Podcast
Questions and Answers
What is the primary function of the propulsion process in the digestive system?
What is the primary function of the propulsion process in the digestive system?
- To facilitate movement of food through the GI tract (correct)
- To increase contact of food with digestive chemicals
- To release digestive enzymes
- To break down large nutrient molecules into smaller ones
What is the name of the process by which food is broken down into smaller molecules?
What is the name of the process by which food is broken down into smaller molecules?
- Secretion
- Ingestion
- Digestion (correct)
- Absorption
What is the term for the movement of digested molecules into the blood and lymph?
What is the term for the movement of digested molecules into the blood and lymph?
- Ingestion
- Absorption (correct)
- Digestion
- Defecation
What is the layer of the GI tract that comes into contact with food and digesting chemicals?
What is the layer of the GI tract that comes into contact with food and digesting chemicals?
What is the term for the process of taking food and liquids into the mouth?
What is the term for the process of taking food and liquids into the mouth?
What is the term for the elimination of wastes, undigested material, and other substances from the body?
What is the term for the elimination of wastes, undigested material, and other substances from the body?
What is the function of the pyloric sphincter?
What is the function of the pyloric sphincter?
Which part of the stomach is the most superior and lies under the diaphragm?
Which part of the stomach is the most superior and lies under the diaphragm?
What is the function of intrinsic factor in the stomach?
What is the function of intrinsic factor in the stomach?
What is the term for the process of food particles being forced back into the body of the stomach for further mixing with gastric juices?
What is the term for the process of food particles being forced back into the body of the stomach for further mixing with gastric juices?
What is the approximate volume of the stomach that serves as a reservoir?
What is the approximate volume of the stomach that serves as a reservoir?
What is the term for the passage of chyme from the stomach into the small intestine?
What is the term for the passage of chyme from the stomach into the small intestine?
Where is the liver located?
Where is the liver located?
What is the function of the bile produced by the liver?
What is the function of the bile produced by the liver?
What is the name of the lobe that is located lateral to the IVC?
What is the name of the lobe that is located lateral to the IVC?
What is the function of the liver in metabolism?
What is the function of the liver in metabolism?
What is the name of the small ducts between hepatocytes that collect bile?
What is the name of the small ducts between hepatocytes that collect bile?
What is the term for the process of engulfing and digesting old red and white blood cells and some bacteria?
What is the term for the process of engulfing and digesting old red and white blood cells and some bacteria?
What is the duration of the gastric phase?
What is the duration of the gastric phase?
What is the function of the large intestine in terms of absorption?
What is the function of the large intestine in terms of absorption?
Which hormone is involved in the intestinal phase of digestion?
Which hormone is involved in the intestinal phase of digestion?
What is the structure of the muscularis in the large intestine?
What is the structure of the muscularis in the large intestine?
What is the name of the blind pouch in the large intestine?
What is the name of the blind pouch in the large intestine?
What is the shape of the sigmoid colon?
What is the shape of the sigmoid colon?
What is the percentage of oxygenated blood supplied to the liver by the hepatic artery?
What is the percentage of oxygenated blood supplied to the liver by the hepatic artery?
Which part of the liver receives deoxygenated blood from the hepatic portal vein?
Which part of the liver receives deoxygenated blood from the hepatic portal vein?
What is the name of the tube that is used to relieve esophageal varices?
What is the name of the tube that is used to relieve esophageal varices?
Which enzyme is responsible for breaking down proteins in the small intestine?
Which enzyme is responsible for breaking down proteins in the small intestine?
What is the name of the hormone that stimulates the pancreas to secrete enzymes?
What is the name of the hormone that stimulates the pancreas to secrete enzymes?
What is the name of the duct that is formed by the union of the right and left hepatic ducts?
What is the name of the duct that is formed by the union of the right and left hepatic ducts?
Which layer of the GI tract is in direct contact with the contents of the GI tract and is sloughed off and replaced every 5 to 7 days?
Which layer of the GI tract is in direct contact with the contents of the GI tract and is sloughed off and replaced every 5 to 7 days?
What is the function of the MALT in the GI tract?
What is the function of the MALT in the GI tract?
Which layer of the GI tract contains many blood and lymphatic vessels?
Which layer of the GI tract contains many blood and lymphatic vessels?
What is the function of the submucosal plexus in the GI tract?
What is the function of the submucosal plexus in the GI tract?
Which layer of the GI tract is responsible for involuntary contractions that help break down food, mix it, and propel it?
Which layer of the GI tract is responsible for involuntary contractions that help break down food, mix it, and propel it?
Which type of muscle is found in the mouth, pharynx, upper esophagus, and external anal sphincter?
Which type of muscle is found in the mouth, pharynx, upper esophagus, and external anal sphincter?
What is the function of the serosa layer in the GI tract?
What is the function of the serosa layer in the GI tract?
What is the primary function of the peritoneal cavity?
