Podcast
Questions and Answers
What is the primary symptom of dysphagia?
What is the primary symptom of dysphagia?
- Pain during swallowing
- Regurgitation of food
- Difficulty in speaking
- Something sticking in the throat or chest during swallowing or immediately after (correct)
Which type of tumor is most commonly associated with dysphagia?
Which type of tumor is most commonly associated with dysphagia?
- Lymphoma
- Leiomyoma
- Squamous cell carcinoma (correct)
- Adenocarcinoma
What is the primary cause of oesophageal spasms leading to dysphagia?
What is the primary cause of oesophageal spasms leading to dysphagia?
- Gastroesophageal reflux disease
- Acid reflux
- Neuromuscular disorders
- Atypical achalasia (correct)
What is the term for a fibrous stricture that forms at the upper end of the oesophagus due to mucosal atrophy?
What is the term for a fibrous stricture that forms at the upper end of the oesophagus due to mucosal atrophy?
What is the primary treatment for a soft food bolus causing dysphagia?
What is the primary treatment for a soft food bolus causing dysphagia?
What is the complication of a tumor spreading to the trachea in dysphagia?
What is the complication of a tumor spreading to the trachea in dysphagia?
What is the risk of iron deficiency due to chronic inflammation?
What is the risk of iron deficiency due to chronic inflammation?
What is the age group where carcinoma of the oesophagus is most common?
What is the age group where carcinoma of the oesophagus is most common?
What is a risk factor for carcinoma of the oesophagus?
What is a risk factor for carcinoma of the oesophagus?
What is a symptom of carcinoma of the oesophagus?
What is a symptom of carcinoma of the oesophagus?
What is the primary complication of retained oesophageal contents?
What is the primary complication of retained oesophageal contents?
What is the main reason for oesophagitis?
What is the main reason for oesophagitis?
What is a local spread effect of carcinoma of the oesophagus?
What is a local spread effect of carcinoma of the oesophagus?
What is the characteristic feature of Globus hystericus?
What is the characteristic feature of Globus hystericus?
What is the most common type of carcinoma present in oesophagus carcinoma?
What is the most common type of carcinoma present in oesophagus carcinoma?
What type of muscle coats the inner and outer layers of the oesophagus?
What type of muscle coats the inner and outer layers of the oesophagus?
How can the oesophagus spread to the liver?
How can the oesophagus spread to the liver?
What is the weak point of the oesophagus?
What is the weak point of the oesophagus?
What is a diagnostic test for carcinoma of the oesophagus?
What is a diagnostic test for carcinoma of the oesophagus?
What type of epithelium lines the mucosal layer of the oesophagus?
What type of epithelium lines the mucosal layer of the oesophagus?
What is pyloric stenosis?
What is pyloric stenosis?
What is haematemesis?
What is haematemesis?
What is the main reason for pharyngeal pouch disease?
What is the main reason for pharyngeal pouch disease?
What is achalasia of the cardia?
What is achalasia of the cardia?
What is the function of the vagus nerve in the oesophagus?
What is the function of the vagus nerve in the oesophagus?
What is the consequence of retained oesophageal contents?
What is the consequence of retained oesophageal contents?
What is the primary result of achalasia of the cardia?
What is the primary result of achalasia of the cardia?
What is the main difference between peptic and gastric ulcers in terms of areas affected?
What is the main difference between peptic and gastric ulcers in terms of areas affected?
What is the primary cause of peptic ulcer disease?
What is the primary cause of peptic ulcer disease?
What is the purpose of quadruple therapy in treating peptic ulcers?
What is the purpose of quadruple therapy in treating peptic ulcers?
What is the result of chronic duodenal ulceration?
What is the result of chronic duodenal ulceration?
What is the primary symptom of peptic ulcer disease?
What is the primary symptom of peptic ulcer disease?
What is the purpose of controlling predisposing factors in treating peptic ulcers?
What is the purpose of controlling predisposing factors in treating peptic ulcers?
What is the result of an oesophageal spasm?
What is the result of an oesophageal spasm?
What is the primary treatment for oesophageal webs?
What is the primary treatment for oesophageal webs?
What is the primary difference between an acute and chronic duodenal ulcer?
What is the primary difference between an acute and chronic duodenal ulcer?
Flashcards are hidden until you start studying
Study Notes
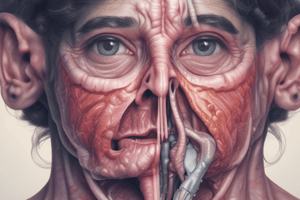
Dysphagia
- Dysphagia is difficulty in swallowing
- Symptom: something sticking in throat/chest during or after swallowing
- 9 oesophageal reasons for dysphagia:
- Tumours (SCC, adenocarcinoma)
- Inflammation (acid reflux, drugs, chemical burn)
- Stricture (radiation, acid reflux)
- Foreign body (soft food bolus, impacted coins, bones)
- Trauma (bones, surgery)
- Web (mucosa becomes atrophic, fibrous stricture forms)
- Goitre, enlarged left atrium, mediastinal glands
- Oesophageal spasms (atypical achalasia, acid reflux, neuromuscular disorders, cardia obstruction)
Pharyngeal and Oral Causes of Dysphagia
- 10 oral and pharyngeal reasons for dysphagia:
- Tumours (SCC)
- Inflammation (severe candidiasis, herpes, tonsillitis, glossitis)
- Fibrosis (scleroderma)
- Trauma (bones, surgery)
- Pouch (herniation of mucosa, food collects in pouch)
- Deformity of cervical spine
- Xerostomia (Sjogren's, drugs)
- Stroke, Parkinson's, MS, MG, Bulbar Palsy
- Globus hystericus (perceived lump in throat, worse with saliva, less with food/liquids)
GI Disease Symptoms
- 9 symptoms of GI disease:
- Abdominal pain
- Dysphagia
- Heartburn
- Dyspepsia
- Flatulence
- Vomiting
- Constipation
- Diarrhoea
- Steatorrhoea
Oesophagus
- The oesophagus is a musculotendinous tube connecting the pharynx to the stomach
- 4 symptoms associated with the oesophagus:
- Dysphagia
- Pain (acid reflux)
- Cough or vomiting (food/liquids refluxing back to pharynx)
- Bleeding (haematemesis)
- 6 diseases associated with the oesophagus:
- Pharyngeal pouch
- Achalasia
- Oesophageal spasm
- Oesophageal web
- Peptic ulcer disease/reflux
- Carcinoma
Oesophageal Anatomy and Function
- The oesophagus consists of 3 muscles: superior, middle, and inferior constrictor muscles (striated)
- Weak point of the oesophagus: Killian's dehiscence, where Zeneker's diverticulum can form
- Innervation: vagus nerve (X)
- Epithelium lining the mucosal layer: stratified squamous non-keratinising epithelium
- Swallowing occurs through peristalsis: a peristaltic wave triggers, food bolus is pushed into the stomach, and the gut stretches, causing depolarisation and action potential, leading to waves of muscle relaxation and contraction.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.