Podcast
Questions and Answers
What is the physiological importance of calcium in the body?
What is the physiological importance of calcium in the body?
- Storage of energy in cells
- Nerve impulse transmission and muscle contraction (correct)
- Formation of red blood cells
- Regulation of blood pH
Which hormone acts indirectly to increase calcium absorption in the intestine?
Which hormone acts indirectly to increase calcium absorption in the intestine?
- Parathyroid hormone (correct)
- Vitamin D3
- Thyroid hormone
- Calcitonin
Which of the following conditions is characterized by low levels of parathyroid hormone?
Which of the following conditions is characterized by low levels of parathyroid hormone?
- Thyroid storm
- Hyperparathyroidism
- Hypoparathyroidism (correct)
- Adrenal insufficiency
What is one possible manifestation of hyperparathyroidism?
What is one possible manifestation of hyperparathyroidism?
Tetany can be a clinical feature related to which condition?
Tetany can be a clinical feature related to which condition?
Parathyroid hormone primarily regulates calcium levels in the blood by acting on which organs?
Parathyroid hormone primarily regulates calcium levels in the blood by acting on which organs?
What can cause an inappropriate, excess secretion of parathyroid hormone?
What can cause an inappropriate, excess secretion of parathyroid hormone?
Calcium homeostasis is primarily regulated by which of the following substances?
Calcium homeostasis is primarily regulated by which of the following substances?
What is the primary action of parathyroid hormone (PTH) in relation to calcium homeostasis?
What is the primary action of parathyroid hormone (PTH) in relation to calcium homeostasis?
Which hormone is primarily responsible for decreasing blood calcium levels?
Which hormone is primarily responsible for decreasing blood calcium levels?
What is the primary compensatory mechanism for hypocalcemia in secondary hyperparathyroidism?
What is the primary compensatory mechanism for hypocalcemia in secondary hyperparathyroidism?
What is one of the major functions of calcium in the body?
What is one of the major functions of calcium in the body?
Which of the following manifestations is NOT associated with hyperparathyroidism?
Which of the following manifestations is NOT associated with hyperparathyroidism?
Which of the following conditions may result from hypoparathyroidism?
Which of the following conditions may result from hypoparathyroidism?
What condition is characterized by the contractions of skeletal muscles due to decreased ionized plasma calcium levels?
What condition is characterized by the contractions of skeletal muscles due to decreased ionized plasma calcium levels?
Which of the following accurately describes the overall effect of Vitamin D3 on calcium homeostasis?
Which of the following accurately describes the overall effect of Vitamin D3 on calcium homeostasis?
Which test is NOT indicative of latent tetany?
Which test is NOT indicative of latent tetany?
What is the relationship between calcium levels and parathyroid hormone (PTH) secretion?
What is the relationship between calcium levels and parathyroid hormone (PTH) secretion?
What happens to calcium levels in the blood as a result of hypoparathyroidism?
What happens to calcium levels in the blood as a result of hypoparathyroidism?
Which organ(s) are primarily influenced by calcitonin regarding calcium regulation?
Which organ(s) are primarily influenced by calcitonin regarding calcium regulation?
Which of the following statements about calcium homeostasis is accurate?
Which of the following statements about calcium homeostasis is accurate?
What effect does hyperparathyroidism have on bone density?
What effect does hyperparathyroidism have on bone density?
What is the effect of hyperparathyroidism on bone tissue?
What is the effect of hyperparathyroidism on bone tissue?
What symptom is NOT typically associated with tetany?
What symptom is NOT typically associated with tetany?
Flashcards
Parathyroid Hormone (PTH) function
Parathyroid Hormone (PTH) function
PTH regulates blood calcium levels by increasing calcium in the blood and decreasing phosphate in the blood.
PTH action on bone
PTH action on bone
PTH stimulates osteoclasts, breaking down bone matrix, releasing calcium into the bloodstream.
PTH action on kidney
PTH action on kidney
PTH increases calcium reabsorption and phosphate excretion in the kidneys.
PTH action on intestines
PTH action on intestines
Signup and view all the flashcards
Parathyroid gland location
Parathyroid gland location
Signup and view all the flashcards
Hyperparathyroidism cause
Hyperparathyroidism cause
Signup and view all the flashcards
Calcium homeostasis
Calcium homeostasis
Signup and view all the flashcards
Calcium Homeostasis
Calcium Homeostasis
Signup and view all the flashcards
Calcium in the body
Calcium in the body
Signup and view all the flashcards
Plasma Calcium Level
Plasma Calcium Level
Signup and view all the flashcards
Parathyroid Hormone (PTH)
Parathyroid Hormone (PTH)
Signup and view all the flashcards
Vitamin D3 (1,25(OH)2D3)
Vitamin D3 (1,25(OH)2D3)
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
Bone Resorption
Bone Resorption
Signup and view all the flashcards
Calcium Absorption
Calcium Absorption
Signup and view all the flashcards
Hypercalcemia
Hypercalcemia
Signup and view all the flashcards
Hypocalcemia
Hypocalcemia
Signup and view all the flashcards
Bone Demineralization
Bone Demineralization
Signup and view all the flashcards
Hypercalcuria
Hypercalcuria
Signup and view all the flashcards
Secondary Hyperparathyroidism
Secondary Hyperparathyroidism
Signup and view all the flashcards
Hypocalcemia
Hypocalcemia
Signup and view all the flashcards
Hyperparathyroidism
Hyperparathyroidism
Signup and view all the flashcards
Manifest Tetany
Manifest Tetany
Signup and view all the flashcards
Latent Tetany
Latent Tetany
Signup and view all the flashcards
Trousseau's Sign
Trousseau's Sign
Signup and view all the flashcards
Chvostek's Sign
Chvostek's Sign
Signup and view all the flashcards
Osteitis Fibrosa Cystica
Osteitis Fibrosa Cystica
Signup and view all the flashcards
Renal Stones
Renal Stones
Signup and view all the flashcards
Hypoparathyroidism
Hypoparathyroidism
Signup and view all the flashcards
Study Notes
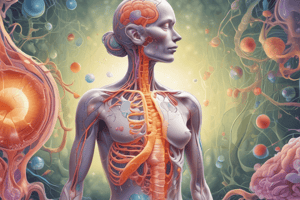
Endocrine Physiology: Parathyroid and Calcium Regulation
- Parathyroid glands are small, bean-shaped glands located on the posterior surface of the thyroid gland. They exist in pairs.