What is the primary function of the peritoneal cavity?
Which structure is the largest serous membrane of the body?
Which structure is the largest serous membrane of the body?
Which of the following structures is NOT retroperitoneal?
Which of the following structures is NOT retroperitoneal?
Which of the following peritoneal folds is not retroperitoneal?
Which of the following peritoneal folds is not retroperitoneal?
What is the primary function of the uvula?
What is the primary function of the uvula?
Which of the following phases of deglutition is under voluntary control?
Which of the following phases of deglutition is under voluntary control?
What is the function of the Mesentery and Mesocolon?
What is the function of the Mesentery and Mesocolon?
What is the location of the esophagus in relation to the trachea?
What is the location of the esophagus in relation to the trachea?
What is the function of the cardiac sphincter?
What is the function of the cardiac sphincter?
What is the shape of the stomach in most people?
What is the shape of the stomach in most people?
What is the function of the soft palate?
What is the function of the soft palate?
Which of the following structures is NOT part of the oral cavity?
Which of the following structures is NOT part of the oral cavity?
What is the function of the upper esophageal sphincter?
What is the function of the upper esophageal sphincter?
What is the primary function of parietal cells in the stomach?
What is the primary function of parietal cells in the stomach?
What is the main reason why mucous production is essential in the stomach?
What is the main reason why mucous production is essential in the stomach?
What is the name of the condition where the stomach pushes through the diaphragm?
What is the name of the condition where the stomach pushes through the diaphragm?
What is the primary function of the small intestine?
What is the primary function of the small intestine?
What is the name of the valve that separates the small intestine from the large intestine?
What is the name of the valve that separates the small intestine from the large intestine?
What is the name of the cells that produce lysozyme to regulate the microbial population in the small intestine?
What is the name of the cells that produce lysozyme to regulate the microbial population in the small intestine?
What is the primary function of the crypts of Lieberkuhn in the small intestine?
What is the primary function of the crypts of Lieberkuhn in the small intestine?
What is the name of the phase of digestion that occurs in the mouth and stomach in preparation for food?
What is the name of the phase of digestion that occurs in the mouth and stomach in preparation for food?
What is the primary function of the duodenal glands in the small intestine?
What is the primary function of the duodenal glands in the small intestine?
What is the name of the enzyme that activates trypsin in the small intestine?
What is the name of the enzyme that activates trypsin in the small intestine?
What is the function of lingual glands in the tongue?
What is the function of lingual glands in the tongue?
What is the pH of saliva?
What is the pH of saliva?
Which of the following enzymes is produced by the pancreas and breaks down starch into simpler sugars?
Which of the following enzymes is produced by the pancreas and breaks down starch into simpler sugars?
What is the function of the islets of Langerhans in the pancreas?
What is the function of the islets of Langerhans in the pancreas?
What is the name of the duct that joins the common bile duct to form the hepatopancreatic duct?
What is the name of the duct that joins the common bile duct to form the hepatopancreatic duct?
What is the main function of the papillae on the tongue?
What is the main function of the papillae on the tongue?
What is the name of the muscle that attaches to the hyoid, mandible, and styloid process of the temporal bone?
What is the name of the muscle that attaches to the hyoid, mandible, and styloid process of the temporal bone?
What is the daily production of saliva in the human body?
What is the daily production of saliva in the human body?
What is the function of lysozyme in saliva?
What is the function of lysozyme in saliva?
What is the name of the process by which the pancreas secretes pancreatic juice into the duodenum?
What is the name of the process by which the pancreas secretes pancreatic juice into the duodenum?
Pair salivary glands to ducts
Pair salivary glands to ducts
Which salivary gland produces the most saliva?
Which salivary gland produces the most saliva?
Head of the pancreas sits?
Head of the pancreas sits?
