Podcast
Questions and Answers
Which of the following conditions is NOT associated with medical management?
Which of the following conditions is NOT associated with medical management?
- Chocolate Cyst (correct)
- Bowel Endometriosis (correct)
- Bladder Endometriosis (correct)
- None of the above
Cyclical hematuria is specifically associated with bladder endometriosis.
Cyclical hematuria is specifically associated with bladder endometriosis.
True (A)
What imaging technique is advised for assessing deep endometriosis and bladder or bowel involvement?
What imaging technique is advised for assessing deep endometriosis and bladder or bowel involvement?
MRI
The __________ sign refers to an imaging finding associated with certain endometriosis presentations.
The __________ sign refers to an imaging finding associated with certain endometriosis presentations.
Match the following endometriosis-related features with their descriptions:
Match the following endometriosis-related features with their descriptions:
What is the recommended management for symptomatic fibroids?
What is the recommended management for symptomatic fibroids?
Adenomyosis can only be definitively diagnosed through imaging techniques.
Adenomyosis can only be definitively diagnosed through imaging techniques.
What is the gold standard investigation for adenomyosis?
What is the gold standard investigation for adenomyosis?
To manage an endometrial polyp, the procedure of ________ is often performed.
To manage an endometrial polyp, the procedure of ________ is often performed.
Match the following conditions with their management:
Match the following conditions with their management:
Which of the following is a characteristic finding in fibroid on per abdominal examination?
Which of the following is a characteristic finding in fibroid on per abdominal examination?
Adenomyosis can be identified by the presence of a mass with a texture similar to myometrium on ultrasound.
Adenomyosis can be identified by the presence of a mass with a texture similar to myometrium on ultrasound.
What is the maximum size of a uterus affected by fibroid during examination?
What is the maximum size of a uterus affected by fibroid during examination?
A solid mass arising from a narrow base is characteristic of a ______.
A solid mass arising from a narrow base is characteristic of a ______.
Match the following examination findings with the correct condition:
Match the following examination findings with the correct condition:
What condition is associated with pedunculated fibroids?
What condition is associated with pedunculated fibroids?
Hyaline degeneration leads to a whorled appearance of the fibroid.
Hyaline degeneration leads to a whorled appearance of the fibroid.
What type of degeneration begins from the periphery of the fibroid?
What type of degeneration begins from the periphery of the fibroid?
The least common type of fibroid degeneration is known as __________.
The least common type of fibroid degeneration is known as __________.
Match the types of degeneration with their characteristics:
Match the types of degeneration with their characteristics:
What is a common clinical presentation of red degeneration in fibroids during pregnancy?
What is a common clinical presentation of red degeneration in fibroids during pregnancy?
Red degeneration is exclusively observed in pregnant women.
Red degeneration is exclusively observed in pregnant women.
What is the primary cause of red degeneration in fibroids?
What is the primary cause of red degeneration in fibroids?
A painful fibroid in a peri/post menopausal female may indicate __________.
A painful fibroid in a peri/post menopausal female may indicate __________.
Match the following features of red degeneration with their descriptions:
Match the following features of red degeneration with their descriptions:
What is the most common symptom associated with heavy menstrual bleeding (HMB)?
What is the most common symptom associated with heavy menstrual bleeding (HMB)?
Submucosal fibroids are the primary cause of both heavy menstrual bleeding and subfertility.
Submucosal fibroids are the primary cause of both heavy menstrual bleeding and subfertility.
What are common pressure symptoms associated with cervical fibroids?
What are common pressure symptoms associated with cervical fibroids?
The main cause of subfertility related to fibroids is __________ interference with implantation.
The main cause of subfertility related to fibroids is __________ interference with implantation.
Match the types of fibroids with their associated symptoms:
Match the types of fibroids with their associated symptoms:
What is the most common type of fibroid?
What is the most common type of fibroid?
Fibroids exhibit a decrease in size during menopause.
Fibroids exhibit a decrease in size during menopause.
Name two hormones that fibroids are dependent on.
Name two hormones that fibroids are dependent on.
All fibroids initially develop as __________ fibroids.
All fibroids initially develop as __________ fibroids.
Match the following fibroid types with their locations:
Match the following fibroid types with their locations:
What characterizes a submucous fibroid on Hysteroscopy?
What characterizes a submucous fibroid on Hysteroscopy?
An endometrial biopsy is the first investigation for Abnormal Uterine Bleeding.
An endometrial biopsy is the first investigation for Abnormal Uterine Bleeding.
What is the best investigation method for diagnosing a submucous fibroid?
