Podcast
Questions and Answers
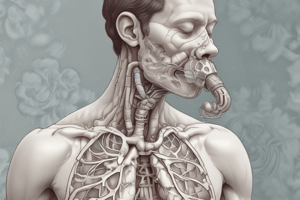
Emphysema is characterized by the destruction of _____. that leads to loss of _____ _____, _____ recoil, and _______ support to maintain airway patency.
Emphysema is characterized by the destruction of _____. that leads to loss of _____ _____, _____ recoil, and _______ support to maintain airway patency.
parenchyma, surface area, elastic, structural
Bronchitis is characterized by _______ of ______ airways by _______ and _______ production.
Bronchitis is characterized by _______ of ______ airways by _______ and _______ production.
narrowing, small, inflammation, mucous
COPD is observed most often in individuals with an extensive history of
COPD is observed most often in individuals with an extensive history of
- smoking (correct)
- exposure to pollutants
- coal mining
- tuberculosis
COPD takes ___ years or longer to mainfest.
COPD takes ___ years or longer to mainfest.
Chronic bronchitis is refers to chronic or recurrent excess mucous secretion occurring on most days for at least ___ months of the year for at least ___ consecutive years.
Chronic bronchitis is refers to chronic or recurrent excess mucous secretion occurring on most days for at least ___ months of the year for at least ___ consecutive years.
Centrilobular emphysema dilation predominantly affects the _______ bronchioles in the _____ lung lobes.
Centrilobular emphysema dilation predominantly affects the _______ bronchioles in the _____ lung lobes.
Panlobular emphysema tissue destruction is _________.
Panlobular emphysema tissue destruction is _________.
Emphysema leads to four primary alterations:
- increase in the size of the ____
- loss of alveolar ______ ______
- mismatch of -__
- increase in ______ _________ workload due to decreased amount of pulmonary capillaries
Emphysema leads to four primary alterations:
- increase in the size of the ____
- loss of alveolar ______ ______
- mismatch of -__
- increase in ______ _________ workload due to decreased amount of pulmonary capillaries
COPD is the ____ leading cause of death and affects more than ___ % of adult Americans.
COPD is the ____ leading cause of death and affects more than ___ % of adult Americans.
In COPD, lung compliance ______ with the tissue damage and the airways' narrowing and collapsibility impede te ability of ventilatory muscles to ____ the lung completely.
In COPD, lung compliance ______ with the tissue damage and the airways' narrowing and collapsibility impede te ability of ventilatory muscles to ____ the lung completely.
In COPD, chronic CO2 retention and hypercapnia, the normal central ventilatory response relies on a ______ in Pa__ to increase ventilation.
In COPD, chronic CO2 retention and hypercapnia, the normal central ventilatory response relies on a ______ in Pa__ to increase ventilation.
Minute ventilation in COPD is generally
Minute ventilation in COPD is generally
Emphysema is caused by damage to elastic fibers because of an imbalance between ______ and ______ in the lung.
Emphysema is caused by damage to elastic fibers because of an imbalance between ______ and ______ in the lung.
Chronic lung hyperinflation results in diaphragmatic _____, and a ______ in contractile force.
Chronic lung hyperinflation results in diaphragmatic _____, and a ______ in contractile force.
_____ intrathoracic pressure is generated during expiration in COPD, which leads to a ______ in systemic venous return.
_____ intrathoracic pressure is generated during expiration in COPD, which leads to a ______ in systemic venous return.
Exaggeration of respiratory variation in arterial blood pressure is called _____ ________
Exaggeration of respiratory variation in arterial blood pressure is called _____ ________
Chronic pressure overload causes right ventricular _______, whereas acute pressure changes causes right ventricular ______.
Chronic pressure overload causes right ventricular _______, whereas acute pressure changes causes right ventricular ______.
Air-containing spaces greater than 1cm in diameter that result from destruction and dilation of air spaces distal to terminal bronchioles.
Air-containing spaces greater than 1cm in diameter that result from destruction and dilation of air spaces distal to terminal bronchioles.
Hallmarks of COPD are
Hallmarks of COPD are
Explain the findings of COPD spirometry: include FEV1, FEV1/FRC, FRC, RV, TLC
Explain the findings of COPD spirometry: include FEV1, FEV1/FRC, FRC, RV, TLC
Match the spirometry to the severity of COPD
Match the spirometry to the severity of COPD
COPD can manifest with impaired gas exchange of oxygen and co2 - PaO2 < __ mmHg, PaCo2 > ___ mmHg
COPD can manifest with impaired gas exchange of oxygen and co2 - PaO2 < __ mmHg, PaCo2 > ___ mmHg
In chronic bronchitis, ____ _____ in the airways impede gas flow.
In chronic bronchitis, ____ _____ in the airways impede gas flow.
In COPD, chronic hypoxia causes _____ _______ _________ to rise and increase work on the ______ ________.
In COPD, chronic hypoxia causes _____ _______ _________ to rise and increase work on the ______ ________.
Current guidelines note that a smoking history of greater than _____ pack-years is the single best variable for predicting airway obstruction.
Current guidelines note that a smoking history of greater than _____ pack-years is the single best variable for predicting airway obstruction.
a1-antitrypsin is produced by the _____ and helps to protect lung tissue from damage by ______ _______.
a1-antitrypsin is produced by the _____ and helps to protect lung tissue from damage by ______ _______.
Smoking can cause an immune-related release of _____ _______. This results in degradation of pulmonary connective tissue.
Smoking can cause an immune-related release of _____ _______. This results in degradation of pulmonary connective tissue.
COPD anesthetic considerations:
- Pre-op: assessment (1) ____ of airflow limitation (2) History of _______(3) _______
- Anesthetic plan: ______ __________ or GA with ______ _______ (to promote bronchodilation)
- Ventilator management: avoid ______, ______, _______; _____ I:E ratio (careful because this can increase PIP)
- Maintain ______ and eliminate _____
COPD anesthetic considerations:
- Pre-op: assessment (1) ____ of airflow limitation (2) History of _______(3) _______
- Anesthetic plan: ______ __________ or GA with ______ _______ (to promote bronchodilation)
- Ventilator management: avoid ______, ______, _______; _____ I:E ratio (careful because this can increase PIP)
- Maintain ______ and eliminate _____
Which of the following is a hallmark sign of COPD?
