Podcast
Questions and Answers
Which theory proposes endometrial fragments are transported through the fallopian tubes during menstruation and implant in the pelvic peritoneum?
Which theory proposes endometrial fragments are transported through the fallopian tubes during menstruation and implant in the pelvic peritoneum?
- Halban's Theory
- Meyer and Ivanoff Theory
- Sampson's Theory (correct)
- Vascular Theory
What is the name of the theory that suggests endometriosis arises from the transformation of coelomic epithelium due to chronic irritation by menstrual blood?
What is the name of the theory that suggests endometriosis arises from the transformation of coelomic epithelium due to chronic irritation by menstrual blood?
- Vascular Theory
- Meyer and Ivanoff Theory (correct)
- Sampson's Theory
- Halban's Theory
Which theory offers a plausible explanation for endometriosis developing at distant sites like the lungs, arms, or thighs?
Which theory offers a plausible explanation for endometriosis developing at distant sites like the lungs, arms, or thighs?
- Direct Implantation
- Sampson's Theory
- Vascular Theory (correct)
- Halban's Theory
Which of the following factors is NOT mentioned as a risk factor for developing endometriosis?
Which of the following factors is NOT mentioned as a risk factor for developing endometriosis?
Which theory focuses on the growth of endometrial or decidual tissue at new sites after implantation, particularly following surgical procedures like hysterectomy, caesarean section, or tubectomy?
Which theory focuses on the growth of endometrial or decidual tissue at new sites after implantation, particularly following surgical procedures like hysterectomy, caesarean section, or tubectomy?
Which of the following is NOT a common clinical manifestation of endometriosis?
Which of the following is NOT a common clinical manifestation of endometriosis?
Which of the following is considered the 'gold standard' for diagnosing endometriosis?
Which of the following is considered the 'gold standard' for diagnosing endometriosis?
What is the first-line medical management for mild dysmenorrhea associated with endometriosis?
What is the first-line medical management for mild dysmenorrhea associated with endometriosis?
Which of the following surgical procedures is considered 'conservative' in the management of endometriosis?
Which of the following surgical procedures is considered 'conservative' in the management of endometriosis?
What is the most appropriate treatment option for endometriosis in a woman who has completed her family and does not desire future pregnancies?
What is the most appropriate treatment option for endometriosis in a woman who has completed her family and does not desire future pregnancies?
Flashcards
Endometriosis
Endometriosis
Presence of endometrial tissue outside the uterus.
Retrograde menstruation
Retrograde menstruation
Menstrual blood flows back into the pelvic cavity.
Coelomic Metaplasia
Coelomic Metaplasia
Chronic irritation causes normal cells to become endometrial cells.
Lymphatic theory
Lymphatic theory
Signup and view all the flashcards
Direct Implantation
Direct Implantation
Signup and view all the flashcards
Dyspareunia
Dyspareunia
Signup and view all the flashcards
Chronic Pelvic Pain
Chronic Pelvic Pain
Signup and view all the flashcards
Laparoscopy
Laparoscopy
Signup and view all the flashcards
Infertility
Infertility
Signup and view all the flashcards
Study Notes
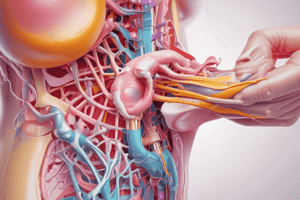
Definition
- Endometriosis is the presence of endometrial tissue (glands and stroma) outside the uterus.
Risk Factors
- First-degree relatives have a 6 times higher risk of endometriosis.
- Early menstruation (before age 11) increases risk.
- Shorter menstrual cycles (less than 27 days) increase risk.
- Heavy menstrual periods (lasting over 7 days) increase risk.
- Nulliparity (never having given birth) increases risk.
- Obstruction of menstrual flow (Müllerian anomalies) increase risk.
Pathophysiology
- Under hormonal influence, endometrial tissue outside the uterus thickens, breaks down, and bleeds each month.
- Trapped blood forms cysts.
- The trapped blood irritates surrounding tissue, causing scar tissue and adhesions.
- This can lead to infertility and pain.
Pathogenesis (Theories)
- Sampson's theory (Retrograde menstruation): Menstrual blood flows backward through fallopian tubes, implanting endometrial tissue in pelvic organs. This theory only explains pelvic endometriosis.
- Meyer and Ivanoff theory (Coelomic metaplasia): Chronic irritation of pelvic peritoneum by menstrual blood causes metaplasia, explaining endometriosis in abdominal viscera, retrovaginal septum and umbilicus.
- Halban's theory (Lymphatic theory): Normal endometrium can metastasize to pelvic lymph nodes through lymphatic channels.
- Vascular theory: Endometriosis can occur in distant sites like lungs or arms.
- Direct implantation: Endometrial or decidual tissues implant in susceptible sites, such as abdominal scars from surgery.
Sites of Endometriosis
- Pelvic: Ovary, cul-de-sac, uterosacral ligaments, posterior surface of the uterus, posterior broad ligament, rectovaginal septum, tubes and round ligaments.
- Extrapelvic (less common): Lungs, thorax, urinary tract, cervix, hernial sacs, umbilicus, laparotomy/episiotomy sites, tubal stumps after sterilization, extremities.
Clinical Manifestations
- Dyspareunia (painful intercourse)
- Dysuria (painful urination)
- Chronic pelvic pain
- Dysmenorrhea (painful menstruation)
- Abnormal menstruation
- Infertility
Physical Examination
- Abdominal examination may not show abnormalities.
- A mass in the lower abdomen might be felt, potentially due to endometriosis lesions.
- Pelvic examination may detect tenderness, nodules in the pouch of Douglas, or bilateral adnexal masses.
- Bluish spots at the posterior fornix during speculum examination might suggest endometriosis.
Diagnostic Tests
- Transvaginal ultrasound (TVS)
- Laparoscopy (the gold standard for diagnosis)
- Serum CA-125 (non-specific marker, higher in severe endometriosis).
Stages of Endometriosis
- Staged using factors like location, number and size of lesions, and depth of the endometrial implants. (Minimal, Mild, Moderate, Severe)
Treatment
- Medical: NSAIDs (first-line for mild dysmenorrhea), OCT (3 months), progestins (DMPA, MPA, NETA), aromatase inhibitors.
- Surgical: Excision of endometrium, adhesions removal, restoration of pelvic anatomy, endometriosis cystectomy (if cyst >5cm), fulguration (ablation of endometriotic deposits), LUNA (laparoscopic uterosacral nerve ablation), and hysterectomy + BSO (optional).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.