What is the best investigation method for diagnosing a submucous fibroid?
An adenomyosis diagnosis is suggested if the T2 measurement is greater than or equal to ____ mm.
An adenomyosis diagnosis is suggested if the T2 measurement is greater than or equal to ____ mm.
Match the conditions with their characteristics based on HSG findings:
Match the conditions with their characteristics based on HSG findings:
Which symptom is primarily associated with fibroids?
Which symptom is primarily associated with fibroids?
Adenomyosis primarily occurs in nulliparous women.
Adenomyosis primarily occurs in nulliparous women.
What type of tumor is a fibroid?
What type of tumor is a fibroid?
The most common cause of post-menopausal bleeding is a __________.
The most common cause of post-menopausal bleeding is a __________.
Which of the following is a common appearance feature of adenomyosis?
Which of the following is a common appearance feature of adenomyosis?
Match each condition with its corresponding characteristics:
Match each condition with its corresponding characteristics:
Polyps most often cause irregular intra-menstrual bleeding in perimenopausal women.
Polyps most often cause irregular intra-menstrual bleeding in perimenopausal women.
What is the primary incidence age range for polyps?
What is the primary incidence age range for polyps?
What type of fibroid originates from within the uterus?
What type of fibroid originates from within the uterus?
A posterior cervical fibroid presses against the bladder.
A posterior cervical fibroid presses against the bladder.
What is the significance of submucosal fibroids regarding treatment?
What is the significance of submucosal fibroids regarding treatment?
A __________ fibroid arises from the broad ligament.
A __________ fibroid arises from the broad ligament.
Match the fibroid types with their characteristics:
Match the fibroid types with their characteristics:
Flashcards are hidden until you start studying
Study Notes
Medical Management
- Medical management is not useful for chocolate cysts, bladder endometriosis, or bowel endometriosis.
Imaging
- MRI is recommended for:
- Bladder endometriosis
- Bowel endometriosis
- Deep endometriosis of the rectosigmoid
- Hypertrophy of the mucosa, submucosa, and muscularis propria (on MRI)
Mushroom Cap Sign
- This refers to an abnormality seen on an MRI scan, but the details of its appearance are not provided.
Cyclical Hematuria
- Occurrence of hematuria during menstruation can be caused by:
- Bladder endometriosis
- Uterovesical fistula (fistula between the uterus and bladder)
Fibroid
- Most common pelvic tumor in females.
- Primarily found in reproductive-aged women (25-35 years)
- More common in nulliparous women (women who have not given birth)
- Estrogen and progesterone-dependent tumor
- Symptoms include:
- Heavy menstrual bleeding (HMB)
- Earlier menorrhagia (excessive menstrual bleeding)
- Regular cycles
- Secondary dysmenorrhea (painful menstruation)
- Infertility
- Pressure symptoms
- Pregnancy complications
Polyp
- Localized outgrowth of the endometrium
- Can be seen in all age groups
- Increased chance of polyps with age (most common age: 40-49 years)
- Increased incidence in women using Tamoxifen
- Most common cause of postmenopausal bleeding
- Symptoms include:
- Menorrhagia (HMB)
- Secondary dysmenorrhea
Adenomyosis
- Endometrial tissue (glands + stroma) present within the myometrium (at least 2.5 mm deep from the basal layer of endometrium).
- More common in women aged 40+
- More common in multiparous women (women who have given birth multiple times)
- Symptoms:
- Endometriosis and fibroids
- Menorrhagia (HMB)
- Secondary dysmenorrhea
- Chronic Pelvic Pain (CPP)
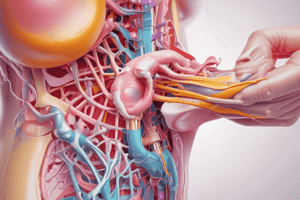
Gross Appearance (Table Summary)
| Feature | Fibroid | Polyp | Adenomyosis |
|---|---|---|---|
| Appearance | Rounded/oval & whorled, White, Firm | Fleshy, Red, Smooth surface, broad base | Symmetrically enlarged uterus: Globular uterus |
| Arises | Broad base, surrounded by pseudocapsule | Hangs from narrow base in uterine cavity | Basal layer of Endometrium infiltrates myometrium ; Cut section: multiple hemorrhages in myometrium |
| Other | Connective tissue, blood vessels | Mucosal outgrowth | Myometrial hypertrophy & hyperplasia |
General Gynaecology
- Active space is a term mentioned, but without proper context, its meaning is unclear and cannot be explained further.
