Podcast
Questions and Answers
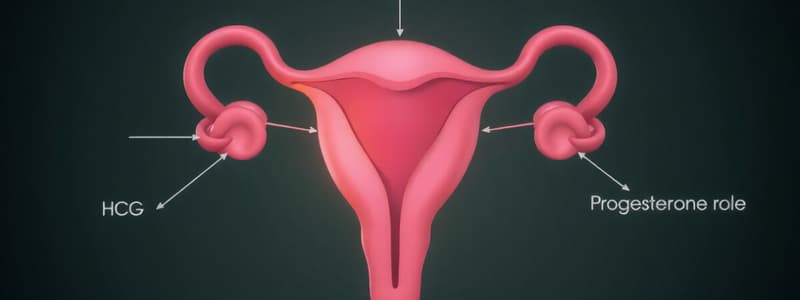
What is the primary function of hCG (human chorionic gonadotropin) in early pregnancy?
What is the primary function of hCG (human chorionic gonadotropin) in early pregnancy?
- It triggers the development of the decidua, the lining of the uterus where the embryo implants.
- It stimulates the corpus luteum to continue producing estrogen and progesterone, maintaining the pregnancy. (correct)
- It stimulates the release of oxytocin, which promotes uterine contractions.
- It inhibits the production of estrogen and progesterone by the corpus luteum.
Which of the following is NOT a component of the placenta?
Which of the following is NOT a component of the placenta?
- Myometrial layer of the uterus (correct)
- Trophoblast cells
- Placental villi
- Fetal blood vessels
What is the primary role of progesterone during early pregnancy?
What is the primary role of progesterone during early pregnancy?
- Decreasing uterine contractility to sustain the pregnancy (correct)
- Maintaining the corpus luteum's function
- Promoting the growth of the endometrial lining
- Stimulating the development of the placenta
During the early stages of pregnancy, how are nutrients supplied to the developing embryo?
During the early stages of pregnancy, how are nutrients supplied to the developing embryo?
What is the role of the trophoblast cells in the placenta?
What is the role of the trophoblast cells in the placenta?
Which of the following events occurs approximately 8-12 weeks into gestation?
Which of the following events occurs approximately 8-12 weeks into gestation?
What is the direct consequence of a decrease in estrogen and progesterone levels in early pregnancy?
What is the direct consequence of a decrease in estrogen and progesterone levels in early pregnancy?
What is the decidua formed from?
What is the decidua formed from?
What hormone is responsible for milk ejection?
What hormone is responsible for milk ejection?
Which of the following hormones is the primary contributor to the increase in body temperature during pregnancy?
Which of the following hormones is the primary contributor to the increase in body temperature during pregnancy?
What happens to the levels of both progesterone and estrogen in the mother's body at the end of gestation?
What happens to the levels of both progesterone and estrogen in the mother's body at the end of gestation?
What is the role of placental lactogen in pregnancy and lactation?
What is the role of placental lactogen in pregnancy and lactation?
Which hormone is responsible for suppressing the follicular development and preventing further ovarian cycles during pregnancy?
Which hormone is responsible for suppressing the follicular development and preventing further ovarian cycles during pregnancy?
How does the placenta contribute to the timing of birth?
How does the placenta contribute to the timing of birth?
What is the primary mechanism by which estrogen stimulates labor?
What is the primary mechanism by which estrogen stimulates labor?
Which hormone is the primary regulator of milk production?
Which hormone is the primary regulator of milk production?
What is the role of prostaglandins in labor?
What is the role of prostaglandins in labor?
How does the body handle the increase in glucose levels during pregnancy?
How does the body handle the increase in glucose levels during pregnancy?
What is the primary reason for the increase in cardiac output during pregnancy?
What is the primary reason for the increase in cardiac output during pregnancy?
How does the fetus contribute to the increase in maternal estrogen levels at the end of gestation?
How does the fetus contribute to the increase in maternal estrogen levels at the end of gestation?
What is the major physiological change that occurs in the cardiovascular system during pregnancy?
What is the major physiological change that occurs in the cardiovascular system during pregnancy?
What is the primary function of progesterone in the maintenance of pregnancy?
What is the primary function of progesterone in the maintenance of pregnancy?
What is the primary role of oxytocin in lactation?
What is the primary role of oxytocin in lactation?
Which of the following hormones is directly involved in increasing insulin resistance during pregnancy?
Which of the following hormones is directly involved in increasing insulin resistance during pregnancy?
Flashcards
Fertilization
Fertilization
Occurs in the fallopian tubes during the luteal phase.
Decidua
Decidua
The area where the embryo implants and grows into the uterine wall.
Placenta
Placenta
Structure formed from fetal tissues that supports the embryo.
hCG (human chorionic gonadotropin)
hCG (human chorionic gonadotropin)
Signup and view all the flashcards
Trophoblast cells
Trophoblast cells
Signup and view all the flashcards
Progesterone
Progesterone
Signup and view all the flashcards
Estrogen
Estrogen
Signup and view all the flashcards
Corps luteum
Corps luteum
Signup and view all the flashcards
Placental lactogen
Placental lactogen
Signup and view all the flashcards
Brain-pituitary-gonadal axis
Brain-pituitary-gonadal axis
Signup and view all the flashcards
Progesterone effects
Progesterone effects
Signup and view all the flashcards
Mammary gland changes
Mammary gland changes
Signup and view all the flashcards
Cardiac output changes
Cardiac output changes
Signup and view all the flashcards
Gestational hypertension
Gestational hypertension
Signup and view all the flashcards
Insulin resistance
Insulin resistance
Signup and view all the flashcards
Labor stimulation
Labor stimulation
Signup and view all the flashcards
Positive feedback loop in labor
Positive feedback loop in labor
Signup and view all the flashcards
Fetal adrenal gland role
Fetal adrenal gland role
Signup and view all the flashcards
Suckling reflex
Suckling reflex
Signup and view all the flashcards
Colostrum
Colostrum
Signup and view all the flashcards
Prolactin decrease over time
Prolactin decrease over time
Signup and view all the flashcards
Early pregnancy maintenance
Early pregnancy maintenance
Signup and view all the flashcards
Study Notes
Early Pregnancy Hormonal Changes
- Fertilization occurs in the fallopian tubes during the luteal phase.
