Podcast
Questions and Answers
What is a potential complication of hypernatremia due to increased serum sodium levels?
What is a potential complication of hypernatremia due to increased serum sodium levels?
- Excessive water intake
- Decreased osmolality of the blood
- Increased fluid retention in the interstitial space
- Cellular dehydration (correct)
Which of the following is NOT a clinical feature associated with hypernatremia?
Which of the following is NOT a clinical feature associated with hypernatremia?
- Thirst
- Altered mental status
- Fatigue
- Muscle spasms (correct)
What management strategy is recommended for mild hypernatremia?
What management strategy is recommended for mild hypernatremia?
- A low-salt diet (correct)
- Immediate diuretics
- High dose corticosteroids
- Intravenous infusion of hypertonic fluids
Hyponatremia is defined as a serum sodium level below what threshold?
Hyponatremia is defined as a serum sodium level below what threshold?
Which of the following conditions can lead to a high sodium loss, contributing to hyponatremia?
Which of the following conditions can lead to a high sodium loss, contributing to hyponatremia?
What is the primary therapeutic goal in treating electrolyte imbalances?
What is the primary therapeutic goal in treating electrolyte imbalances?
What treatment is appropriate for hypercalcemia?
What treatment is appropriate for hypercalcemia?
Which of the following indicates hyperkalemia?
Which of the following indicates hyperkalemia?
What is the normal serum sodium level considered as hyponatremia?
What is the normal serum sodium level considered as hyponatremia?
Which ion is associated with a condition requiring hypomagnesemia treatment?
Which ion is associated with a condition requiring hypomagnesemia treatment?
What condition is indicated by a serum chloride level greater than 112 mEq/L?
What condition is indicated by a serum chloride level greater than 112 mEq/L?
Which of the following is not a consequence of high sodium levels in the blood?
Which of the following is not a consequence of high sodium levels in the blood?
What should be the initial focus when treating electrolyte imbalances?
What should be the initial focus when treating electrolyte imbalances?
What is the most serious clinical feature of hyperkalemia?
What is the most serious clinical feature of hyperkalemia?
Which dietary source should be restricted to manage mild hyperkalemia?
Which dietary source should be restricted to manage mild hyperkalemia?
What is the definition of hypokalemia?
What is the definition of hypokalemia?
Which symptom is most commonly associated with hypokalemia?
Which symptom is most commonly associated with hypokalemia?
Which treatment is appropriate for severe hypokalemia?
Which treatment is appropriate for severe hypokalemia?
What characterizes acidosis?
What characterizes acidosis?
Which of the following is a mechanism that helps regulate acid-base balance?
Which of the following is a mechanism that helps regulate acid-base balance?
What is the potential consequence if acidosis and alkalosis are not treated promptly?
What is the potential consequence if acidosis and alkalosis are not treated promptly?
What is a respiratory cause of acidosis?
What is a respiratory cause of acidosis?
Which of the following is a treatment for metabolic alkalosis?
Which of the following is a treatment for metabolic alkalosis?
What is a symptom associated with metabolic acidosis?
What is a symptom associated with metabolic acidosis?
Which nursing assessment is crucial before administering potassium?
Which nursing assessment is crucial before administering potassium?
What condition can result from an excessive intake of sodium bicarbonate?
What condition can result from an excessive intake of sodium bicarbonate?
What monitoring is essential during IV potassium infusion?
What monitoring is essential during IV potassium infusion?
Which of the following can indicate respiratory alkalosis?
Which of the following can indicate respiratory alkalosis?
Which symptom indicates a central nervous system stimulation due to alkalosis?
Which symptom indicates a central nervous system stimulation due to alkalosis?
For what is monitoring serum electrolyte levels important during therapy?
For what is monitoring serum electrolyte levels important during therapy?
What is the best method to monitor for signs of transfusion reactions?
What is the best method to monitor for signs of transfusion reactions?
What is the primary indication for using isotonic crystalloids?
What is the primary indication for using isotonic crystalloids?
Which statement best describes hypertonic crystalloids?
Which statement best describes hypertonic crystalloids?
What effect do hypotonic crystalloids typically have on the body?
What effect do hypotonic crystalloids typically have on the body?
What is a common adverse effect of isotonic crystalloids?
What is a common adverse effect of isotonic crystalloids?
Colloids are primarily used for which condition?
Colloids are primarily used for which condition?
What is a characteristic of blood products compared to crystalloids and colloids?
