Podcast
Questions and Answers
What is the most common site for endometriosis?
What is the most common site for endometriosis?
- Broad ligament
- Uterosacral ligaments
- Pouch of Douglas
- Ovary (correct)
Endometriosis regresses during pregnancy due to increased estrogen levels.
Endometriosis regresses during pregnancy due to increased estrogen levels.
False (B)
What effect do oral contraceptive pills (OCPs) have on endometriosis?
What effect do oral contraceptive pills (OCPs) have on endometriosis?
They decrease local estrogen levels and promote endometrial thinning.
Endometriosis is primarily associated with an _____ condition.
Endometriosis is primarily associated with an _____ condition.
Match the following risk factors with their effects on estrogen levels:
Match the following risk factors with their effects on estrogen levels:
What is the recommended treatment for moderate to severe tubal factors causing infertility?
What is the recommended treatment for moderate to severe tubal factors causing infertility?
Total Abdominal Hysterectomy (TAH) allows for retrograde menstruation.
Total Abdominal Hysterectomy (TAH) allows for retrograde menstruation.
Name one cause of infertility related to follicular health.
Name one cause of infertility related to follicular health.
If a patient with endometrioma desires pregnancy, it is advisable not to manage the cyst due to the risk of __________.
If a patient with endometrioma desires pregnancy, it is advisable not to manage the cyst due to the risk of __________.
Match the following conditions to their appropriate management:
Match the following conditions to their appropriate management:
Which of the following is considered a specific symptom of endometriosis?
Which of the following is considered a specific symptom of endometriosis?
What is considered a first-line treatment for mild dysmenorrhea associated with endometriosis?
What is considered a first-line treatment for mild dysmenorrhea associated with endometriosis?
Laparoscopic management for endometriosis includes adhesiolysis.
Laparoscopic management for endometriosis includes adhesiolysis.
Laparoscopy is primarily used for both diagnostic and therapeutic purposes in the investigation of endometriosis.
Laparoscopy is primarily used for both diagnostic and therapeutic purposes in the investigation of endometriosis.
What does 'B/L' likely refer to in medical terms?
What does 'B/L' likely refer to in medical terms?
Name a drug that can lead to endometrial atrophy in the treatment of endometriosis.
Name a drug that can lead to endometrial atrophy in the treatment of endometriosis.
The gold standard for diagnosing endometriosis is __________.
The gold standard for diagnosing endometriosis is __________.
Severe endometriosis may require treatment options including _____ if first-line medical management fails.
Severe endometriosis may require treatment options including _____ if first-line medical management fails.
Match the following symptoms and findings related to endometriosis:
Match the following symptoms and findings related to endometriosis:
Match the drug to its side effect:
Match the drug to its side effect:
Which of the following is a common physiological symptom of Premenstrual Syndrome (PMS)?
Which of the following is a common physiological symptom of Premenstrual Syndrome (PMS)?
A diagnosis of PMS can be made if all symptoms are present only in the pre-ovulatory phase.
A diagnosis of PMS can be made if all symptoms are present only in the pre-ovulatory phase.
Name one treatment option for insomnia associated with PMS.
Name one treatment option for insomnia associated with PMS.
The ___________ is considered the gold standard for diagnosing Pelvic Inflammatory Disease (PID).
The ___________ is considered the gold standard for diagnosing Pelvic Inflammatory Disease (PID).
Match the following PMS management options with their intended use:
Match the following PMS management options with their intended use:
What is the primary cause of primary dysmenorrhea?
What is the primary cause of primary dysmenorrhea?
Secondary dysmenorrhea is typically associated with younger females.
Secondary dysmenorrhea is typically associated with younger females.
What condition refers to hidden menstruation due to an obstruction in the passage?
What condition refers to hidden menstruation due to an obstruction in the passage?
Dysmenorrhea that decreases on its own after physical activity is classified as ________ dysmenorrhea.
Dysmenorrhea that decreases on its own after physical activity is classified as ________ dysmenorrhea.
Match the types of dysmenorrhea with their characteristics:
Match the types of dysmenorrhea with their characteristics:
What characteristic appearance is associated with a chocolate cyst?
What characteristic appearance is associated with a chocolate cyst?
The presence of chocolate cysts indicates a mild form of endometriosis.
The presence of chocolate cysts indicates a mild form of endometriosis.
Identify one common ultrasound appearance associated with chocolate cysts.
Identify one common ultrasound appearance associated with chocolate cysts.
Chocolate cysts are diagnostic indicators of __________ disease.
