Podcast
Questions and Answers
What is the primary function of hepatocytes?
What is the primary function of hepatocytes?
- Production of bile only
- Gas exchange in the liver
- Storage of Vitamin A only
- Protein synthesis and detoxification of toxins (correct)
Which cell type in the liver acts as a macrophage?
Which cell type in the liver acts as a macrophage?
- Gallbladder Cells
- Kupffer Cells (correct)
- Ito Cells
- Hepatocytes
What is the composition of the gallbladder's lining?
What is the composition of the gallbladder's lining?
- Stratified Squamous Epithelium
- Simple Columnar Epithelium with Microvilli (correct)
- Simple Squamous Epithelium
- Cuboidal Epithelium
Which ducts form the common bile duct?
Which ducts form the common bile duct?
What characterizes Rokitansky-Aschoff Sinuses in the gallbladder?
What characterizes Rokitansky-Aschoff Sinuses in the gallbladder?
What is the main role of pepsinogen in the stomach?
What is the main role of pepsinogen in the stomach?
Which hormone produced by the liver helps regulate metabolism by increasing insulin production?
Which hormone produced by the liver helps regulate metabolism by increasing insulin production?
Which function is NOT performed by the liver?
Which function is NOT performed by the liver?
What role do Kupffer cells serve in the liver?
What role do Kupffer cells serve in the liver?
What is the primary role of albumin produced by the liver?
What is the primary role of albumin produced by the liver?
Which of the following is a minor lobe of the liver?
Which of the following is a minor lobe of the liver?
Which cell type in the liver is involved in the detoxification of drugs and alcohol?
Which cell type in the liver is involved in the detoxification of drugs and alcohol?
What is the role of bile produced by the liver?
What is the role of bile produced by the liver?
What is the primary function of the gallbladder?
What is the primary function of the gallbladder?
Which cell type in the small intestine is responsible for secreting lysozyme?
Which cell type in the small intestine is responsible for secreting lysozyme?
What is the main role of the muscularis externa in the gastrointestinal tract?
What is the main role of the muscularis externa in the gastrointestinal tract?
Which segment of the small intestine contains Brunner’s Gland?
Which segment of the small intestine contains Brunner’s Gland?
What is the role of colonocytes in the large intestine?
What is the role of colonocytes in the large intestine?
What type of muscle fibers are organized in circular and longitudinal layers in the muscularis?
What type of muscle fibers are organized in circular and longitudinal layers in the muscularis?
What type of connective tissue makes up the submucosa?
What type of connective tissue makes up the submucosa?
Which structure is responsible for the absorption of nutrients and is characterized by plicae circulares?
Which structure is responsible for the absorption of nutrients and is characterized by plicae circulares?
Which area of the gastrointestinal tract is primarily involved in forming feces?
Which area of the gastrointestinal tract is primarily involved in forming feces?
What is the function of the serosa in the gastrointestinal tract?
What is the function of the serosa in the gastrointestinal tract?
What is the primary role of the mechanical phase of digestion?
What is the primary role of the mechanical phase of digestion?
What type of epithelium lines the esophagus?
What type of epithelium lines the esophagus?
What is the main function of the tongue's filiform papillae?
What is the main function of the tongue's filiform papillae?
Which component of the stomach secretes intrinsic factor necessary for vitamin absorption?
Which component of the stomach secretes intrinsic factor necessary for vitamin absorption?
What is the length of the human digestive tract?
What is the length of the human digestive tract?
Which type of muscle is primarily found in the upper third of the esophagus?
Which type of muscle is primarily found in the upper third of the esophagus?
What is the term for the act of swallowing?
What is the term for the act of swallowing?
What is the main function of the cardiac sphincter?
What is the main function of the cardiac sphincter?
Where are fungiform papillae predominantly located on the tongue?
Where are fungiform papillae predominantly located on the tongue?
Which substance primarily aids in the digestion of starch in the oral cavity?
Which substance primarily aids in the digestion of starch in the oral cavity?
What type of movement is segmentation, commonly observed in the intestines?
What type of movement is segmentation, commonly observed in the intestines?