What is a characteristic of blood products compared to crystalloids and colloids?
Which blood product is indicated for increasing clotting factor levels?
Which blood product is indicated for increasing clotting factor levels?
What is a serious potential adverse effect of colloid administration?
What is a serious potential adverse effect of colloid administration?
Which electrolyte imbalance is commonly associated with renal impairment?
Which electrolyte imbalance is commonly associated with renal impairment?
How do sodium bicarbonate and sodium sulfate differ?
How do sodium bicarbonate and sodium sulfate differ?
What is the primary mechanism of action for hypertonic crystalloids?
What is the primary mechanism of action for hypertonic crystalloids?
What is one key feature of blood products?
What is one key feature of blood products?
What is a serious risk associated with dextran therapy?
What is a serious risk associated with dextran therapy?
What percentage of total body weight does water constitute in a middle-aged adult?
What percentage of total body weight does water constitute in a middle-aged adult?
Which hormone is primarily responsible for regulating sodium levels in the body?
Which hormone is primarily responsible for regulating sodium levels in the body?
What is the normal range for osmolality in mOsm/kg?
What is the normal range for osmolality in mOsm/kg?
What happens when hypertonic intravenous fluid is administered?
What happens when hypertonic intravenous fluid is administered?
Which of the following is a primary regulator of fluid output?
Which of the following is a primary regulator of fluid output?
What type of fluids are crystalloids?
What type of fluids are crystalloids?
What is the role of the renin–angiotensin-aldosterone system?
What is the role of the renin–angiotensin-aldosterone system?
Which IV solution has a hypertonic effect when administered?
Which IV solution has a hypertonic effect when administered?
What is the greatest contributor to changes in osmolality?
What is the greatest contributor to changes in osmolality?
What bodily condition can deficient fluid balance disorders lead to?
What bodily condition can deficient fluid balance disorders lead to?
In which scenario would IV fluid therapy be indicated?
In which scenario would IV fluid therapy be indicated?
What primarily drives the thirst mechanism in the body?
What primarily drives the thirst mechanism in the body?
What is isotonic intravenous fluid characterized by?
What is isotonic intravenous fluid characterized by?
Which type of IV solution is designed to replace lost fluids and promote urine output?
Which type of IV solution is designed to replace lost fluids and promote urine output?
What is the pharmacotherapy approach commonly used to correct hypokalemia?
What is the pharmacotherapy approach commonly used to correct hypokalemia?
Which condition is most likely to result from laxative misuse, as seen in the case of Sandy?
Which condition is most likely to result from laxative misuse, as seen in the case of Sandy?
Which nursing action is essential when managing fluid and electrolyte imbalances?
Which nursing action is essential when managing fluid and electrolyte imbalances?
What common cause may lead to metabolic alkalosis that a nurse should recognize?
What common cause may lead to metabolic alkalosis that a nurse should recognize?
What is the primary role of intravenous fluid therapy in treating acid-base disorders?
What is the primary role of intravenous fluid therapy in treating acid-base disorders?
What physiological effect does elevated serum sodium have on the body's cells?
What physiological effect does elevated serum sodium have on the body's cells?
Which clinical feature is NOT typically associated with hypernatremia?
Which clinical feature is NOT typically associated with hypernatremia?
What management strategy is recommended for treating acute hypernatremia in a hypovolemic patient?
What management strategy is recommended for treating acute hypernatremia in a hypovolemic patient?
What is a common cause of hyponatremia related to renal function?
What is a common cause of hyponatremia related to renal function?
During management of a patient with mild hypernatremia, which dietary approach is recommended?
During management of a patient with mild hypernatremia, which dietary approach is recommended?
What should be monitored when administering sodium bicarbonate therapy to patients with cardiac disease?
What should be monitored when administering sodium bicarbonate therapy to patients with cardiac disease?
Which of the following is a contraindication for ammonium chloride therapy?
Which of the following is a contraindication for ammonium chloride therapy?
What dilution method is recommended for oral potassium to minimize gastrointestinal distress?
What dilution method is recommended for oral potassium to minimize gastrointestinal distress?
What is the appropriate rate for intravenous potassium administration in critically ill patients?
What is the appropriate rate for intravenous potassium administration in critically ill patients?
What electrolyte imbalance is indicated by a potassium level of 2.8 mEq/L?
What electrolyte imbalance is indicated by a potassium level of 2.8 mEq/L?