Which of the following is a hallmark sign of COPD?
A decrease in FEV1 is a dominant feature of COPD.
A decrease in FEV1 is a dominant feature of COPD.
What condition can lead to increased PVR and increased work on the RV in COPD patients?
What condition can lead to increased PVR and increased work on the RV in COPD patients?
The main treatment for COPD includes __________ cessation and bronchodilator therapy.
The main treatment for COPD includes __________ cessation and bronchodilator therapy.
Match the following treatments for COPD with their purpose:
Match the following treatments for COPD with their purpose:
Which gas levels indicate a diagnosis of chronic respiratory failure in COPD?
Which gas levels indicate a diagnosis of chronic respiratory failure in COPD?
Pulmonary rehabilitation is recommended for patients with FEV1 < 50%.
Pulmonary rehabilitation is recommended for patients with FEV1 < 50%.
What intervention is suggested to maintain a PaO2 greater than 60 mmHg in COPD patients?
What intervention is suggested to maintain a PaO2 greater than 60 mmHg in COPD patients?
What is the primary cause of emphysema related to COPD?
What is the primary cause of emphysema related to COPD?
Chronic obstruction in COPD leads to the normal central ventilatory response relying on decreases in PaO2 to increase __________.
Chronic obstruction in COPD leads to the normal central ventilatory response relying on decreases in PaO2 to increase __________.
What is the primary risk factor for developing COPD?
What is the primary risk factor for developing COPD?
Chronic bronchitis is characterized by the permanent destruction of alveolar walls.
Chronic bronchitis is characterized by the permanent destruction of alveolar walls.
What does FEV1 measure?
What does FEV1 measure?
In COPD, a smoking history of greater than _____ pack-years is the best predictor of airway obstruction.
In COPD, a smoking history of greater than _____ pack-years is the best predictor of airway obstruction.
Match the following changes in lung function with their effects on COPD:
Match the following changes in lung function with their effects on COPD:
Which of the following statements is true regarding emphysema?
Which of the following statements is true regarding emphysema?
In COPD patients, the FEV1/FVC ratio is typically greater than 70%.
In COPD patients, the FEV1/FVC ratio is typically greater than 70%.
What is the impact of chronic bronchitis on airway dimensions?
What is the impact of chronic bronchitis on airway dimensions?
COPD is characterized by an inflammatory response in the lungs leading to ________ airflow obstruction.
COPD is characterized by an inflammatory response in the lungs leading to ________ airflow obstruction.
What is one of the clinical consequences of emphysema?
What is one of the clinical consequences of emphysema?
What does the BODE assessment in COPD stand for?
What does the BODE assessment in COPD stand for?
Regional anesthesia is recommended for COPD patients to avoid airway management.
Regional anesthesia is recommended for COPD patients to avoid airway management.
What is the effect of avoiding N2O in patients with COPD?
What is the effect of avoiding N2O in patients with COPD?
In patients with COPD, a lower ______ ratio allows more time for expiration but can increase peak pressure.
In patients with COPD, a lower ______ ratio allows more time for expiration but can increase peak pressure.
Match the following anesthetic considerations with their corresponding details:
Match the following anesthetic considerations with their corresponding details:
What physiological change is primarily caused by chronic microbial colonization in patients with COPD?
What physiological change is primarily caused by chronic microbial colonization in patients with COPD?
How does excess mucus production affect patients with COPD?
How does excess mucus production affect patients with COPD?
What is one consequence of the paralysis of the mucociliary transport system in COPD patients?
What is one consequence of the paralysis of the mucociliary transport system in COPD patients?
What impact does chronic neutrophil influx have on lung tissue in COPD?
What impact does chronic neutrophil influx have on lung tissue in COPD?
What role does increased mucus production play in the progression of COPD?
What role does increased mucus production play in the progression of COPD?
Which of the following is a hallmark feature of obstructive sleep apnea?
Which of the following is a hallmark feature of obstructive sleep apnea?
Obstructive sleep apnea is primarily caused by muscular tension in the airway during sleep.
Obstructive sleep apnea is primarily caused by muscular tension in the airway during sleep.
What primary risk factor contributes to obesity hypoventilation syndrome?
What primary risk factor contributes to obesity hypoventilation syndrome?
The STOP-BANG Questionnaire assesses the risk of sleep apnea by evaluating factors such as snoring, daytime _____, and neck circumference.
The STOP-BANG Questionnaire assesses the risk of sleep apnea by evaluating factors such as snoring, daytime _____, and neck circumference.
What is the recommended definitive diagnostic criterion for obstructive sleep apnea?
What is the recommended definitive diagnostic criterion for obstructive sleep apnea?
Weight loss is an effective treatment for obstructive sleep apnea.
Weight loss is an effective treatment for obstructive sleep apnea.
What does the acronym STOP-BANG stand for in sleep apnea screening?
What does the acronym STOP-BANG stand for in sleep apnea screening?
What intraoperative strategy is advised for patients with obstructive sleep apnea?
What intraoperative strategy is advised for patients with obstructive sleep apnea?
What are the potential complications of obstructive sleep apnea?
What are the potential complications of obstructive sleep apnea?
Obstructive sleep apnea is a mechanical obstruction to breathing caused by the relaxation of _______ ________ during sleep under ______ inspiratory pressure.
Obstructive sleep apnea is a mechanical obstruction to breathing caused by the relaxation of _______ ________ during sleep under ______ inspiratory pressure.
In OSA, chronic _____ and _______ lead to an inflammatory state.
In OSA, chronic _____ and _______ lead to an inflammatory state.
Sleep apnea is also associated with a decreased _____, which contributes to less _____ reserve when OSA patients become apneic.
Sleep apnea is also associated with a decreased _____, which contributes to less _____ reserve when OSA patients become apneic.
Incidence of OSA in obese patients is ____ % and ___% in bariatric surgery patients.
Incidence of OSA in obese patients is ____ % and ___% in bariatric surgery patients.
Chronic _____ and ______ leads to an inflammatory state in OSA.
Chronic _____ and ______ leads to an inflammatory state in OSA.