- Fallopian tube and uterine glands provide nutrients for early embryonic development.
- Embryo implants in the uterine endometrial layer around day 7.
- Endometrium thickens and becomes vascularized.
- Decidua is the implanted area, forming the placenta.
- Placenta is derived from fetal tissues, including the trophoblast.
- Maternal component includes the uterine wall and maternal blood vessels.
- Maternal blood surrounds placental villi for nutrient and waste exchange.
- Maternal circulation supplies fetal nutrients, not uterine wall glands.
- High estrogen levels promote endometrial and myometrial proliferation and placental blood vessel growth.
- Progesterone decreases uterine contractility, maintaining uterine quiescence.
- Trophoblast cells create a barrier and transport substances.
- hCG (human chorionic gonadotropin), structurally similar to LH and FSH, is secreted by trophoblast cells.
- hCG stimulates corpus luteum to produce estrogen and progesterone, crucial for maintaining pregnancy.
- Early pregnancy loss (miscarriage) can result from insufficient hCG, leading to hormone drops.
- Around 8-12 weeks, placenta takes over estrogen and progesterone production (placental shift).
- Corpus luteum is essential for hormones before placental shift.
- Insufficient placental hormones after 12 weeks can cause pregnancy failure.
- Placental lactogen, structurally similar to prolactin and growth hormone, plays a role in glucose metabolism and breast development.
Physiological Changes During Pregnancy
- Brain-pituitary-gonadal axis regulates to prevent ovarian cycles.
- Placental estrogen and progesterone inhibit LH and FSH, preventing follicular development.
- Progesterone increases body temperature.
- Estrogen and progesterone affect maternal behaviors.
- Increased food intake due to high metabolic demands.
- Mammary gland changes:
- Puberty: Estrogen and growth hormone stimulate ductal growth.
- Pregnancy: Estrogen and progesterone stimulate lobular-alveolar growth.
- Cortisol, thyroid hormone, and prolactin contribute to breast development.
- Placental lactogen levels rise with placental development, supporting fetal growth and alveoli structure for milk.
- Lactogenesis requires multiple hormones including insulin and cortisol.
- High progesterone inhibits milk production.
- Postpartum lactation requires oxytocin stimulation.
- Cardiovascular Changes:
- Uterine blood vessels increase to supply placenta.
- Cardiac output increases (higher stroke volume and heart rate).
- Blood volume increases by 40%.
- Blood pressure decreases due to reduced total peripheral resistance.
- Uterine and renal arteries dilate for increased blood flow.
- Increased placental blood flow for fetal needs.
- Gestational hypertension is abnormal pressure increase.
- Metabolic Changes:
- High insulin levels but resistance to insulin; reduced glucose tolerance.
- Elevated maternal glucose ensures fetal glucose supply.
- Cortisol and placental lactogen increase insulin resistance.
- Increased fat deposition stores for milk.
- Shift in metabolism to supply glucose to the fetus and store fat for milk.
- Gestational diabetes is excessive insulin resistance.
Labor and Delivery
- Estrogen stimulates labor and delivery.
- Estrogen enhances oxytocin's effect and stimulates prostaglandin secretion for myometrial contraction (PGF2 alpha).
- Estrogen increases oxytocin receptors, intensifying oxytocin's action and prostaglandin production.
- Uterine contractions stretch the cervix, stimulating oxytocin release.
- Oxytocin causes uterine contractions via prostaglandin effects.
- Positive feedback loop: Cervical stretch-oxytocin-contractions-further stretch.
- Oxytocin central to the loop, causing contractions and cervical stretch.
- Progesterone decreases estrogen/oxytocin receptors, inhibiting prostaglandin production and maintaining uterine quiescence.
- Estrogen increases receptors, increasing PGF2 alpha action. - Birth occurs when estrogen effect outweighs progesterone effect.
- Estradiol levels rise due to placental production at the end of pregnancy.
- Progesterone levels do not drop; myometrial response to progesterone decreases due to receptor changes.
- Fetus plays a role in the timing:
- Fetal placenta produces estrogen.
- Fetal adrenal gland produces androgens for placental estrogen production (DHEA).
- Fetal adrenal gland maturation increases steroid production (DHEA), increasing maternal estrogen.
Lactation
- Suckling stimulates prolactin and oxytocin release.
- Prolactin from anterior pituitary increases milk protein production.
- Oxytocin from posterior pituitary causes milk ejection.
- Colostrum, early milk, is lower in protein but has glucose and antibodies.
- Milk production increases over the first few days.
- Prolactin response to suckling decreases over time.
- High prolactin levels can prevent ovulation but aren't reliable birth control.
Summary Points
- Early pregnancy maintained by corpus luteum (stimulated by hCG) followed by placental hormone production.
- Estrogen and progesterone adjust maternal physiology (mammary glands, cardiovascular).
- Estrogen needed for endometrial proliferation and placental blood flow.
- Progesterone maintains uterine quiescence; estrogen drives labor.
- Oxytocin crucial for positive feedback loop during labor.
- Prolactin and oxytocin stimulate milk production and ejection.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.