Which part of the digestive system is responsible for the initial phase of digestion?
Which part of the digestive system is responsible for the initial phase of digestion?
What does chyme consist of?
What does chyme consist of?
Which of the following correctly describes the stomach's lining?
Which of the following correctly describes the stomach's lining?
Flashcards are hidden until you start studying
Study Notes
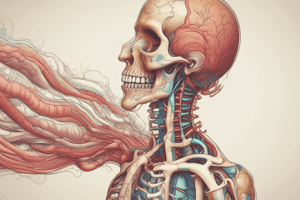
Digestive System Overview
- The digestive system is a continuous work in progress, with many organs performing specific functions for digestion.
- The digestive tract is a long, coiled tube extending from the mouth to the anus, spanning approximately nine meters in length.
- Digestion consists of two phases; Mechanical and Chemical.
- Mechanical involves breaking food into smaller pieces, pushing it down the food tube, and mixing it with digestive juices.
- Chemical involves further breaking down larger food molecules into smaller molecules through digestive enzymes.
Oral Cavity Structures
- Lips are muscular structures, predominantly formed by the Orbicularis Oris muscle.
- The oral cavity is responsible for the initial phase of digestion, which includes a small amount of absorption primarily of carbohydrates, specifically starch due to the presence of salivary amylase.
Tongue
- The tongue is a mass of striated muscle covered by mucosa.
- It's a major sensory organ for taste, and one of the essential organs for speech.
- The dorsal surface of the tongue is keratinized while the ventral surface is non-keratinized.
Tongue Papillae & Taste Receptors
- Filiform Papillae = Most numerous, cone-shaped, and the only papillae without taste buds.
- Fungiform Papillae = Mushroom or fungus shape, lightly keratinized, and located on the tip and sides of the tongue.
- Foliate Papillae = Found posterolaterally on the tongue, they have parallel ridges.
- Circumvallate Papillae = Largest, located in a V-shape at the terminal sulcus, and are the least numerous. They also have a serous minor salivary gland known as Von Ebner's gland.
Esophagus
- It's a muscular tube, approximately 25 centimeters long in adults.
- The mucosa has non-keratinized stratified squamous epithelium, and the submucosa contains small mucus-secreting glands.
- The esophageal glands are responsible for lubricating and protecting the mucosa.
- The esophagus has two sphincters: The upper and lower (cardiac) sphincters. These regulate the movement of materials into and out of the esophagus.
Stomach
- It's a J-shaped organ with a lining of simple columnar epithelium with microvilli.
- The stomach is responsible for the second phase of digestion and food storage.
- The stomach contains rugae, longitudinal folds that help with digestion.
Stomach Cells & Functions
- Surface mucous cells = "Foveolar cells", secrete alkaline mucous, and primarily line the gastric mucosa.
- Mucous neck cells = They secrete acidic mucous, which helps protect against stomach acid.
- Parietal or Oxyntic cells = Secrete gastric (hydrochloric) acid, gastroferrin (which binds to iron), and intrinsic factor (essential for vitamin B12 absorption). The parietal cells also help with digestion and activate pepsinogen.
- Chief cells = Secrete pepsinogen, an inactive form of pepsin that digests proteins.
- G-cells = "Enteroendocrine cells", secrete gastrin, which stimulates the parietal cells to produce gastric acid.
Liver
- The liver carries out several essential functions:
- Albumin synthesis, crucial for maintaining fluid within blood vessels and preventing leakage.
- Bile production, necessary for emulsification (breaking down fats) and waste removal.
- Cholesterol metabolism.
- Detoxification of drugs and alcohol.
- Excretion.
- Production of clotting factors.
- Glycogen storage.
- Hormone production: Betatrophin, Angiotensinogen, Thrombopoietin, Heparin.
Hepatocytes
- Hepatocytes are the most versatile cells in the liver, considered the functional unit of the liver.
- They perform diverse tasks: protein synthesis, detoxification of toxins, drug and alcohol metabolism, lipid synthesis, and bile production.