The inflammatory response in OSA promotes development of the following conditions: _______, ______, ______, _______,
The inflammatory response in OSA promotes development of the following conditions: _______, ______, ______, _______,
OSA decreases _____ and these patients have a decreased _____ reserve.
OSA decreases _____ and these patients have a decreased _____ reserve.
Hallmark sign of OSA includes _______ ________ due to habitual snoring and fragmented sleep.
Hallmark sign of OSA includes _______ ________ due to habitual snoring and fragmented sleep.
Apnea Plus Hypopnea Index (AHI) measures
Apnea Plus Hypopnea Index (AHI) measures
Moderate OSA is an AHI score of > ___
Moderate OSA is an AHI score of > ___
Severe OSA is an AHI score of > ____
Severe OSA is an AHI score of > ____
Preoperative considerations of OSA:
- Bring _____ on day of surgery
- _______ examination
- Anticipate _______ _______
- Mallampati + _______ _________
Preoperative considerations of OSA:
- Bring _____ on day of surgery
- _______ examination
- Anticipate _______ _______
- Mallampati + _______ _________
In OSA patients, the preoperative considerations include considering ______ anesthesia or ________ analgesia to minimize need for medications that produce sedation.
In OSA patients, the preoperative considerations include considering ______ anesthesia or ________ analgesia to minimize need for medications that produce sedation.
During induction in a patient with OSA, anticipate ______ _______, decreased _____, decreased ______ reserve. Have ______ ________ readily available and ______ patient to align ear with sternal notch.
During induction in a patient with OSA, anticipate ______ _______, decreased _____, decreased ______ reserve. Have ______ ________ readily available and ______ patient to align ear with sternal notch.
For emergence in OSA patients, consider _____ _______.
For emergence in OSA patients, consider _____ _______.
What structures are involved in the filtration function of the nose?
What structures are involved in the filtration function of the nose?
What is the primary function of alveoli in the respiratory system?
What is the primary function of alveoli in the respiratory system?
Match the following components of the respiratory system with their respective functions:
Match the following components of the respiratory system with their respective functions:
List the postoperative considerations of OSA:
- Monitor ventilation and oxygenation by _____ and ____ ____
- Consider _____ in PACU
- Consider prolonged monitoring (-_ hours)
List the postoperative considerations of OSA:
- Monitor ventilation and oxygenation by _____ and ____ ____
- Consider _____ in PACU
- Consider prolonged monitoring (-_ hours)
Preoperative considerations for patients with COPD:
- Assess _____, ______ of airflow limitation, history of _______, and _________.
- Consider _______ anesthesia
Preoperative considerations for patients with COPD:
- Assess _____, ______ of airflow limitation, history of _______, and _________.
- Consider _______ anesthesia
Anesthetic management for COPD patient includes:
- _____ anesthetics promote ________
- Consider ______ of inspired gas
- Ventilation: maintain ______ and eliminate ____
4.Avoid _____ (high inspiratory pressure), _______, and _____ (secondary to high Vt or auto-PEEP)
Anesthetic management for COPD patient includes:
- _____ anesthetics promote ________
- Consider ______ of inspired gas
- Ventilation: maintain ______ and eliminate ____ 4.Avoid _____ (high inspiratory pressure), _______, and _____ (secondary to high Vt or auto-PEEP)
Postoperative considerations for COPD patient:
- ______ _______ and incentive spirometer
- Prolonged ______ _________
Postoperative considerations for COPD patient:
- ______ _______ and incentive spirometer
- Prolonged ______ _________
ARDs has a ____% mortality rate.
ARDs has a ____% mortality rate.
Asthma is characterized by chronic inflammation of the respiratory tract and widespread propagation of inflammatory _____
Asthma is characterized by chronic inflammation of the respiratory tract and widespread propagation of inflammatory _____
The presence of antigens provokes T-lymphocytes to generate an _____-mediated response.
The presence of antigens provokes T-lymphocytes to generate an _____-mediated response.
Clinical manifestations of asthma include recurrent wheezing, breathlessness, chest _____, and fatigue.
Clinical manifestations of asthma include recurrent wheezing, breathlessness, chest _____, and fatigue.
Exercise-induced asthma may be related to high minute ventilation or low temperature/humidity of inspired _____
Exercise-induced asthma may be related to high minute ventilation or low temperature/humidity of inspired _____
Aspirin-induced asthma occurs in predisposed individuals as a result of cyclooxygenase inhibition that drives arachidonic acid metabolism toward the _____ pathway.
Aspirin-induced asthma occurs in predisposed individuals as a result of cyclooxygenase inhibition that drives arachidonic acid metabolism toward the _____ pathway.
Status Asthmaticus is characterized by airflow obstruction that is refractory to _____ therapy.
Status Asthmaticus is characterized by airflow obstruction that is refractory to _____ therapy.
Infection-induced asthma is secondary to acute inflammation due to viral, bacterial, or _____ infection.
Infection-induced asthma is secondary to acute inflammation due to viral, bacterial, or _____ infection.
The mechanisms of non-immunologic asthma are less clearly defined but can be triggered by irritants such as cold air or _____ irritants.
The mechanisms of non-immunologic asthma are less clearly defined but can be triggered by irritants such as cold air or _____ irritants.
Poorly controlled asthma is defined by frequent rescue inhaler use or ED visit within _____ days.
Poorly controlled asthma is defined by frequent rescue inhaler use or ED visit within _____ days.
Bronchoconstriction, a key feature of asthma, can lead to increased airway _____ and mucous secretion.
Bronchoconstriction, a key feature of asthma, can lead to increased airway _____ and mucous secretion.
In asthma, the presence of antigens provoke T-lymphocytes to generate an ______-mediated response.
In asthma, the presence of antigens provoke T-lymphocytes to generate an ______-mediated response.
One of the clinical features of asthma is bronchoconstriction, which is an _____________ of the airways.
One of the clinical features of asthma is bronchoconstriction, which is an _____________ of the airways.
The hallmark signs of asthma include recurrent wheezing, dyspnea, cough, and prolonged ________ phase.
The hallmark signs of asthma include recurrent wheezing, dyspnea, cough, and prolonged ________ phase.