What could be a significant complication of administering ammonium chloride too quickly?
What could be a significant complication of administering ammonium chloride too quickly?
During assessment, which symptom should a nurse monitor for in a patient taking oral potassium?
During assessment, which symptom should a nurse monitor for in a patient taking oral potassium?
Which electrolyte imbalance is most associated with dehydration?
Which electrolyte imbalance is most associated with dehydration?
What is a common symptom of hyperkalemia?
What is a common symptom of hyperkalemia?
Which dietary change is recommended for managing mild hypokalemia?
Which dietary change is recommended for managing mild hypokalemia?
What should be administered in severe hyperkalemia to counteract potassium toxicity on the heart?
What should be administered in severe hyperkalemia to counteract potassium toxicity on the heart?
What pH value indicates alkalosis?
What pH value indicates alkalosis?
Which of the following is a cause of hypokalemia?
Which of the following is a cause of hypokalemia?
In the management of mild hyperkalemia, which food source should be restricted?
In the management of mild hyperkalemia, which food source should be restricted?
Which symptom is likely to occur due to hypokalemia?
Which symptom is likely to occur due to hypokalemia?
What is the critical management action for treating acidosis?
What is the critical management action for treating acidosis?
What is the normal osmolality range in mOsm/kg for a healthy adult?
What is the normal osmolality range in mOsm/kg for a healthy adult?
What primarily regulates fluid intake in the human body?
What primarily regulates fluid intake in the human body?
What occurs when hypotonic intravenous fluid is administered?
What occurs when hypotonic intravenous fluid is administered?
Which type of fluid is characterized by its ability to closely mimic the body's extracellular fluid?
Which type of fluid is characterized by its ability to closely mimic the body's extracellular fluid?
Which hormone is identified as a key regulator of sodium levels in the body?
Which hormone is identified as a key regulator of sodium levels in the body?
What is the primary function of intravenous fluid therapy?
What is the primary function of intravenous fluid therapy?
What is the main purpose of administering isotonic crystalloids?
What is the main purpose of administering isotonic crystalloids?
Which of the following is a common indication for the use of hypertonic crystalloids?
Which of the following is a common indication for the use of hypertonic crystalloids?
What is a potential consequence of deficient fluid balance disorders?
What is a potential consequence of deficient fluid balance disorders?
What is the primary adverse effect associated with hypotonic crystalloids?
What is the primary adverse effect associated with hypotonic crystalloids?
What is the definition of tonicity in relation to fluid movement?
What is the definition of tonicity in relation to fluid movement?
Which intravenously administered fluid is considered hypertonic?
Which intravenously administered fluid is considered hypertonic?
What is the role of 5% albumin as a colloid solution?
What is the role of 5% albumin as a colloid solution?
What type of fluid could be used to treat excess fluid balance disorders?
What type of fluid could be used to treat excess fluid balance disorders?
Which of the following is an adverse effect of blood products?
Which of the following is an adverse effect of blood products?
Which of the following is NOT a cause of water and electrolyte loss?
Which of the following is NOT a cause of water and electrolyte loss?
Which IV fluid type is designed to enter the interstitial spaces and intracellular fluid?
Which IV fluid type is designed to enter the interstitial spaces and intracellular fluid?
What characterizes the difference between whole blood and packed red blood cells (PRBCs)?
What characterizes the difference between whole blood and packed red blood cells (PRBCs)?
What is the primary indicator for administering isotonic crystalloids?
What is the primary indicator for administering isotonic crystalloids?
Which electrolyte is essential for nerve conduction and membrane permeability?
Which electrolyte is essential for nerve conduction and membrane permeability?
What fluid shift occurs when hypertonic intravenous fluid is administered?
What fluid shift occurs when hypertonic intravenous fluid is administered?
A common underlying issue associated with electrolyte imbalance is:
A common underlying issue associated with electrolyte imbalance is:
What is an adverse effect specifically associated with dextran therapy?
What is an adverse effect specifically associated with dextran therapy?
Which solution is indicated for increasing clotting factor levels in patients?
Which solution is indicated for increasing clotting factor levels in patients?
Colloids primarily function by:
Colloids primarily function by:
What is the key safety measure associated with administering blood products?
What is the key safety measure associated with administering blood products?