Liver Parts
- Lobes: The liver is composed of right and left major lobes, and the smaller caudate (tail) and quadrate lobes.
- Porta (Hilum): Contains the Hepatic Duct (right and left), the Hepatic Portal Vein, and the Hepatic Artery.
- Kupffer Cells: These are macrophages within the liver.
- Ito Cells: Also known as "HSC" or "Perisinusoidal cells", they're adipocytes located in the Space of Disse and store vitamin A.
Gallbladder
- The gallbladder is lined by simple columnar epithelium with microvilli.
- It stores and concentrates bile.
- The common bile duct is created by the joining of the cystic duct (from the gallbladder) and the hepatic duct (from the liver).
- The common bile duct empties into the duodenum.
- Rokitansky-Aschoff Sinuses: These are deep diverticula (outpouchings) found in the gallbladder mucosa.
- The gallbladder does not have a submucosa layer, unlike the stomach, small intestines, and large intestines.
- Glands of Luschka: These are developmental abnormalities, microscopic small bile ducts found in the subhepatic or subserosal connective tissue.
Pancreas
- The pancreas is a lobulated gland, divided into head, body, and tail segments.
- Ducts: The pancreas contains the Wirsung (main pancreatic duct) and the Santorini (accessory pancreatic duct).
- Exocrine Part: The exocrine part of the pancreas produces digestive enzymes, specifically proenzymes, which are inactive precursors to enzymes. The exocrine part includes pancreatic Acini and centroacinar cells.
- Sphincter of Oddi: This sphincter controls the release of bile and pancreatic juice into the duodenum.
Small Intestine
- The small intestine is the site where digestion is completed and nutrients are absorbed.
- It is made up of three segments: duodenum, jejunum, and ileum.
- The lining of the small intestine has permanent circular or semilunar folds called Plicae Circulares.
- The small intestine also contains villi.
Cells of the Small Intestine
- Enterocytes: Responsible for nutrient absorption.
- Goblet Cells: Secrete mucus to aid in lubrication and protection.
- Paneth Cells: Immune cells found at the base of intestinal crypts. They secrete lysozyme, which digests bacterial cell walls.
- Enteroendocrine Cells (APUD): Found in intestinal glands, they secrete hormones that regulate digestion.
- M (Microfold) Cells: They sample antigens from the gut lumen and carry them to immune cells.
Large Intestine
- The large intestine, also known as the "bowel," is responsible for water and electrolyte absorption.
- It forms indigestible material into feces.
- The large intestine is composed of the cecum, colon (ascending, transverse, descending), and rectum.
- Colonocytes: Columnar absorptive cells in the colon.
- Teniae Coli: Three longitudinal bands of muscle that help with peristalsis.
- Haustra: Individual segments of the colon that allow for independent contraction.
General Structure of the Digestive Tract
- The digestive tract is a hollow tube with variable lumen diameters and a wall made of four main layers:
- Mucosa
- Submucosa
- Muscularis
- Serosa
Mucosa
- The mucosa consists of:
- An epithelial lining.
- An underlying lamina propria composed of loose connective tissue.
- A thin layer of smooth muscle known as the Muscularis Mucosae.
Submucosa
- The submucosa contains dense connective tissue, larger blood and lymph vessels, and the submucosal plexus (Meissner's Plexus) of the autonomic nervous system (ANS).
- The submucosa also includes Brunner's glands, which are only found in the duodenum.
Muscularis (Muscularis Externa)
- The muscularis is composed of smooth muscle cells arranged in two or more sublayers:
- Internal Sublayer (Circular): Closer to the lumen, the fibers are generally circular.
- External Sublayer (Longitudinal): The fibers run longitudinally.
- The muscularis contains the Myenteric Plexus (Auerbach's Plexus) of the ANS, which controls contractions for peristalsis.
Serosa
- The serosa is a thin layer of loose connective tissue rich in blood vessels, lymphatics, and adipose tissue. It is covered by mesothelium, a simple squamous epithelium.
- In the abdominal cavity, the serosa is continuous with mesenteries, which are covered by mesothelium on both sides and support the intestines.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.