During exacerbations of asthma, FEF (25-75%) is decreased, indicating ________ obstruction.
During exacerbations of asthma, FEF (25-75%) is decreased, indicating ________ obstruction.
Treatment for asthma may include short-acting B2 agonists and inhaled ________.
Treatment for asthma may include short-acting B2 agonists and inhaled ________.
Complications of chronic asthma may lead to irreversible lung destruction and ________ hypertension.
Complications of chronic asthma may lead to irreversible lung destruction and ________ hypertension.
Peak expiratory flow values below ______% of expected indicate a severe episode of bronchoconstriction.
Peak expiratory flow values below ______% of expected indicate a severe episode of bronchoconstriction.
Symptoms of asthma often worsen with exercise, viral infections, or ________ allergens.
Symptoms of asthma often worsen with exercise, viral infections, or ________ allergens.
Asthma is characterized by recurrent wheezing, dyspnea, and ________.
Asthma is characterized by recurrent wheezing, dyspnea, and ________.
In asthma, symptoms often worsen with exercise and ________ infections.
In asthma, symptoms often worsen with exercise and ________ infections.
Treatment for asthma may include short-acting B2 agonists and ________ corticosteroids.
Treatment for asthma may include short-acting B2 agonists and ________ corticosteroids.
During an exacerbation, the FEV1:FVC ratio is ________.
During an exacerbation, the FEV1:FVC ratio is ________.
Mechanical ventilation for asthma patients should avoid ________ to prevent complications.
Mechanical ventilation for asthma patients should avoid ________ to prevent complications.
Ketamine is considered beneficial for patients experiencing an active asthmatic ________.
Ketamine is considered beneficial for patients experiencing an active asthmatic ________.
Oral glucocorticoids should be administered postoperatively in patients who have used ________ corticosteroids recently.
Oral glucocorticoids should be administered postoperatively in patients who have used ________ corticosteroids recently.
A hallmark of asthma is prolonged ________ phase during respiration.
A hallmark of asthma is prolonged ________ phase during respiration.
Chronic asthma may lead to complications such as pulmonary ________ and lung hyperinflation.
Chronic asthma may lead to complications such as pulmonary ________ and lung hyperinflation.
Patients with significant respiratory symptoms should have ________ procedures postponed.
Patients with significant respiratory symptoms should have ________ procedures postponed.
Consider deep extubation to avoid mechanical stimulation from _____ if awake extubation is used.
Consider deep extubation to avoid mechanical stimulation from _____ if awake extubation is used.
B-blockers can cause _____, so esmolol is preferred due to its B1 selectivity.
B-blockers can cause _____, so esmolol is preferred due to its B1 selectivity.
For intra-op bronchospasm, one should deepen sedation with volatile anesthetics or administer a _____ like albuterol.
For intra-op bronchospasm, one should deepen sedation with volatile anesthetics or administer a _____ like albuterol.
In asthma and pregnant patients, Budesonide is the preferred _____ agent.
In asthma and pregnant patients, Budesonide is the preferred _____ agent.
Audible wheezing is one manifestation of intra-op _____ episodes.
Audible wheezing is one manifestation of intra-op _____ episodes.
Prostaglandins like Hemabate can reduce uterine bleeding but cause _____ in asthmatic patients.
Prostaglandins like Hemabate can reduce uterine bleeding but cause _____ in asthmatic patients.
One should avoid long-acting muscle relaxants due to the risk of residual muscle _____ in patients.
One should avoid long-acting muscle relaxants due to the risk of residual muscle _____ in patients.
In patients experiencing bronchospasm, a decrease in FRC, ERV, and ability to cough can occur if spinal or epidural levels are to the _____ area or higher.
In patients experiencing bronchospasm, a decrease in FRC, ERV, and ability to cough can occur if spinal or epidural levels are to the _____ area or higher.
Intra-op bronchospasm can result in manifestations such as wheezing, increased mucus secretion, and _____ on pulse oximetry.
Intra-op bronchospasm can result in manifestations such as wheezing, increased mucus secretion, and _____ on pulse oximetry.
Consider using aminophylline if long-term postoperative _____ is planned.
Consider using aminophylline if long-term postoperative _____ is planned.
Flashcards are hidden until you start studying
Study Notes
COPD Anesthetic Considerations
- COPD severity and treatments:
- Identify severity.
- Implement treatments to reduce inflammation, improve secretion clearance, treat underlying infections, and increase airway caliber.
BODE Index
- A tool for assessing COPD severity.
- It includes Body Mass Index (BMI), Obstruction of airflow, Dyspnea, and Exercise capacity
Anesthetic Assessment
- Includes symptoms, severity of airflow limitation, history of exacerbations, and co-morbidities
COPD Anesthesia Considerations
- Avoid drastic reductions in PaCO2:
- Rapid decreases in PaCO2 can lead to respiratory distress and worsen symptoms.
- Regional anesthesia is recommended:
- Avoids airway management and mechanical ventilation, especially in patients with severe COPD.
- However, neuraxial anesthesia above T6 is not recommended
- Decreases expiratory reserve volume.
- Impairs coughing effort.
- May create anxiety-provoking weakness.
- General anesthesia:
- Use volatile anesthetics to facilitate bronchodilation.
- Humidification is essential to maintain airway moisture.
- Opioids:
- Can be used with caution.
- Cause less V/Q mismatch compared to other sedatives
- Respiratory depressant effects need to be considered, especially in the elderly.
- N2O should be avoided:
- Can enlarge and rupture bullae (air pockets in the lung).
- Ventilator Management:
- Maintain adequate oxygenation.
- ** Eliminate CO2.**
- Avoid barotrauma (high peak inspiratory pressures).
- Avoid alveolar injury (atelectasis).
- Avoid volutrauma from excessive tidal volume (Vt) or auto-PEEP.
- Lower I:E ratio (inspiratory: expiratory time ratio):
- Allows more time for expiration.
- Increases peak pressure.
- Postoperative Care:
- Pulmonary toilet (techniques to clear airways)
- Incentive spirometry (deep breathing exercises)
COPD Defense System Disruption
- Excess mucus production and mucociliary transport system paralysis in COPD patients create an environment for microbial colonization.