Flashcards
Hypernatremia Definition
Hypernatremia Definition
Serum sodium level greater than 145 mEq/L
Loop Diuretics Therapeutic Goal
Loop Diuretics Therapeutic Goal
Correct electrolyte imbalances and treat the underlying cause
Hypercalcemia Abnormal Value
Hypercalcemia Abnormal Value
Calcium level greater than 11 mEq/L
Hyponatremia Abnormal Value
Hyponatremia Abnormal Value
Signup and view all the flashcards
Sodium's Role (extracellular)
Sodium's Role (extracellular)
Signup and view all the flashcards
Hypocalcemia Supplement
Hypocalcemia Supplement
Signup and view all the flashcards
Hyperchloremia Treatment
Hyperchloremia Treatment
Signup and view all the flashcards
Hypokalemia Supplement
Hypokalemia Supplement
Signup and view all the flashcards
Fluid Balance
Fluid Balance
Signup and view all the flashcards
Osmolality
Osmolality
Signup and view all the flashcards
Tonicity
Tonicity
Signup and view all the flashcards
Osmosis
Osmosis
Signup and view all the flashcards
Hypertonic IV fluid
Hypertonic IV fluid
Signup and view all the flashcards
Hypotonic IV fluid
Hypotonic IV fluid
Signup and view all the flashcards
Isotonic IV fluid
Isotonic IV fluid
Signup and view all the flashcards
Crystalloids
Crystalloids
Signup and view all the flashcards
Normal Saline
Normal Saline
Signup and view all the flashcards
Dehydration
Dehydration
Signup and view all the flashcards
Fluid Replacement
Fluid Replacement
Signup and view all the flashcards
Electrolytes
Electrolytes
Signup and view all the flashcards
Body Fluid Compartments
Body Fluid Compartments
Signup and view all the flashcards
Thirst Mechanism
Thirst Mechanism
Signup and view all the flashcards
Kidneys
Kidneys
Signup and view all the flashcards
Isotonic Crystalloids
Isotonic Crystalloids
Signup and view all the flashcards
Hypertonic Crystalloids
Hypertonic Crystalloids
Signup and view all the flashcards
Hypotonic Crystalloids
Hypotonic Crystalloids
Signup and view all the flashcards
Crystalloids Adverse Effects (Isotonic/Hypertonic)
Crystalloids Adverse Effects (Isotonic/Hypertonic)
Signup and view all the flashcards
Crystalloids Adverse Effects (Hypotonic)
Crystalloids Adverse Effects (Hypotonic)
Signup and view all the flashcards
Colloids
Colloids
Signup and view all the flashcards
Colloids: Hypovolemic Shock Treatment
Colloids: Hypovolemic Shock Treatment
Signup and view all the flashcards
Colloids: Osmotic Pressure
Colloids: Osmotic Pressure
Signup and view all the flashcards
Blood Products
Blood Products
Signup and view all the flashcards
Blood Products: Indications (Cryoprecipitate/PPF)
Blood Products: Indications (Cryoprecipitate/PPF)
Signup and view all the flashcards
Blood Products: Indications (FFP)
Blood Products: Indications (FFP)
Signup and view all the flashcards
Blood Products: Indications (PRBCs)
Blood Products: Indications (PRBCs)
Signup and view all the flashcards
Blood Products Adverse Effects
Blood Products Adverse Effects
Signup and view all the flashcards
Electrolyte Imbalance Cause
Electrolyte Imbalance Cause
Signup and view all the flashcards
Hypernatremia Cause: Excess Sodium
Hypernatremia Cause: Excess Sodium
Signup and view all the flashcards
Hypernatremia Effects
Hypernatremia Effects
Signup and view all the flashcards
Hypernatremia: Managing the Problem
Hypernatremia: Managing the Problem
Signup and view all the flashcards
Hyponatremia Causes: Sodium Loss
Hyponatremia Causes: Sodium Loss
Signup and view all the flashcards
Hyperkalemia
Hyperkalemia
Signup and view all the flashcards
Hyperkalemia Causes
Hyperkalemia Causes
Signup and view all the flashcards
Hyperkalemia Symptoms
Hyperkalemia Symptoms
Signup and view all the flashcards
Hyperkalemia Management
Hyperkalemia Management
Signup and view all the flashcards
Hypokalemia
Hypokalemia
Signup and view all the flashcards
Hypokalemia Causes
Hypokalemia Causes
Signup and view all the flashcards
Hypokalemia Symptoms
Hypokalemia Symptoms
Signup and view all the flashcards
Hypokalemia Treatment
Hypokalemia Treatment
Signup and view all the flashcards
Acidosis