Chocolate cysts are diagnostic indicators of __________ disease.
Match the following laparoscopy findings with their descriptions:
Match the following laparoscopy findings with their descriptions:
What does a positive result in the Progesterone Challenge Test (PCT) indicate?
What does a positive result in the Progesterone Challenge Test (PCT) indicate?
An FSH level of greater than 25 IU/L indicates hypergonadotropic hypogonadism.
An FSH level of greater than 25 IU/L indicates hypergonadotropic hypogonadism.
What is the management approach for pituitary apoplexy?
What is the management approach for pituitary apoplexy?
A negative result in the Progesterone Challenge Test (PCT) indicates the need for further investigation into ________.
A negative result in the Progesterone Challenge Test (PCT) indicates the need for further investigation into ________.
Match the following conditions with their possible investigations or characteristics:
Match the following conditions with their possible investigations or characteristics:
Which theory explains endometriosis located at the umbilicus?
Which theory explains endometriosis located at the umbilicus?
Dysmenorrhea is the most common symptom associated with endometriosis.
Dysmenorrhea is the most common symptom associated with endometriosis.
List one common extragenital site for endometriosis.
List one common extragenital site for endometriosis.
The classical triad of symptoms for endometriosis includes 2º dysmenorrhea, dyspareunia, and __________.
The classical triad of symptoms for endometriosis includes 2º dysmenorrhea, dyspareunia, and __________.
Match the endometriosis theories with their corresponding sites:
Match the endometriosis theories with their corresponding sites:
Which of the following is a defect that can cause secondary amenorrhea related to the pituitary gland?
Which of the following is a defect that can cause secondary amenorrhea related to the pituitary gland?
The most common symptom of Sheehan syndrome is persistent amenorrhea.
The most common symptom of Sheehan syndrome is persistent amenorrhea.
What hormonal patterns are observed in obesity-related amenorrhea?
What hormonal patterns are observed in obesity-related amenorrhea?
In cases of Hypothalamic amenorrhea, LH and FSH levels are typically _____ and Estrogen levels are _____ .
In cases of Hypothalamic amenorrhea, LH and FSH levels are typically _____ and Estrogen levels are _____ .
Match the following defects to their corresponding hormonal patterns:
Match the following defects to their corresponding hormonal patterns:
Flashcards are hidden until you start studying
Study Notes
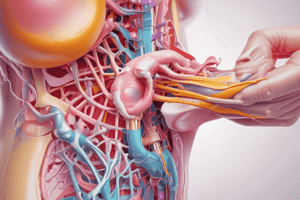
Pathophysiology & Theories
- Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterus.
- This ectopic tissue is hormonally active and responds to estrogen.
- During menstruation, the ectopic tissue sheds and bleeds, causing inflammation and adhesion formation, leading to chronic inflammation.
Estrogen dependent state
- Endometriosis regresses during pregnancy due to increased progesterone levels.
- After menopause, the condition also regresses due to lower estrogen levels.
Risk Factors
- Nulliparity is a significant risk factor due to higher estrogen levels.
- Early menarche and late menopause also increase risk, contributing to prolonged estrogen exposure.
- Low BMI increases risk as well, as does obesity (high BMI).
Protective Factors
- Multiparity is protective due to decreased estrogen levels.
- Prolonged use of oral contraceptives can reduce local estrogen levels and endometrial thickness.
- Smoking can decrease local estrogen levels by stimulating aromatase.
Epidemiology
- Endometriosis most commonly affects women of reproductive age (25-35 years).
- Teenage girls with endometriosis may have müllerian malformations.
- There is a genetic predisposition, with the K-RAS gene being associated with endometriosis.
Site
- The most common site is the ovary, where it may form a chocolate cyst (endometrioma).
- Other common locations include the pouch of Douglas, broad ligament, and uterosacral ligaments.
- Rare sites include the spleen and central nervous system.
- Endometriosis can be found anywhere in the body, including the nose, lungs, umbilicus, and surgical scars like cesarean sections and episiotomies.
General Gynecology
- Total abdominal hysterectomy (TAH) is a last resort in managing endometriosis.
- TAH eliminates retrograde menstruation and prevents new implants from forming, halting the disease's progression.
Infertility
- Endometriosis can cause infertility by affecting follicular growth, causing anovulation, and distorting anatomy.
- In mild to minimal cases, it can be treated as unexplained infertility.
- Moderate to severe tubal factors may require in vitro fertilization (IVF).
