardiac Cycle process
- Blood returns to the heart from circulation and collects in the atrium
- The atrium contracts and pushes blood into the ventricle.
- The ventricle contracts, ejecting blood into circulation.
Cardiovascular System - Electrical
- Autorythmic Cells: heart tissue made of two types of heart muscles
Types of Heart Muscle Cells
- Myocardial contractile cells: responsible for heart contractions
- Myocardial conductile cells: generate and spread electrical signals to control heartbeats, making up about 1%
Myocardial conductile cells Characteristics & Functions
- Self-excitable: They do not require an external signal to fire an action potential
- Unstable resting membrane potential: spontaneously depolarize at a set rate
- Pacemakers: setting the rhythmic electrical excitation that stimulates heartbeat
- Conduction System: ensures coordinated contraction of the atria and ventricles
Sinoatrial (SA) Node
- Natural pacemaker containing autorhythmic cells that generate electrical impulse (action potential)
- Ensures coordinated heart contraction
- Sends signals traveling at 1m/s through muscle fibres
- Action potential refers to the rise and fall of electrical potential across the cellular membrane
Atrioventricular (AV) Node
- Signal reaches the AV node 1/10 of a second after the SA node generates an impulse
- Regulates ventricular contraction by delaying the impulse
- AV node is the only electrical link between the atria and ventricles
- AV node slows down the impulse, preventing the ventricles from contracting too quickly
Bundle of His
- After passing through the AV node, the signal reaches the Bundle of His
- "Bundle"transmits signal through the cardiac muscles of both ventricles and splits into left and right bundle branches
Purkinje Fibres
- Specialized muscle cells with very fast conduction speeds
- They relay the signal to the ventricular walls ensuring the ventricles contract
Action Potential in Contractile Cardiac
- Brief repolarization: K+ outflow (transient K+ channels open)
- Plateau (maintained depolarization) due to: Ca2+ inflow and K+ outflow
Factors of Repolarization in Contractile Cardiac
- Closure of Ca2+ channels
- K+ outflow when additional voltage-gated K+ channels open
Action Potential in Autorhythmic Cardiac
- Rapid influx of Ca2+ leading to depolarization and outflux of K+ leading to repolarization
- Slow influx of Nat+ resulting in prepolarization
Electrocardiogram (ECG)
- ECG monitors electrical activity of cardiac muscles using placement of electrodes
Waves and Intervals of ECG Recording
- P-Wave: indicates the SA node initiates and the atria depolarize and contracts at the AV node delay
- Ventricles depolarize causing the QRS then the atria repolarizes
- T Wave: Ventricles repolarizing
ECGs can Diagnose
- Arrhythmias
- Heart blocks
- Myocardial Infarction
Arrhythmias that ECGs can diagnose
- Tachychordia: fast
- Brachychordia: slow
- Fibrilation: rapid, irregular
Heart Block Electrical Issues
- Pacemakers and ICDs are devices to treat bradycardia.
- ICD - detects irregular heart contractions and delivers an electrical impulse to restore ryhthm in high risk ventricular tachychordia or fibrilation.
Cardiac Cycle & Blood Pressure
- Cardiac Cycle has 2 phases
- Diastole: Ventricles relax and fill with blood
- Systole: Ventricles contract and pump blood out
Blood Pressure
- Systolic, healthy = ~90-120
- Diastolic = ~60-80
- Blood pressure drops further from the heart
Blood Pressure Phases
- Phase 1: Inflow phase AB→BC. Ventricular filling
- Phase 2: Isovolumetric contraction CD. Pressure↑, volume stays
- Phase 3: Outflow phase DE, EF. Aortic valve opens, blood eject
- Phase 4: Isoudumetric relaxation FA. Pressure, volume stays
Phases of Diastole vs Systole
- Systole: CDEF
- Diastole: FABC
Valvular Events and Cardiac events that occur during Ventricular Filling
- Open AV valves -> Rapid ventricular filling & Decreased Ventricular filling
- Closed AV valves -> Opening of semilunar valves and Ventricular Relaxation
Ventricular Filling, Atrial Contraction, Ventricular Contraction and Ventricular Ejection Phases
- Ventricular Filling: Ventricle relaxed w/ low pressure; Blood goes from Atria to Ventricle due to higher atrial pressure; AV values open to allow flow
- Atrial Contraction: Final push of blood into ventricle before contraction; End of diastole
- Ventricular Contraction: Start of systole; Ventriculor pressure rises to be greater than atrial which closes the AV valves to prevent backflow; Semilunar valves (aortic & pulmonary) remain closed(Isovolumetric contraction)
- Ventricular Ejection: Ventricular pressure exceeds the pressure in the aorta and pulmonary arteries, forcing semilunar valves to open; Blood is ejected into circulation.