Acidosis
Signup and view all the flashcards
Alkalosis
Alkalosis
Signup and view all the flashcards
Respiratory Acidosis
Respiratory Acidosis
Signup and view all the flashcards
Metabolic Acidosis
Metabolic Acidosis
Signup and view all the flashcards
Respiratory Alkalosis
Respiratory Alkalosis
Signup and view all the flashcards
Metabolic Alkalosis
Metabolic Alkalosis
Signup and view all the flashcards
Kussmaul Breathing
Kussmaul Breathing
Signup and view all the flashcards
Sodium Bicarbonate Infusion
Sodium Bicarbonate Infusion
Signup and view all the flashcards
Ammonium Chloride
Ammonium Chloride
Signup and view all the flashcards
Nursing Implications
Nursing Implications
Signup and view all the flashcards
Hypernatremia's Effect on Cells
Hypernatremia's Effect on Cells
Signup and view all the flashcards
Hypernatremia Management: Mild vs. Severe
Hypernatremia Management: Mild vs. Severe
Signup and view all the flashcards
Hyponatremia: Causes of Low Sodium
Hyponatremia: Causes of Low Sodium
Signup and view all the flashcards
Hyponatremia: Key Concept
Hyponatremia: Key Concept
Signup and view all the flashcards
Hypernatremia: Causes of High Sodium
Hypernatremia: Causes of High Sodium
Signup and view all the flashcards
What is Tonicity?
What is Tonicity?
Signup and view all the flashcards
Kidney's Role in Fluid Balance
Kidney's Role in Fluid Balance
Signup and view all the flashcards
Hyperkalemia: What is it?
Hyperkalemia: What is it?
Signup and view all the flashcards
Hyperkalemia: What are the signs?
Hyperkalemia: What are the signs?
Signup and view all the flashcards
Hyperkalemia: How do we manage it?
Hyperkalemia: How do we manage it?
Signup and view all the flashcards
Hypokalemia: What is it?
Hypokalemia: What is it?
Signup and view all the flashcards
Hypokalemia: What are the signs?
Hypokalemia: What are the signs?
Signup and view all the flashcards
Hypokalemia: How do we manage it?
Hypokalemia: How do we manage it?
Signup and view all the flashcards
Acidosis: What is it?
Acidosis: What is it?
Signup and view all the flashcards
Alkalosis: What is it?
Alkalosis: What is it?
Signup and view all the flashcards
Electrolyte Balance
Electrolyte Balance
Signup and view all the flashcards
Electrolyte Imbalance
Electrolyte Imbalance
Signup and view all the flashcards
Electrolytes Important to Human Physiology
Electrolytes Important to Human Physiology
Signup and view all the flashcards
Calcium
Calcium
Signup and view all the flashcards
Sodium
Sodium
Signup and view all the flashcards
Study Notes
Drugs for Fluid and Electrolyte Imbalances, and Acid-Base Disorders
- Drugs treat imbalances in fluid, electrolytes, and acid-base.
- Learning objectives include describing conditions requiring intravenous fluids, explaining sodium and potassium replacement therapies, discussing acidosis/alkalosis causes and treatments, and nurses' roles in pharmacologic management of these imbalances.
- A case study highlights Sandy, a 16-year-old, whose low sodium (136 mEq/L) and potassium (2.8 mEq/L) levels, potentially due to a fad diet and laxative use, necessitate assessment and management of electrolyte imbalances.
Body Fluid Compartments
- Water comprises ~60% of a middle-aged adult's body weight.
- Continuous fluid exchange occurs across semipermeable membranes, between intracellular and extracellular compartments.
- Large molecules and less ionized substances cross membranes with difficulty.
Major Fluid Compartments in the Body
- Intracellular fluid (25L): Within cells (40% of body weight)
- Interstitial fluid (12L): Surrounding cells.
- Plasma (3L): Fluid in blood vessels.
Control of Water Balance
- Water balance is critical for homeostasis.
- Imbalances of body fluids, electrolytes, and acid-base levels often necessitate intravenous (IV) therapy.
Osmolality
- Osmolality measures dissolved solutes per kilogram of fluid (~275-295 mOsm/kg).
- Common solutes include sodium, glucose, and urea.
- Changes in osmolality cause water movement; Sodium is the main contributor and is regulated by aldosterone.