- Parathyroid hormone (PTH) is released from chief cells within the parathyroid glands.
- PTH regulates calcium levels in the blood, a vital function.
- Its main role is to increase plasma calcium levels and decrease plasma phosphate levels.
- PTH works by acting on three target organs: bone, kidney, and intestine.
- On bone, PTH increases bone resorption, releasing calcium from the bone matrix into the blood. Normal levels of PTH affect both osteoblasts and osteoclasts, but high levels only affect osteoclasts.
- On the kidney, PTH increases calcium reabsorption and phosphate excretion.
- On the intestine, PTH indirectly increases calcium absorption through its interaction with vitamin D3.
- Calcium homeostasis is controlled by serum calcium levels.
- There is no higher control of the parathyroid gland from the hypothalamus and pituitary.
- Abnormalities in parathyroid hormone (PTH) secretion can lead to either hyperparathyroidism or hypoparathyroidism.
- Hyperparathyroidism is characterized by excessive PTH secretion, resulting in increased blood calcium levels.
- Causes of primary hyperparathyroidism include parathyroid gland abnormalities (adenomas).
- Causes of secondary hyperparathyroidism include hypocalcemia (e.g., vitamin D3 deficiency or chronic renal failure).
- Hypercalcemia (excess calcium in the blood) can lead to symptoms like stones (kidney stones), bones (bone pain and deformities), and abdominal groans (GI issues).
- Hypoparathyroidism results in low PTH levels, leading to low blood calcium levels.
- Causes include accidental removal of the parathyroid during thyroid surgery.
- Hypocalcemia (low blood calcium) can manifest as tetany, a state of spastic muscle contractions due to increased neuromuscular excitability.
- Manifest tetany usually appears during rest when calcium levels are below 7 mg%.
- It has symptoms like carpopedal spasm, generalized convulsions, laryngeal and respiratory spasm, and suffocation.
- Latent tetany may appear during stress when calcium levels are between 7-9mg%. It can be identified by tests like Trousseau's sign and Chvosteck's test.
- Causes of tetany include decreased calcium intake, hypoparathyroidism, vitamin D3 deficiency, and renal failure.
- Normal blood calcium levels are typically 9-11 mg/dL.
- Vitamin D3 (1,25(OH)2D3) is crucial for maintaining calcium balance; it works on the intestine (increasing calcium absorption), kidneys (increasing calcium reabsorption), and bones (supporting osteoblast activity and bone matrix calcification).
- Vitamin D3 production is initiated by sunlight on the skin.
- Calcitonin is a hormone that decreases calcium levels in the blood. It is produced by parathyroid cells in the thyroid and counteracts the effects of PTH. The effects involve reducing bone resorption by inhibiting osteoclasts, increasing the excretion of calcium by the kidneys, and reducing absorption of calcium in the gut.
Calcium Homeostasis
Calcium (Ca) makes up 1.5% of total body mass, 99% stored in bones.
Plasma calcium levels are 9-11 mg/dL (average 10 mg/dL).
Calcium is in two forms, free/ionized (active) and bound (inactive).
- Calcium metabolism involves intake from the diet, interchange and exchange with bones, and excretion.
- There is a balance in the exchange between the intestine, blood, and kidneys in calcium metabolism to regulate normal levels in the body.
Functions of Calcium
- Calcium is essential for:
- Bone and tooth formation
- Blood clotting
- Neuromuscular function and coupling
- Endocrine function and hormone actions
Hormones Involved in Calcium Homeostasis
- Parathyroid Hormone (PTH): increases blood calcium levels
- Vitamin D3: Increases blood calcium levels
- Calcitonin decreased blood calcium levels
Vitamin D3 (1,25(OH)2D3) Function
Acts on the intestine: promotes calcium absorption from the digestive tract
Acts on the kidneys: increases calcium reabsorption
Acts on bones: promotes osteoblast activity and bone calcification
Calcitonin Function
- Acts on bone to decrease bone resorption
- Acts on kidneys to increase calcium excretion
- Acts on the intestine to decrease calcium absorption.
Calcium Homeostasis Regulation
- The body maintains a balance between PTH, vitamin D3, and calcitonin to monitor calcium in the blood, bones, and gut.
- Blood calcium levels trigger the production or reduction of these hormones.
Assignment: Comparing Hormone Effects
- Students need to compare the ways PTH, Calcitonin, and vitamin D3 impact calcium homeostasis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.