- Chronic colonization leads to a vicious cycle, increasing mucus production, reducing ciliary motility, and causing an influx of neutrophils.
- This influx of neutrophils contributes to fibrosis, further impairing the respiratory system.
Obstructive Sleep Apnea (OSA)
- OSA is caused by relaxation of pharyngeal muscles during sleep leading to mechanical obstruction of the airway.
- OSA involves chronic hypoxia and hypoxemia which trigger inflammation.
- OSA is also associated with reduced Functional Residual Capacity (FRC), decreasing oxygen reserves during apneic periods.
- The OSA cycle involves alveolar hypoventilation, hypoxia, sympathetic nervous system (SNS) stimulation, vasoconstriction, increased Systemic Vascular Resistance (SVR), and ultimately, hypertension.
Obesity Hypoventilation Syndrome (OHS)
- OHS is characterized by a triad of obesity, daytime hypoventilation, and sleep-disordered breathing.
- OSA is marked by episodes of breathing cessation lasting 10 seconds or more.
- OSA significantly increases morbidity and mortality in hospitalized patients.
- Obesity is the primary risk factor for OSA, with 40% of obese individuals and 80% of bariatric surgery patients experiencing OSA.
- Redundant neck tissue is a common consequence of obesity and contributes to OSA.
- Snoring and fragmented sleep are hallmark features of OSA, often accompanied by daytime somnolence.
STOP-BANG Questionnaire
- The STOP-BANG questionnaire has a high sensitivity (100%) but lower specificity (40%).
- Snoring loudly
- Tiredness during the day
- Observed cessation of breathing or choking/gasping during sleep
- Pressure, high blood pressure
- BMI > 35 kg/m2
- Age > 50 years
- Neck circumference > 40 cm or 17 inches
- Gender – male (24% incidence in men)
OSA Diagnosis
- Polysomnography is used to diagnose OSA.
- An Apnea-Hypopnea Index (AHI) of > 5 with associated sleep symptoms or > 15 without symptoms confirms the diagnosis.
- Mild OSA: AHI > 15
- Severe OSA: AHI > 30
OSA Treatment
- Weight loss is crucial for OSA management.
- Continuous Positive Airway Pressure (CPAP) is a common treatment modality, but adherence rates are only around 50%.
OSA Complications
- Hypertension
- Pulmonary hypertension (PAH) due to hypoxemia causing pulmonary vasoconstriction and increased pulmonary vascular resistance (PVR).
- Congestive heart failure (CHF)/Right heart failure (RHF)
- Ischemic heart disease
Anesthesia Considerations in OSA Patients
- Airway: Anticipate airway difficulty and rapid desaturation due to reduced FRC.
- Have airway adjuncts readily available.
- Positioning: Ramp upper body for intubation; hyperoxygenate before intubation.
- Intraoperative: Regional anesthesia is preferred when possible. For general anesthesia (GA), use short-acting agents. Limit long-acting opioids and minimize muscle relaxants; provide positive end-expiratory pressure (PEEP).
- Postoperative: Extubate when fully awake and elevate the upper body. Vigilant monitoring is essential during extubation, as 25% of pediatric OSA patients after tonsillectomy are at risk for airway obstruction.
- Use multimodal and non-opioid analgesia to minimize systemic opioid use.
- CPAP in recovery is recommended.
- Analgesics and general somnolence can lead to airway obstruction in the Post-Anesthesia Care Unit (PACU).
- Discharge: Patients can be discharged on the same day if they undergo minor surgery with regional anesthesia or sedation and minimal opioid use.
- Major surgery, significant opioid needs, severe OSA, or home CPAP require overnight monitoring with spo2 monitoring.
### Respiratory System Functions
- The respiratory system functions to take in oxygen and expel carbon dioxide.
- Respiration is the process of gas exchange, it is crucial for cellular energy production.
Components of Respiration
- Respiration involves anatomical structures from the upper airway to the alveoli.
- The upper airway includes the nose, pharynx, and larynx.
- The lower airway includes the trachea, bronchi, bronchioles, alveolar ducts, and alveoli.
Nose Structures
- The nose has alae nasae, anterior nares, nasal vestibules, nasal fossae, and nasal septum.
- The nasal septum is composed of the vomer bone and septal cartilages.
- Three nasal conchae help filter air.
- The nasal fossae connect to the nasopharynx via the nasal choanae.
- Paranasal sinuses include the maxillary, frontal, ethmoid, and sphenoid sinuses.
Nose Neurovascular Structures
- The nose is supplied by arteries, veins, and lymphatics.
- It is innervated by cranial nerves for sensory functions.
Nose Functions
- The nose warms, humidifies, filters, and detects odors in the air.
Pharynx
- The pharynx is a muscular tube extending from the skull base to the esophagus.
- Tonsils are lymphoid tissue aggregations in the pharynx.
Larynx Structures
- The larynx is located between C3-C6, preventing aspiration during swallowing.
- Vestibular folds are fibrous tissue covered in mucous membranes superior to the true vocal cords.
- True vocal cords are fibrous folds between the thyroid and arytenoid cartilages.
- The larynx has nine cartilages, ligaments, muscles, and membranes.
Larynx Musculature
- The larynx contains intrinsic muscles that move the vocal cords, controlling sound production.
Cormack-Lehane Classification
- This classification describes visualization of laryngeal structures during intubation with grades 1-4.
- Grade 1: Full view of the laryngeal inlet.
- Grade 2a: Partial view of vocal cords.
- Grade 2b: View of posterior vocal cords or arytenoids.
- Grade 3: View of only the epiglottis.
- Grade 4: No visible laryngeal structures.
Larynx Neurovascular Structures
- The larynx receives arterial blood supply and venous drainage.
- It is innervated by the superior laryngeal and recurrent laryngeal (RLN) nerves, both branches of the vagus nerve.
- Superior laryngeal nerve: internal branch provides sensory innervation above the vocal cords, and the external branch controls cricothyroid muscles.
- Recurrent laryngeal nerve: controls all intrinsic laryngeal muscles except cricothyroid and interarytenoid muscles, and provides sensory innervation below the vocal cords.
Trachea
- The trachea is a protective structure composed of hyaline cartilage rings which prevents airway collapse.