Investigations
- 1st Ix (Initial investigation)
- AUB: Abnormal Uterine Bleeding
- UPT: Urine Pregnancy Test
- TVS: Transvaginal Sonography
- 240 years - Endometrial Biopsy: (The text mentions "240 years" but this is likely a typo. It may be interpreted as an age range, but without further context, the exact meaning is unclear.)
- INV (Investigation)
- EST: Estrogen
- IO: Imaging and Other
- TVS: Transvaginal Sonography
- Submucous fibroid
- SIS > TVS (Saline Infusion Sonography is better than TVS in this case)
- Best Ix: Hysteroscopy
- TVS: Transvaginal Sonography
- N: Normal
- S:
- T:
- I:
- O:
- N:
- S:
- LOC: Location
- MRI: Usually not required.
- T2: ≥ 12 mm: Adenomyosis; < 8 mm: Rules out Adenomyosis.
- TZ: Blurry + Endometrial glands.
Fibroid (Detailed)
- On Per Abdominal (P/A) Examination:
- Abdomino-pelvic lump
- Midline mass
- Mobile
- Firm
- Size: Up to 20 weeks pregnant uterus
- On Per vaginal (P/v) Examination:
- Bimanual palpation: Abdomino pelvic mass: Firm, mobile
- Cannot separate from uterus
- Asymmetrically enlarged, non-tender uterus
- Movement of Transmitted to cervix
- On USG:
- Mass distorting uterine cavity
- Posterior acoustic shadow
- Texture: Similar to myometrium
- Fibroid with texture of myometrium on SIS (Saline Infusion Sonography)
- On Doppler: Vascularity around fibroid periphery
Polyp
- Normal:
- Solid mass arising from a narrow base
- Polyp texture: Not the same as myometrium
- On USG:
- Polyp supplied by a single blood vessel upto the centre → Feeder vessel sign
- Enlarged uterus
- Venetian blind appearance (alternate dark & light bands)
Adenomyosis
- On Per Abdominal (P/A) Examination:
- Uterus: Symmetrically enlarged, globular
- Size: 10-12 weeks pregnant uterus (Never 24 weeks)
- Tender: Halban sign
- Adnexal tenderness
- On USG:
- Thickening of wall of uterus: Posterior > Anterior
- Most specific sign: Collection of blood in myometrium = myometrial cyst
- Histology::
- Loss of demarcation between endometrium & myometrium
- Endometrium
- Transition zone (T2)
- Myometrium
- Hazy, irregular T2
General Gynaecology (Presentation)
- Most common: Asymptomatic
- Most common symptom: Heavy menstrual bleeding (HMB)
- Other symptoms:
- Secondary dysmenorrhea
- Subfertility
- Pressure symptoms
- Pain can occur
- Adverse pregnancy outcomes are possible
Cause of HMB
- Increased surface area of endometrium
- Increased vascularity of the uterus (increased estrogen)
- Interference with uterine contractility
- Ulceration of Submucosal fibroid
- Most common fibroid causing HMB: Submucosal fibroid
Cause of Subfertility
- Impaired gamete transport (due to impaired):
- Tubal motility
- Uterine contractility
- Interference with implantation (due to distorted uterine cavity)
- Displacement of the cervix away from the vaginal pool of semen
- Most common fibroid causing subfertility: Submucosal fibroid
Pain
- Usually painless
- If painful: Pelvic pressure/pain
- Acute pain in the abdomen with fibroids:
- Torsion
- Red degeneration of fibroid
Pressure symptoms:
- Urinary: Cervical fibroid
- Rectal: Post cervical fibroid (rare)
Endocrine symptoms:
- Polycythaemia
- Hypercalcemia
- Increased PRL levels
Extra-uterine Fibroids
- These fibroids originate outside of the uterus.
- Cervical Fibroids:
- Anterior Cervical Fibroid: Presses against and irritates the bladder.
- Posterior Cervical Fibroid: Puts pressure on the urethra.
- Broad Ligament (BL) Fibroids:
- True BL Fibroid: Originates from the broad ligament.
- Pseudo BL Fibroid: Arises from the broad ligament.
- Intrauterine Fibroids: Originate from within the uterus.
FIGO Classification of Fibroids
- Subtypes are defined based on their position within the uterine wall. | Subtype | Characteristics | Significance | |---|---|---| | Submucosal | Totally inside uterine cavity; generally pedunculated | Type 0 or Type 1: Removed hysteroscopically; Type 2 or beyond: Removed via laparoscopy | | Intramural | Inside cavity greater than or equal to 50% | | | Subserosal | Inside cavity less than 50% | |
Fibroid (Additional Information)
- The text mentions a diagram, but it is unavailable in this response.