Tonicity
- Tonicity describes a solution's ability to cause water movement across a membrane due to osmotic forces.
- Plasma tonicity is used as a reference point for IV solutions.
Osmosis
- Water moves from areas of low to high osmolality.
- Hypertonic IV fluid shifts water from interstitial space to plasma.
- Hypotonic IV fluid shifts water from plasma to interstitial space.
- Isotonic fluids cause no significant fluid shift.
Movement of Fluids and Solution Tonicity
- Isotonic: Equal osmolality; no net fluid movement.
- Hypertonic: Higher osmolality; draws water out of cells.
- Hypotonic: Lower osmolality; draws water into cells.
Regulation of Fluid Intake & Output
- Fluid intake/output is controlled by complex mechanisms.
- Thirst primarily regulates fluid intake.
- Kidneys, the renin-angiotensin-aldosterone system, and antidiuretic hormone (ADH) regulate fluid output.
Fluid Balance Disorders
- Deficient fluid balance (dehydration/shock) necessitates oral/intravenous fluid therapy.
- Excess fluid balance (fluid overload) requires diuretics.
- Identifying and addressing the underlying cause is paramount in fluid and electrolyte management.
Fluid Replacement Agents
- Fluid replacement corrects net fluid loss in the body (dehydration/shock).
- Intravenous fluid therapy maintains blood volume and blood pressure.
Intravenous Fluid Therapy
- IV fluids replace lost fluids/electrolytes (vomiting, diarrhea, laxatives, extensive sweating, burns, hemorrhage, uncontrolled ketoacidosis).
- Crystalloids and colloids are used in IV therapy.
Crystalloids
- Crystalloid IV solutions contain electrolytes.
- These mimic extracellular fluid (ECF) and help replace depleted fluids and promote urine output.
- Tonicity dictates the compartment the fluid enters.
Selected Crystalloid IV Solutions
- Crystalloid solutions vary in tonicity.
- Normal saline (0.9% NaCl) is isotonic; lactated Ringer's and Plasma-Lyte 148 solutions are also isotonic.
- Hypotonic solutions (like 0.45% saline) have lower and hypertonic solutions (like dextrose in water or normal saline) have higher osmolality than plasma.
Isotonic Crystalloids
- Isotonic crystalloids expand plasma volume without significant fluid shifts between compartments.
- These are primary choices in cases of fluid loss or low blood pressure. Normal saline is the most common choice.
Hypertonic Crystalloids
- Hypertonic crystalloids draw water from cells/tissues into vascular compartment.
- Indications include treating cellular edema, specifically cerebral edema.
Hypotonic Crystalloids
- Hypotonic solutions shift water from plasma to cells and tissues.
- Not for expanding plasma volume; use in situations of hypernatremia and cellular dehydration.
Adverse effects of Crystalloids
- Isotonic/hypertonic solutions may cause fluid overload.
- Hypotonic solutions might cause intravascular volume depletion and can cause hypotension/cellular swelling. This can lead to peripheral edema.
Colloids
- Colloids contain large molecules (proteins, starches) that mainly exert their effect in the intravascular space.
- They expand plasma volume more quickly due to osmotic pressure, drawing water from interstitial and intracellular spaces into the vascular compartment.
- Colloids are used to treat hypovolemia, shock, burns, or hemorrhage.
Selected Colloid Solutions (Plasma Volume Expanders)
- Various colloids, like albumin, dextrans, and hetastarch, are used as plasma volume expanders. They generally have isotonic tonicity.
Selected colloid solutions
- Normal serum albumin is the most frequent utilized colloid.
- Dextran is a synthetic polysaccharide, causing rapid plasma volume expansion.
- Hetastarch is a synthetic colloid similar to albumin, exerting effects over a longer period.
Adverse effects of Colloids
- Colloids, generally safe, can temporarily alter coagulation; blood-clotting factors should be monitored.
- Rare cases of anaphylaxis or kidney problems have occurred.
Blood Products
- Blood products are the only fluids that carry oxygen, supporting tissue oxygenation and increasing plasma volume.
- Human donors are required, making these fluids the most expensive.
Indications for Blood Products
- Cryoprecipitate/plasma protein factors are indicated for acute bleeding (>20% blood loss).
- Fresh frozen plasma (FFP) increases clotting factor levels in situations with demonstrated deficiencies.