- It extends from the inferior larynx to the carina where it divides into the bronchi.
- The trachea receives arterial blood supply, has venous drainage, and is innervated by branches of the vagus nerve.
Bronchi Neurovascular Structures
- The bronchi are supplied by arteries and veins.
- They receive both sympathetic and parasympathetic innervation.
- Sympathetic stimulation causes bronchodilation, while parasympathetic stimulation causes bronchoconstriction.
- Histamine and anaphylaxis also cause bronchoconstriction.
Respiratory Zone
- The respiratory zone, where gas exchange occurs, includes respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli.
Alveoli
- Alveoli are the primary sites of gas exchange within the lungs.
Pulmonary Hilum
- This is the conduit to the lung, containing the main bronchus, pulmonary and bronchial circulations, lymphatics, lymph nodes, and pulmonary nerves.
Thoracic Cavity
- The thoracic cavity houses the left pleural cavity, mediastinum, and right pleural cavity.
- The pleura are serous membranes that separate the lungs from the thoracic cage and mediastinum.
- Parietal pleura lines the chest wall, mediastinum, and diaphragm.
- Visceral pleura lines the lungs.
Mechanics of Breathing
- The diaphragm is the primary muscle of inspiration, separating the thoracic and abdominal cavities.
- Inspiration: contraction of the diaphragm flattens it, increasing the volume of the thoracic cavity and causing air to flow into the lungs.
- Expiration: relaxation of the diaphragm, along with the elastic recoil of lung tissue, decreases the volume of the thoracic cavity, forcing air out of the lungs.
Boyle's Law
- This law describes the inverse relationship between pressure and volume: P₁V₁ = P₂V₂
- During inspiration, the volume of the thoracic cavity increases, causing a decrease in alveolar pressure, drawing air into the lungs.
- During expiration, the volume of the thoracic cavity decreases, causing an increase in alveolar pressure, forcing air out of the lungs.
Pleural, Alveolar, and Transpulmonary Pressures
- Pleural pressure (Ppl): pressure within the pleural space, always negative relative to alveolar pressure.
- Alveolar pressure (Palv): pressure within the alveoli.
- Transpulmonary pressure: pressure difference between alveolar and pleural pressures, responsible for keeping alveoli open (Palv - Ppl).
Lung Compliance
- Compliance is the flexibility of the lungs, or how easily they expand in response to pressure changes.
- It is influenced by elastic forces of lung tissue (collagen, elastin), and alveolar surface tension.
- Compliance is calculated as the change in lung volume (ΔV) divided by the change in pressure (ΔP) (C=ΔV/ΔP).
Lung Volumes & Capacities
- Tidal Volume (TV): volume of air inhaled or exhaled during normal breathing.
- Inspiratory Reserve Volume (IRV): additional volume of air that can be inhaled beyond a normal tidal inhalation.
- Expiratory Reserve Volume (ERV): additional volume of air that can be exhaled beyond a normal tidal exhalation.
- Residual Volume (RV): volume of air remaining in the lungs after a forceful exhalation.
- Inspiratory Capacity (IC): total volume of air that can be inhaled from the normal expiratory level (TV + IRV).
- Functional Residual Capacity (FRC): volume of air remaining in the lungs at the end of a normal exhalation (ERV + RV).
- Vital Capacity (VC): maximum volume of air that can be exhaled after a maximum inhalation (TV + IRV + ERV).
- Total Lung Capacity (TLC): maximum volume of air that the lungs can hold (TV + IRV + ERV + RV).
Helium Dilution Method
- This method is used to measure lung volumes and capacities that cannot be measured directly using spirometry, like FRC, RV, and TLC.
- A known volume of air/helium mixture is inhaled, causing dilution of the helium concentration, which can be used to calculate the unknown lung volumes.
Minute Ventilation
- This is the total volume of air moved in and out of the lungs per minute (Minute Ventilation = Tidal Volume x Respiratory Rate).
Dead Space
- Dead space includes areas of the lungs that receive ventilation but not enough perfusion for effective gas exchange.
- Alveolar ventilation is the volume of air available for gas exchange per minute (Alveolar Ventilation = Respiratory Rate x (Tidal Volume - Dead space)).
Pulmonary Circulation
- Pulmonary circulation carries deoxygenated blood from the heart to the lungs for oxygenation and then returns oxygenated blood to the heart.
- Bronchial circulation is a separate circulatory system that supplies oxygen to the tissues of the bronchi and bronchioles.
Ventilation/Perfusion Ratio (V/Q)
- This ratio describes the distribution of ventilation (airflow) relative to perfusion (bloodflow).
- V/Q varies in different regions of the lungs.
- Ideal: When ventilation and perfusion are matched (V/Q = 1).
- Dead space: Ventilation without perfusion (V/Q = ∞).
- Shunt: Perfusion without ventilation (V/Q = 0).
Dalton's Law of Partial Pressures
- This law states that the total pressure of a gas mixture is the sum of the partial pressures of each gas in the mixture.
- Partial pressures of gases in the atmosphere change with altitude.
- Water vapor also contributes to the total pressure in the alveoli.
Alveolar Gas Equation
- This equation calculates the partial pressure of oxygen in the alveoli (PAO2) considering the partial pressure of inspired oxygen (PIO2), partial pressure of carbon dioxide in the alveoli (PACO2), and the respiratory quotient (RQ).
Fick's Law of Diffusion
- This law describes the diffusion of gases across the alveolocapillary membrane.
- Diffusion rate is directly proportional to: surface area (A), diffusion coefficient (D), and the pressure difference (P1-P2).
- Diffusion rate is inversely proportional to the thickness (T) of the diffusion barrier.
Oxygen Transport
- Oxygen is transported in the blood by physical dissolution in plasma (0.3%) and bound to hemoglobin (99.7%).
Oxyhemoglobin Dissociation Curve
- This curve shows the relationship between the partial pressure of oxygen and the saturation of hemoglobin with oxygen.
- Rightward shift: enhances oxygen release from hemoglobin (increased H+^ , CO2, temperature, and 2,3-BPG).
- Leftward shift: reduces oxygen release from hemoglobin (decreased H+^ , CO2, temperature, and 2,3-BPG, methemoglobin, carbon monoxide).