- Clomiphene citrate and intrauterine insemination (IUI) can be tried for 3 cycles before considering IVF.
Endometrioma
- Endometriomas cannot be managed medically.
- If a woman desires pregnancy, cystectomy is recommended to avoid damaging the follicle.
- If pregnancy is not desired, asymptomatic cysts smaller than 5 cm are monitored by ultrasound.
- Symptomatic or cysts larger than or equal to 5 cm are treated by laparoscopic cystectomy, and the specimen is sent for histopathological evaluation.
Endometriosis Staging
- Endometriosis is staged as mild, moderate, or severe.
Indications for Surgery
- Surgical intervention is indicated when medical management fails.
- Specific indications include adhesions, chocolate cysts, and pelvic cavity distortion.
Treatment
- Dysmenorrhea is managed differently based on severity.
- In mild to minimal cases, primary dysmenorrhea treatment is used, including oral contraceptive pills as first-line therapy or NSAIDs if pregnancy is desired. Progesterone is a second-line option.
- For moderate to severe dysmenorrhea, continuous GnRH agonists or GnRH antagonists are the first-line treatment. Laparoscopy is considered if these fail.
- Mirena (oral) is a third-line option.
- If all three lines fail, laparoscopy is necessary.
Other Drugs
- Danazol or Gestrinone can be used, but they have side effects including hirsutism.
- Letrozole (aromatase inhibitor) is another option.
- Mifepristone causes endometrial atrophy.
Drugs not used
- Misoprostol (PGE₂) is not used due to its pain-inducing properties.
Laparoscopic Management
- Laparoscopic procedures include adhesiolysis, fulguration of implants, cystectomy when indicated, pre-sacral neurectomy, and LUNA (Laparoscopic Uteroscopic Nerve Ablation).
Specific Symptoms ("VCC")
- Vicarious menstruation: Menstrual bleeding from other sites.
- Cyclical hematuria: Blood in the urine during menstruation.
- Catamenial hemothorax/pneumothorax: These conditions occur during menstruation.
Menstrual Abnormalities
- Heavy menstrual bleeding (HMB)
- Inflammation of the ovary
- Abnormal follicular growth
Pain - Causes
- Pain in endometriosis is caused by adhesion formation, peritoneal inflammation, local prostaglandin production, and deeper infiltration causing nerve irritation.
Examination Signs
- Per abdomen: Not significant.
- Per vaginal :
- Uterus: Normal size.
- Uterus: Retroverted and fixed due to adhesions, non-tender.
- Adnexa: Bilateral adnexal mass (chocolate cyst) with or without adnexal tenderness.
- Uterosacral ligament: Nodularity and tenderness.
Investigations
- Transvaginal Sonography (TVS): Used to rule out other disorders and detect chocolate cysts.
- Laparoscopy: Provides both diagnostic and therapeutic value to visualize lesions, stage disease, and biopsy for histopathological examination.
- Histopathological Examination (HPE): The gold standard for diagnosing endometriosis; involves examining a biopsy of the endometrial implant.
Severity
- The depth of the lesion correlates with the severity of endometriosis.
- Severity is independent of the extent of the disease.
Premenstrual Syndrome (PMS)
- PMS is characterized by mood swings and bloating, often interfering with daily life.
Diagnosis
- Diagnosis of PMS requires the presence of five specific criteria:
- Symptoms interfering with routine activity.
- Symptoms occurring in at least three consecutive cycles.
- Symptoms resolving after menstruation.
- Symptoms present in the post-ovulatory phase.
- Symptoms absent in the pre-ovulatory phase.
Management
- Fluoxetine, an SSRI, is the standard of care for PMS.
- Alprazolam can be used for insomnia.
- Evening primrose oil may help with breast tenderness.
- Diuretics are used for water retention.
- Pyridoxine is also part of PMS management.
Lifestyle Changes
- Reduced sugar intake
- Reduced salt intake
- Reduced caffeine intake
Chronic Pelvic Pain
- Pelvic pain lasting for two or more months.
- Laparoscopy is typically recommended in these cases.
Laparoscopy
- Laparoscopy is the gold standard for diagnosing chronic pelvic pain, endometriosis, and pelvic inflammatory disease (PID).
Cyclical Abdominal Pain
- Cryptomenorrhea: Hidden menstruation due to obstruction in the passage and failure of menstrual blood flow. Causes include imperforate hymen, transverse vaginal septum, and vaginal atresia.
- Mittelschmerz Syndrome: Pain during ovulation, presenting with midcycle pain.