- Packed red blood cells (PRBCs) increase oxygen-carrying capacity in cases of anemia or significant blood loss, up to 25% loss.
- Whole blood has the same uses as packed red blood cells, but is beneficial in severe cases of blood loss (more than 25% loss).
Adverse effects of Blood Products
- Blood products can induce incompatibility responses with the recipient's immune system.
- Crossmatching is critical to avoid transfusion reactions, anaphylaxis, and the transmission of pathogens (e.g., hepatitis, HIV).
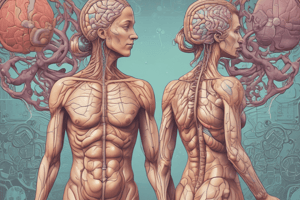
Electrolyte Balance
- Positively or negatively charged inorganic molecules (electrolytes) are essential for nerve conduction, membrane permeability, water balance, and other bodily functions.
Electrolytes Important to Human Physiology
- A table of common cation and anion electrolytes and their formulas is provided for reference.
Electrolyte Imbalance
- Electrolyte imbalances often signal underlying medical conditions.
- These imbalances may stem from renal problems, adverse drug reactions, etc.
- Correcting the imbalance and addressing the underlying cause are critical to treatment.
Electrolyte Imbalances
- A table of diverse electrolytes, their abnormal levels, and associated treatment methods.
Sodium
- Sodium (a major extracellular cation) is crucial for regulating osmolality, water balance, and blood pressure.
Renal Regulation of Sodium and Potassium Balance
- A diagram showing the roles of the kidneys and adrenal gland (through aldosterone) in regulating sodium and potassium balance.
Hypernatremia
- Hypernatremia involves serum sodium levels above 145 mEq/L.
- Causes range from renal diseases & high sodium intake, to excessive water loss through inadequate water intake, watery diarrhea, fevers, burns, and high levels of corticosteroids.
Hypernatremia (Contd.)
- High serum sodium concentration leads to increased plasma osmolality, drawing water from the interstitial spaces and cells into the intravascular space; this results in cellular dehydration.
- Symptoms include thirst, fatigue, weakness, muscle twitching, convulsions, altered mental status, and decreased consciousness.
- Treatment of mild cases involves reducing sodium intake. For acute hypernatremia in hypovolemic patients, IV hypotonic solutions like 5% dextrose or 0.45% NaCl are indicated. Hypervolemic patients may benefit from diuretics.
Hyponatremia
- Hyponatremia involves serum sodium levels below 135 mEq/L.
- Causes include significant sodium loss due to kidney disease, excessive gastrointestinal fluid loss (vomiting, diarrhea), or burns, and excessive sweating.
- Hyponatremia may also be caused by excessive dilution of plasma (due to disorders of the adrenal gland or ADH secretion, or infusion of hypotonic solutions).
Hyponatremia (Contd.)
- Early symptoms are nausea, vomiting, anorexia, and abdominal cramping.
- Later symptoms may include altered neurologic status: confusion, lethargy, seizures, coma, and muscle twitching.
- The rate of correcting hyponatremia must be monitored carefully; rapid correction can lead to potentially dangerous complications. Therapy depends on whether the patient is hypovolemic or hypervolemic.
Potassium Balance
- Potassium (a primary intracellular cation) plays a critical role in nerve and muscle function, and acid-base balance.
- Aldosterone regulates potassium secretion, influencing its balance with sodium reabsorption in the kidneys.
Hyperkalemia
- Hyperkalemia involves serum potassium levels exceeding 5 mEq/L.
- Causes encompass various renal diseases, high potassium intake (especially from drugs like potassium-sparing diuretics).
Hyperkalemia (Contd.)
- Symptoms include muscle twitching, fatigue, paresthesia, dyspnea, cramping, and diarrhea. More serious complications include cardiac dysrhythmias, and cardiac arrest.
- Treatment of mild cases involves restricting potassium-rich foods.
- For severe hyperkalemia, IV glucose with insulin, albuterol, and calcium gluconate can be administered to reduce the potassium levels.
Hypokalemia
- Hypokalemia is characterized by serum potassium levels below 3.5 mEq/L.
- Causes include excessive potassium loss due to diuretic use, strenuous activity, or severe vomiting/diarrhea.
Hypokalemia (Contd.)
- Symptoms include muscle weakness, muscle cramps, lethargy, anorexia, dysrhythmias, paralysis, and even cardiac arrest.
Hypokalemia (Contd.)