Ventricular Relaxation
- Beginning of diastole
- Ventricular pressure drops, semilunar valves elose,
- AV valves elosed, resuts in isoudumetric relaxation
- When vetricular pressure < atrial pressure, AV Valves open and ventricles stort filiing again
Cardiac Cycle Thermodynamics
- Thermodynamic assumptions:
- Neglect changes in kinetic & potential energy
- Adiabatic, isentropic, steady flow, steady state
Pressure Levels in Cardiac Cycle
- P2: systolic pressure
- P1: atrial filling pressure
- V2: end diastolic volume
- V1: end systolic volume
Stroke Volume Defined
- (V2-V1 ) is often referred to as the stroke volume (SV)
Valves of the Cardiac Cycle
- Valve A (inflow) closes
- Valve B(Outflow) opens
- Valve c (Outflow) Closes
- Valve D (Inflow)Opens
Modelling Cardiac Cycle
- Win = ∫21 Pdv= P2 (V1-V₂)
- Wout = ∫21 Pdv = P1 (V2-V1 )
Additional Variables in Cardiac Cycle
- P2 = Systolic pressure
- P1 = Atrial filling pressure
- V2 = End diastolic volume
- V1 = End systolic volume
Stroke Volume Equations
- Wnet = Win + Wout
- Pw = Wnet * h {h = heart rate}
- CO= h (SV) = h (V2-V1)
- EF = (SV/ EDV 100 )/{EDV: End-Diastolic Volume}
Left Ventricle Heart Failure Dysfunctions
- Systolic Dysfunction: reduced ejection fraction and enlarged ventricle chamber
- Diastolic Dysfunction: increased resistance to filling w/ increased filling pressures
Left Ventricular Assist Device (LVADS)
- Mechanical Circulatory support for heart failure
- Bridge to support cardiac function and health to transplant patient
- Destination therapy that consist of long term patient care
- Bridge to recovery from prolonged LVAD
Blood Rheology
- Study of materials w solid & fluid characteristics
- Fluid Rheology: Compares fluids based on shear stress (z) vs. shear rate (du/dy) behavior
- Newtonian Fluid: t = - m (du/dy) with m defined as fluid viscosity
- Bingham Fluid: T = t + k 8
- Casson Fluid: t(½) = T(½) + kc(½); non-newtonian- yield-stress & pseudoplastic- like behavior
Composition of Blood and Plasma
- Cells: Erythrocytes (Red Blood Cells) make up 95% cellular content w/ White Blood Cells (0.1%) and Platelets (4.9%)
- Plasma: Liquid component of blood
Liquid Component of Blood
- Contains salt, sugars, proteins, amino acids, fats,
Proteins in Plasma
- Albumin then fibrinogen
- Newtonian fluid, viscosity: 1.16-1.35 mPa's(cP)
Yield Stress Influences on Properties of RBC's
- Yield Stress arises due to presence of RBC and Fibrinogen
- t (½)= [(H*.1) (CF+0.5)] +[(μ )/(1−H)a(x)];-2
Fibrinogen Facts
- Protein that interacts w RBC
- In saline, RBCs act as newtonian fluid, but fibrinogen binds RBCs together
Hematocrit Properties
- Proportion of blood volume occupied by RBC's (Normal hematocril levels: 0.35-0.50)
- RBCs :tend to stich together when close
- Fibrinogen & Hematocrit contribute to bloods non-Newtonian behavior by ↑ yield stress
Characteristics of Blood viscosity
- Relatively low hematocrits, viscosity increases because of The stickiness of red blood cells and viscosity increases because of cell deformation in high hematocrit
- Decreases with increasing sheer rate
Factors involved in Blood Viscosity Properties
- For large vessels, Viscosity is independent of vessel diameter; diameter decrease and viscosity decreases to a point
- Hematrocrit and tubular diameter
- With given diameter the viscosity is directly related to hematocrit
- diameter increases the diameter is inversely related to viscosity
Fahreous - Lindquist Effect
- Observation that blood viscosity decreases steeply at lower radii. –4 factors influencing:
The Factors of Fahreous - Lindquist Effect in blood Viscosity
- Axial Accumulation -RBCs migrate toward enter, leaving ell free plasma near wall
- -Reduces friction btw walls & RBC, lowering viscosity
- Limited Number of Laminae
- In small vessels, number of fluid layers lower. More efficient flow
- Tank treading of RBC -RBCs spin w plasma, moving like tank treads,Minimizes energy lass
- Deformation of RBC:
- RBC becomes bullet shaped in small vessels which, Reduces viscosity
- For Newtonian Fluids, to/ y is rated constant Z= μ
- Y For Non-Newtonian fluids/ y ratio changes y.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.