Pseudo Meig's Syndrome
- Pedunculated fibroid
- Right-sided pleural effusion
- Ascites
- Myomectomy
- Spontaneous resolution
Pregnancy Complications
- Pre-term labor
- IUGR (intrauterine growth restriction)
- Abruptio placentae
Degeneration of Fibroid
- Physiology of Degeneration:
- Most vascular part: Periphery
- Least vascular part: Central
- Degeneration begins from the center of the fibroid.
- Hyaline Degeneration:
- Most common degeneration
- Homogenous appearance of fibroid
- Whorled appearance is lost
- Calcareous Degeneration:
- Most common in subserosal fibroids
- Begins from the periphery
- X-Ray: Popcorn calcification/womb stone appearance
- Sarcomatous Degeneration:
- Least common (less than 0.5%)
- Most commonly seen in intramural fibroids
- Mimics: Malignant ovarian tumor
- Not seen in fibroid:
- Amenorrhoea
- Malpresentation
- PPH (Postpartum hemorrhage)
- Subinvolution
General Gynaecology (Specific Degeneration)
- Clinical Presentation:
- Peri/post menopausal female
- Sudden increase in size of fibroid
- Painful fibroid
- Histopathological Examination (HPE):
- Fibroid becomes soft
- Loose pseudocapsule
- 210 mitoses/HPF
Red Degeneration
- Specific to pregnancy
- Commonly seen in mid-pregnancy
- Pathogenesis:
- Thrombosis of blood vessels supplying the fibroid
- Aseptic necrosis of fibroid + Peritoneal irritation
- Clinical Presentation in Pregnancy:
- Pain in the abdomen
- Nausea and vomiting
- Fever (possible)
- Investigations:
- Increased White Blood Cells (WBC)
- Increased Erythrocyte Sedimentation Rate (ESR)
- Management:
- Conservative Management:
- Analgesics
- Antiemetics
- IV fluids
- Medical interventions (NO):
- Antibiotics
- Termination of pregnancy
- Myectomy
- Note on Red Degeneration:
- Caused by thrombosed vessels releasing blood pigments
- Results in a salmon-pink colored fibroid with a fishy odor
Fibroid (Features)
- Benign tumors arising from smooth muscle cells of the uterus.
- Contain varying amounts of fibrous tissue.
- Most common pelvic tumors in females.
Etiopathogenesis
- Estrogen + Progesterone dependent tumors
- Receptors for:
- Estrogen
- Progesterone
- Aromatase
- Apoptosis
- Angiogenic factors: TGF-β, EGF, etc.
- Effect on fibroid:
- Menopause: Regresses
- Oral Contraceptives (OCPs): No effect on the size of the fibroid
- Pregnancy: No effect on the size of the fibroid
- Important Points:
- Most common type of fibroid: Uterine fibroid (Type 4)
- All fibroids begin as intramural fibroids
- Associated with chromosomal anomalies
- Familial predisposition
Classification (Anatomical)
- Uterine:
- Intramural (most common)
- Submucosal
- Subserosal
Comparison of Fibroid, Polyp & Adenomyosis
Fibroid
- AKA Leiomyoma
- Smooth muscle tumor arising from myometrium
- Incidence: Most common in reproductive age (25-35 years). Most common in nulliparous women. (Hyperestrogenic conditions)
- Association: Estrogen + Progesterone dependent tumor
- Symptoms: Heavy menstrual bleeding (HMB), earlier menorrhagia, regular cycles. Secondary dysmenorrhea, infertility, pressure symptoms, pregnancy complications.
Polyp
- Localized outgrowth of endometrium
- Incidence: Seen in all age groups. Increased chance of polyps with age (most common age: 40-49 years).
- Association: Increased incidence in women using Tamoxifen. Reproductive/Perimenopausal age: irregular/intermenstrual bleeding. Post-menopausal: post-menopausal bleeding (PMB). Most common cause of postmenopausal bleeding.
- Symptoms: Menorrhagia (HMB) + secondary dysmenorrhea.
Adenomyosis
- Endometrial tissue (glands + stroma) inside myometrium (at least 2.5 mm deep from basal layer of endometrium).
- Incidence: Women age 40+. Most common in multiparous women.
- Symptoms: Endometriosis and fibroids. Menorrhagia (HMB) + secondary dysmenorrhea. Chronic Pelvic Pain (CPP).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.