Carbon Dioxide Transport
- Carbon dioxide is transported in the blood through: physical dissolution in plasma (5-10%), carbamino compounds (5-10%), and bicarbonate (80-90%).
- Bicarbonate formation is catalyzed by carbonic anhydrase within red blood cells.
- The chloride shift maintains equilibrium as bicarbonate diffuses out of red blood cells and chloride diffuses in.
- H+^ is buffered by binding to hemoglobin within the red blood cells.
Bohr & Haldane Effects
- Bohr Effect: CO2/H+^ affect hemoglobin's affinity for O2.
- Haldane Effect: O2 affects hemoglobin's affinity for CO2/H+^.
Control of Breathing
- The respiratory system primarily functions to maintain homeostatic levels of O2, CO2, and H+^ in the body.
Medullary Respiratory Center
- This center in the medulla oblongata controls the basic rhythm of breathing.
- It receives afferent signals from the glossopharyngeal and vagus nerves.
- The medullary respiratory center includes the dorsal and ventral respiratory groups.
Central Chemoreceptors
- These receptors are located in the medulla, sensitive to changes in CSF pH.
- They are not directly exposed to blood, but CO2 can diffuse across the blood-brain barrier and affect CSF pH.
Peripheral Chemoreceptors
- These receptors are located in the carotid bodies and aortic bodies, sensitive to changes in arterial blood O2, CO2, and H+ levels.
Hering-Breuer Reflex
- Lung stretch receptors inhibit inspiration when tidal volumes exceed 1500 mL, preventing lung overinflation.
Cough and Sneeze Reflexes
- Cough: irritation of the airway, triggered via vagus nerve, expels irritants from the trachea and bronchi.
- Sneeze: irritation of the nasal passages, triggered by the trigeminal nerve, expels irritants from the nose.
Acid-Base Balance
- The respiratory system plays a key role in acid-base balance along with the kidneys and buffers.
- The respiratory system regulates CO2 levels in the body, which influences blood pH.
Arterial Blood Gas Interpretation
- Arterial blood gas analysis measures blood pH, partial pressures of O2 (PaO2) and CO2 (PaCO2), and bicarbonate levels.
- These measurements help identify acid-base disturbances and respiratory/metabolic conditions.
Asthma Pathophysiology
-
Allergic (Atopic) Asthma:
- Chronic inflammation of the respiratory tract
- Inflammatory mediators: eosinophils, mast cells, neutrophils, macrophages
- Antigens trigger T-lymphocytes, leading to IgE production
- Results in:
- Vasoconstriction
- Increased smooth muscle tone
- Enhanced mucous secretion
- Submucosal edema
- Increased vascular permeability
- Inflammatory cell chemotaxis
-
Non-Immunologic Asthma:
- Less clear mechanisms
- Triggers include:
- Cold air
- Airway instrumentation or irritation
- Inhaled irritants
- Abnormal leukotriene production
- Climate changes
- Upper respiratory illnesses
Clinical Features of Asthma
- Bronchoconstriction: Narrowing of airways
- Airway Hyperresponsiveness: Exaggerated response to stimuli
- Mucous Secretion: Increased glycoprotein mucin production
- Airway Edema: Swelling of airway lining
Types of Asthma
-
Exercise-Induced Asthma:
- May be related to high minute ventilation or low temperature/humidity of inspired gas
-
Occupational Asthma:
- Inhaled irritants stimulate vagal nerve endings in the airway epithelium
-
Infection-Induced Asthma:
- Secondary to acute inflammation caused by viral, bacterial, or mycoplasma infections
-
Aspirin-Induced Asthma:
- Occurs in individuals with predisposition due to cyclooxygenase inhibition
- Drives arachidonic acid metabolism towards the lipoxygenase pathway, increasing leukotriene production
Asthma Susceptibility Factors
- Deficiency of acquired immunity
- Genetics
- Exposure to respiratory irritants
Clinical Manifestations
- Recurrent wheezing
- Breathlessness
- Chest tightness
- Fatigue
Asthma Exacerbations
- Short-lived attacks lasting minutes to hours
- Severity determined by time between attacks
Status Asthmaticus
- Airflow obstruction unresponsive to bronchodilator therapy
Poorly Controlled Asthma
- Frequent rescue inhaler use or emergency department visits within 30 days
- Associated with increased respiratory complications, affecting length of stay, surgical risk, and in-hospital mortality
Airflow Changes in Asthma
- Bronchoconstriction
- Airway hyperresponsiveness
- Mucous secretion
- Airway edema
Asthma Pathophysiology
-
Allergic (Atopic) Asthma:
- Chronic inflammation of the respiratory tract
- Antigens stimulate T-lymphocytes leading to IgE production
- Increased eosinophils, mast cells, neutrophils, and macrophages
- This response causes vasoconstriction, increased smooth muscle tone, mucus secretion, edema, increased vascular permeability, and inflammatory cell chemotaxis
-
Non-Immunologic Asthma:
- Less defined mechanisms
- Triggers: cold air, airway instrumentation, inhaled irritants, leukotriene production, climate changes, or respiratory illness
Asthma Clinical Features
- Bronchoconstriction: narrowing of the airways
- Airway Hyperresponsiveness: exaggerated bronchoconstriction response to stimuli
- Mucous Secretion: hypersecretion of mucin
- Airway Edema: swelling of the airway
Asthma Subtypes
- Exercise-Induced: high minute ventilation or low temperature/humidity
- Occupational: inhaled irritants stimulating the vagal nerve ending
- Infection-Induced: viral, bacterial, or mycoplasma infection
- Aspirin-Induced: cyclooxygenase inhibition leading to increased leukotriene production
Asthma Susceptibility
- Deficient acquired immunity
- Genetic predisposition
- Exposure to respiratory irritants
Asthma Clinical Manifestations
- Recurrent wheezing
- Breathlessness
- Chest tightness
- Fatigue
Asthma Exacerbations
- Short-lived attacks (minutes to hours)
- Severity determined by time between attacks
Status Asthmaticus
- Airflow obstruction unresponsive to bronchodilators
Poorly Controlled Asthma
- Frequent rescue inhaler use or ER visits within 30 days
- Increased respiratory complications, affecting length of stay, surgical risk, and in-hospital mortality
Airflow Changes in Asthma
- Bronchoconstriction: airway narrowing
- Airway Hyperresponsiveness: exaggerated bronchoconstriction response
- Mucous Secretion: increased mucin production
- Airway Edema: airway swelling
Asthma Hallmarks
- Recurrent wheezing, shortness of breath, coughing
- Labored breathing with accessory muscle use
- Rapid breathing
- Chest tightness
- Prolonged exhalation
- Fatigue
- Symptoms worsen during exercise, viral infections, exposure to allergens, weather changes, stress, or menstrual cycles
Asthma Diagnosis
- During exacerbations, forced expiratory flow (FEF25-75%) and forced expiratory volume in one second (FEV1) are decreased
- Decreased FEV1/forced vital capacity (FVC) ratio suggests airflow obstruction
- Gas exchange abnormalities lead to ventilation/perfusion (V/Q) mismatch, causing hypoxia
- Peak expiratory flow (PEF) values 30-50% below expected indicate moderate bronchoconstriction
- PEF values below 50% of normal indicate severe bronchoconstriction
Asthma Treatment
- Short-acting beta2 agonists
- Inhaled corticosteroids
- Oral glucocorticoids
- Long-acting beta2 agonists (LABAs)
- Leukotriene modifiers
- Anti-immunoglobulin E (IgE) antibody
- Theophylline
- Anti-interleukin-5 (IL-5) antibodies
Asthma Complications
- Chronic asthma may lead to irreversible lung damage
- Loss of lung elasticity
- Pulmonary hypertension
- Lung hyperinflation
Asthma Hallmarks
- Recurring wheezing, shortness of breath, cough, labored breathing, rapid breathing, chest tightness, prolonged exhalation, fatigue.