- Dysmenorrhea: Pain during menstruation.
- Primary Dysmenorrhea: Pain due to the release of prostaglandins, without pelvic pathology.
- Onset: Begins with or just before menses, decreasing within 72 hours.
- Pain: Centralised suprapubic pain, decreasing with physical activity, marriage, or childbirth.
- Progression: Pain progressively decreases.
- Management: NSAIDs or OCPs to make cycles anovulatory.
- Secondary Dysmenorrhea: Pain due to pelvic pathology, most commonly endometriosis.
- Onset: Occurs well before and continues after the onset of menses.
- Pain: Localized pain.
- Progression: Pain progressively increases.
- Management: Treatment of the underlying cause.
- Note:* The table shows a summary of primary and secondary dysmenorrhea. The details are based on the provided text. "PGF ad" and "(m/c)" are abbreviations that weren't clarified in the document. "mx" likely refers to management or further investigation.
Chocolate Cyst (Endometrioma)
- Chocolate cyst formation is a result of bleeding in the ovary, eventually forming a cyst with a brown color due to hemosiderin.
- The brown color indicates severe disease.
Laparoscopy Findings
- Laparoscopy may reveal chocolate cysts, adhesions, peritoneal defects, and superficial peritoneal deposits.
Ultrasound (USG) Appearance
- Chocolate cysts appear with a "ground glass" appearance and homogeneous internal echo on ultrasound.
Histology
- Red Nodules (Red Flame Lesions): Red in color and indicate fresh implants.
- Black Nodules (Powder Burn Appearance/Gunshot Appearance): Dark in color and indicate old lesions.
Uses of Laparoscopy
- Laparoscopy allows for direct visualization of lesions, staging of disease, biopsy, and therapeutic intervention.
Compartmentwise Causes of 2º Amenorrhea
- This table outlines the causes of secondary amenorrhea based on the affected organ and its potential defects.
Sheehan Syndrome
- Pathophysiology: PPH leading to pituitary gland necrosis.
- Clinical Features: The most common symptom is failure of lactation. Persistent amenorrhea is also common.
- Investigations: Hormone levels, with growth hormone being the first to decline and TSH the last. MRI shows an empty sella turcica.
Work Up of a Case of Secondary Amenorrhea
- Initial Evaluation: Measure FSH and estrogen levels. FSH levels higher than 25 IU/L and low estrogen levels suggest a problem.
- Further Tests:
- Hypergonadotropic hypogonadism: Suggests anterior pituitary problems.
- Post-ovulatory bleeding: Possible ovarian failure.
- Progesterone Challenge Test (PCT): If FSH levels are less than or equal to 10 IU/L, a PCT is conducted.
- Positive PCT: Further investigation is needed.
- Negative PCT: Further investigation is required.
Additional Investigations
- MRI: To rule out anatomical causes like empty sella turcica, Sheehan syndrome, and space-occupying lesions.
- Asherman Syndrome: Condition causing intrauterine adhesions.
- Prolactinoma: Benign tumor of the pituitary gland producing prolactin.
- Signs: Headache, visual disturbances, post-partum collapse (decrease in ACTH), hypoglycemia.
Pituitary Apoplexy
- Pathogenesis: Occurs in pregnant females with undiagnosed adenomas, where post-partum hemorrhage causes pituitary infarction and hemorrhage.
- Management: Corticosteroids.
General Gynaecology
- The text highlights the theories of endometriosis based on the site of the ectopic endometrial tissue:
Theories of Endometriosis
- Ovary/POD/Uterosacral ligament: Theory of retrograde menstruation (Sampson's Theory of Implantation)
- Umbilicus: Halban's Theory of Lymphatic Spread
- Lungs: Ivanoff's Theory of Coelomic metaplasia
- Scar Endometriosis: Direct implantation
Implantation Theory of Sampson's
- Most common site: Ovary > POD.
- Most common extragenital site: Sigmoid colon.
- More common in: Females with short, frequent cycles.
- Causes: Outflow tract obstruction (imperforate hymen, transverse vaginal septum), and Müllerian malformation.
- Mechanism: Retrograde flow of menstrual blood.
- Important Note:* "d/t" is an abbreviation for "due to."
Symptoms & Signs
- Most common symptom: Pain (secondary dysmenorrhea > Chronic pelvic pain > Dyspareunia)
- Second most common symptom: Infertility
- Third most common symptom: Adnexal mass (chocolate cyst).
- Classic Triad: Secondary dysmenorrhea, Dyspareunia, Infertility.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.