Hepatic Artery Proper does ___% and Hepatic portal vein does ___% of blood supply to liver
Hepatic Artery Proper does ___% and Hepatic portal vein does ___% of blood supply to liver
Trypsinogen (inactive) activates to TRYPSIN from _______
Trypsinogen (inactive) activates to TRYPSIN from _______
Flashcards are hidden until you start studying
Study Notes
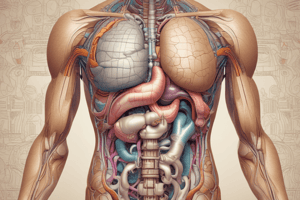
Stomach
- The stomach has four main regions: cardia, fundus, body, and pyloric part
- The stomach is divided into two main regions: anterior and posterior surfaces
- The muscularis layer of the stomach has three layers: longitudinal, circular, and oblique
- The stomach has rugae, which are folds in the mucous membrane that allow for expansion
- The stomach secrets gastric juices that contain pepsin, gastric amylase, and gastric lipase
- The stomach mixes food with gastric juices and breaks down proteins into peptides and amino acids
Functions of the Stomach
- Mechanical digestion: mixing food with gastric juices
- Chemical digestion: breaking down proteins into peptides and amino acids
- Secretion: producing gastric juices
- Mixing: churning and breaking down food
- Propulsion: moving food into the small intestine
Small Intestine
- The small intestine is responsible for most of the digestion and absorption of nutrients
- The small intestine has three main regions: duodenum, jejunum, and ileum
- The small intestine has villi, which increase the surface area for absorption
- The small intestine has microvilli, which further increase the surface area for absorption
- The small intestine secrets intestinal juice that contains enzymes to break down carbohydrates, proteins, and fats
Digestion and Absorption
- Digestion: breaking down of nutrients into smaller molecules
- Absorption: the uptake of nutrients into the bloodstream
- Chemical digestion: breaking down of nutrients into smaller molecules using enzymes
- Mechanical digestion: breaking down of food into smaller pieces using the mechanical action of the digestive system
Large Intestine
- The large intestine is responsible for the absorption of water, electrolytes, and vitamins
- The large intestine has four main regions: cecum, colon, rectum, and anus
- The large intestine has a larger diameter than the small intestine
- The large intestine has haustra, which are pouches that allow for the expansion of the intestine
- The large intestine secrets mucus to protect the intestinal wall from the acidic contents of the digestive system
Functions of the Large Intestine
- Absorption of water and electrolytes
- Absorption of vitamins
- Formation and elimination of feces
Liver and Pancreas
- The liver produces bile, which aids in the digestion of fats
- The liver regulates blood sugar levels
- The liver detoxifies the blood
- The pancreas produces pancreatic juice that contains enzymes to break down carbohydrates, proteins, and fats
- The pancreas regulates blood sugar levels
Phases of Digestion
-
Cephalic phase: preparation for food intake
-
Gastric phase: digestion in the stomach
-
Intestinal phase: digestion in the small intestine
-
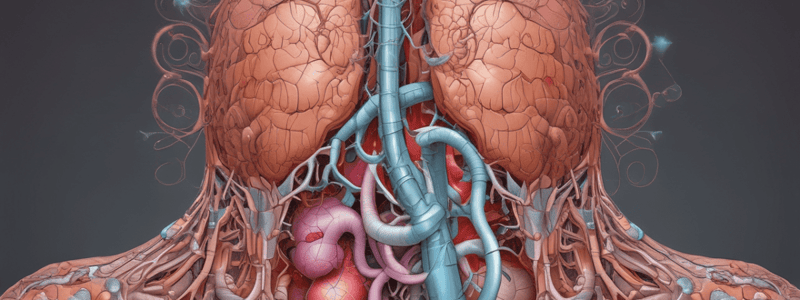
Absorptive phase: absorption of nutrients into the bloodstream### Hepatic Sinusoids
-
Highly permeable capillaries between rows of hepatocytes
-
Receive oxygenated blood from branches of the hepatic artery
-
Receive nutrient-rich, de-oxygenated blood from branches of the hepatic portal vein
Blood Supply to the Liver
- Hepatic artery: 30% of blood supply
- Hepatic portal vein: 70% of blood supply
- Central vein drains into the hepatic vein, which empties into the inferior vena cava
Portal Triad
- Consists of hepatic artery, hepatic portal vein, and bile duct
- Found in the portal triad area of the liver
Liver Function
- Filters blood coming from the digestive system
- Regulates blood sugar levels
- Removes toxins and waste products from the blood
Bile Ducts
- Right and left hepatic ducts merge to form the common hepatic duct
- Common hepatic duct merges with the cystic duct to form the common bile duct
Gallbladder
- Pear-shaped sac that stores and concentrates bile
- Located in a depression on the posterior, inferior surface of the liver
Chemical Digestion
- Mouth: lingual lipase, salivary amylase
- Stomach: gastric lipase, pepsin (from chief cells), gastrin (hormone)
- Small intestine: pancreatic amylase, lipase, proteolytic enzymes (trypsin, chymotrypsin)
Layers of the GI Tract
- Mucosa: epithelium, lamina propria, mucosa-associated lymphatic tissue (MALT)
- Submucosa: blood and lymphatic vessels
- Muscularis: circular and longitudinal layers of smooth muscle
- Serosa: outermost layer, forms the visceral peritoneum
Peritoneum
- Largest serous membrane in the body
- Parietal peritoneum lines the abdominal wall
- Visceral peritoneum lines some organs and is their serosa layer
- Peritoneal cavity: between parietal and visceral peritoneum
- Peritoneal fluid: lubricating fluid in the peritoneal cavity
Peritoneal Folds
- Greater omentum: largest fold, attaches to the greater curvature of the stomach
- Lesser omentum: attaches the liver to the stomach
- Falciform ligament: attaches the liver to the anterior abdominal wall
- Mesentery: attaches the small intestine to the posterior abdominal wall
- Mesocolon: attaches the transverse colon to the posterior abdominal wall
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.