- Symptoms worsen with exercise, viral infections, allergens, weather changes, stress, or menstruation.
Asthma Diagnosis
- During exacerbations, forced expiratory flow (FEF 25-75%) is decreased and decreased FEV1:FVC ratio.
- Airflow obstruction and gas exchange abnormalities lead to a ventilation-perfusion mismatch, causing hypoxemia.
- Peak expiratory flow (PEF) values 30-50% below expected indicate moderate bronchoconstriction.
- PEF below 50% of normal indicates a severe episode.
Asthma Treatment
- Short-acting beta-2 agonists (SABAs)
- Inhaled corticosteroids (ICSs)
- Oral glucocorticoids
- Long-acting beta-2 agonists (LABAs)
- Leukotriene modifiers
- Anti-IgE antibody
- Theophylline
- Anti-interleukin-5 (IL-5) antibodies
Asthma Complications
- Chronic asthma can lead to irreversible lung damage, loss of lung elasticity, pulmonary hypertension, and lung hyperinflation.
Asthma Anesthetic Considerations
-
Pre-operative
- Review asthma control level, including medication use, especially oral corticosteroids within the past 6 months.
- For patients receiving oral systemic corticosteroids in the 6 months prior to surgery, administer 100mg hydrocortisone intravenously every 8 hours during the surgical period.
- Reduce the dose quickly within 24 hours after surgery.
- Complications of steroid use include delayed wound healing, infection, and adrenocortical insufficiency.
- Postpone elective procedures in patients with significant respiratory symptoms.
-
Increased likelihood of intra-operative difficulties:
- Frequent nocturnal awakenings.
- Recent increases in medication usage.
- Signs of viral infection.
-
Induction:
- Avoid endotracheal intubation if possible because it can cause bronchospasm.
- Consider a supraglottic airway or administer SABA 20-30 minutes before airway manipulation.
- Ketamine offers bronchodilation and is best for active asthmatic episodes or emergency surgeries.
- Avoid ketamine in patients who have recently taken theophylline due to a risk of seizure activity.
-
Maintenance:
- Inhalation agents like isoflurane and desflurane can irritate the airway.
- This effect can be reduced with opioids.
- Sevoflurane is the least irritating volatile anesthetic.
-
Mechanical ventilation:
- Avoid hyperinflation and barotrauma.
- Allow for longer expiratory times and moderate permissive hypercapnia.
-
Emergence:
- Consider deep extubation to avoid mechanical stimulation from the endotracheal tube.
- If awake extubation is necessary, use opioids to reduce airway irritability.
- Consider sugammadex. Anticholinesterase reversal agents can worsen bronchospasm.
-
Avoid:
- Atracurium, mivacurium, and morphine due to histamine release.
- Beta-blockers as they can cause bronchoconstriction.
- Esmolol is a good alternative due to its beta-1 selectivity and short half-life.
- Prostaglandins like the F2a subtype (Hemabate), ergonovine, and ergot derivatives, as they can trigger bronchospasm.
- Long-acting muscle relaxants due to potential residual muscle weakness.
- Ketorolac and other NSAIDs in patients with aspirin-induced asthma.
- Spinal or epidural anesthesia to midthoracic levels or higher can decrease functional residual capacity (FRC), expiratory reserve volume (ERV), and the ability to cough.
- H2-receptor antagonists.
-
Intra-operative bronchospasm:
- Manifested by wheezing, increased mucus secretion, high inspiratory pressures, slanted expiratory carbon dioxide waveform, and hypoxemia.
- Treatment:
- Deepen sedation with volatile anesthetics, propofol, or ketamine.
- Administer 100% oxygen.
- Administer a SABA (albuterol).
- Give epinephrine intravenously or subcutaneously (10 mcg/kg).
- Consider inhaled corticosteroids (2-4 mg/kg).
- Administer aminophylline if long-term post-operative ventilation is planned.
-
Asthma + Pregnant Surgical Patient:
- Albuterol is the preferred SABA.
- Budesonide is the preferred ICS.
- Beta-agonists cause bronchodilation and relax the uterus, which can impede labor progression and enhance postpartum bleeding.
- Prostaglandins (Hemabate) reduce uterine bleeding but induce bronchoconstriction.
-
Bronchospasm signs:
- Increased peak inspiratory pressure (PIP).
- Hypoxemia evident on pulse oximetry.
- Audible wheezing.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.