- Mild cases may be treated by increasing dietary potassium intake (e.g., dried fruits, nuts, bananas, and avocados) or/and oral potassium supplements.
- Severe cases may need intravenous potassium supplementation, but IV administration rates and dilution are critical parameters.
Acid-Base Disorders
- Acidosis (pH below 7.35) and alkalosis (pH above 7.45) are imbalances needing attention to symptoms and addressing the underlying causes.
Regulation of Acid-Base Balances
- Buffers (bicarbonate and phosphate) help maintain normal body pH by neutralizing strong acids and bases.
- Lungs eliminate CO2, and kidneys remove H+, crucial for acid-base homeostasis.
Acid-Base Imbalances
- A diagram demonstrates the balance between acids and bases, with acidosis occurring at pH below 7.35 and alkalosis above 7.45.
Causes of Alkalosis and Acidosis
- Comprehensive table detailing respiratory and metabolic causes of acidosis and alkalosis. Examples include hypoventilation, hyperventilation, diarrhea, kidney failure, and ingestion of excess sodium bicarbonate, as well as diuretic use.
Pharmacotherapy of Acidosis
- Acidosis symptoms, such as lethargy, confusion, and coma, stem from central nervous system depression.
- Kussmaul breathing (rapid, deep respirations) may indicate the body's compensatory effort for metabolic acidosis.
- Treatment for metabolic acidosis involves administering sodium bicarbonate to reverse the excessive acid effects.
Pharmacotherapy of Alkalosis
- Alkalosis, often with central nervous system stimulation (nervousness, hyperreflexia, seizures), may have slowed shallow respirations as a compensatory mechanism.
- Mild alkalosis may be addressed with sodium chloride and potassium chloride; severe cases require ammonium chloride.
Nursing Implications (Assessment)
- Assess baseline fluid/electrolyte balance, vital signs, skin, membranes, daily weights, and intake/output.
- Monitor ECG to measure potassium levels before potassium administration.
- Evaluate for contraindications to therapies.
- Assess transfusion history.
- Establish venous access.
Nursing Implications (Monitor)
- Monitor electrolytes (serum/urine) during treatment.
- Monitor infusions’ rate and the solution; identify/evaluate infiltration/complications.
- Observe for therapeutic response based on evaluation of lab values (RBC/WBC/H&H/electrolytes), fluid balance, activities, and adverse effects
- Monitor closely.
Nursing Implications (Fluid Replacement)
- Administer colloids slowly.
- Monitor for fluid overload/heart failure.
- Carefully follow transfusion procedures.
- Monitor patients cautiously for transfusion reactions.
Nursing implication (Sodium Replacement Therapy)
- Assess sodium and electrolyte balance.
- Be alert to hyponatremia/hypernatremia-related signs/symptoms.
- Monitor serum sodium levels, urine specific gravity, serum/urine osmolality.
- Teach patients about symptoms related to fluid overload and appropriate fluid/electrolyte replacement strategies.
Nursing Implications (Potassium Infusion)
- IV potassium administration should not exceed 10 mEq/hr for patients not on cardiac monitors; higher rates may be appropriate in critically ill patients using cardiac monitors.
- Potassium should never be delivered as a bolus or undiluted IV solution.
Nursing Implications (Oral Potassium)
- Dilute oral potassium supplements in water or juice.
- Monitor for gastrointestinal distress (nausea, vomiting, abdominal pain, or bleeding).
Nursing Implications (Acid-Base Agents)
- Monitor arterial blood gases as appropriate for acid-base imbalances.
- Use sodium bicarbonate cautiously in patients with cardiac or renal conditions; assess risks.
- Administer ammonium chloride slowly based on the patient's condition and to mitigate potential risks of ammonia toxicity.
Case Study (Refer to the Recorded Lecture for the Answers)
- Sandy, a 16-year-old, presents with possible electrolyte imbalance potentially caused by a "fad diet" and laxative use, prompting assessment of her sodium (136 mEq/L) and potassium (2.8 mEq/L) levels.
Key Terms
- A summary of key terms for fluid and electrolyte imbalances, including dehydration, shock, IV therapy, crystalloids, colloids, hypernatremia, hyponatremia, hyperkalemia, hypokalemia, acidosis, and alkalosis.
Review Question
- Students should answer three multiple-choice questions after the lesson.
- A QR code provides access to the review questions.
References
- Provides citations from two pharmacology textbooks.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.