Podcast
Questions and Answers
Where does most nutrient digestion occur in the small intestine?
Where does most nutrient digestion occur in the small intestine?
- In the cytoplasm of enterocytes
- In the duodenum
- In the lumen of the small intestine
- In the brush border (correct)
What is the primary function of secretin in the small intestine?
What is the primary function of secretin in the small intestine?
- Promotes bile storage
- Stimulates gastric secretion
- Inhibits gastric secretions and stimulates pancreas secretions (correct)
- Inhibits pancreatic secretion
What role does alkaline and viscous mucus serve in the duodenum?
What role does alkaline and viscous mucus serve in the duodenum?
- Stimulates bile production
- Protects mucosa and neutralizes acidic chyme (correct)
- Aids in substrate digestion
- Enhances enzyme secretion
What percentage of ingested carbohydrates is digested by pancreatic enzymes?
What percentage of ingested carbohydrates is digested by pancreatic enzymes?
Which hormone is released by D-cells in the duodenum and pancreas?
Which hormone is released by D-cells in the duodenum and pancreas?
What is bile predominantly composed of?
What is bile predominantly composed of?
What is NOT a function of the gallbladder?
What is NOT a function of the gallbladder?
Which of the following is true regarding pancreatic enzymes?
Which of the following is true regarding pancreatic enzymes?
What mechanism allows fructose to be transported from the mucosal cell into the bloodstream?
What mechanism allows fructose to be transported from the mucosal cell into the bloodstream?
What happens to fructose once it reaches the liver?
What happens to fructose once it reaches the liver?
What is a common public health issue associated with increased fructose intake?
What is a common public health issue associated with increased fructose intake?
How can the absorption of fructose be improved in individuals with sensitivity?
How can the absorption of fructose be improved in individuals with sensitivity?
What transport system is associated with the absorption of fructose combined with glucose?
What transport system is associated with the absorption of fructose combined with glucose?
Which of the following tissues relies heavily on a continuous supply of glucose?
Which of the following tissues relies heavily on a continuous supply of glucose?
What is the major site of gluconeogenesis in the body?
What is the major site of gluconeogenesis in the body?
Which of the following is NOT a source of glucose production during gluconeogenesis?
Which of the following is NOT a source of glucose production during gluconeogenesis?
Which enzyme is specifically involved in the bypass of the pyruvate kinase step during gluconeogenesis?
Which enzyme is specifically involved in the bypass of the pyruvate kinase step during gluconeogenesis?
Which compound is an intermediate product of the gluconeogenesis pathway?
Which compound is an intermediate product of the gluconeogenesis pathway?
What happens to galactose in hepatocytes?
What happens to galactose in hepatocytes?
In which tissues is glucose distributed after being metabolized in the liver?
In which tissues is glucose distributed after being metabolized in the liver?
Which glucose transporter is primarily involved in insulin-dependent uptake?
Which glucose transporter is primarily involved in insulin-dependent uptake?
What mechanism facilitates fructose transport in the intestinal lumen?
What mechanism facilitates fructose transport in the intestinal lumen?
What is the primary function of phosphorylating galactose in the liver?
What is the primary function of phosphorylating galactose in the liver?
How does glucose metabolism differ from galactose in terms of distribution?
How does glucose metabolism differ from galactose in terms of distribution?
What does the absorption of fructose in the intestinal lumen primarily rely on?
What does the absorption of fructose in the intestinal lumen primarily rely on?
What happens to glucose after it is absorbed in the intestine?
What happens to glucose after it is absorbed in the intestine?
What is one effect of soluble fiber on diabetes mellitus?
What is one effect of soluble fiber on diabetes mellitus?
Which of the following statements is true regarding the benefits of fiber in relation to heart disease?
Which of the following statements is true regarding the benefits of fiber in relation to heart disease?
What role does soluble fiber play in obesity management?
What role does soluble fiber play in obesity management?
Which of the following gastrointestinal disorders may benefit from the prebiotic effects of fiber?
Which of the following gastrointestinal disorders may benefit from the prebiotic effects of fiber?
How do beneficial bacterial species contribute to the prevention of colon cancer?
How do beneficial bacterial species contribute to the prevention of colon cancer?
Flashcards are hidden until you start studying
Study Notes
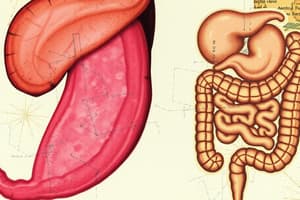
Small Intestine
- Digestion of nutrients usually is completed in the brush border.
- Some nutrient digestion is completed in the cytoplasm of the enterocyte.
- Mixing and propelling occur in the small intestine.
Small Intestine - Secretory Products
- Duodenum secretes alkaline and viscous mucus to protect the mucosa from damage and neutralize highly acidic chyme.
- Secretin: inhibits gastric secretions, stimulates pancreas and gallbladder secretions.
- Somatostatin: released by D-cells in the duodenum, pancreas, and antrum of the stomach, diminishes secretion by stomach cells
Pancreas
- Pancreatic enzymes digest 50% of all ingested carbohydrates, 50% of all proteins and 80-90% of ingested fat.
- Two active cells are stimulated by secretin:
- Acinar cells: produce enzymatic secretions
- Duct cells: produce bicarbonate
Liver/Gallbladder
- The liver produces bile, which is stored and concentrated in the gallbladder.
- Bile: greenish-yellow fluid; mostly contains bile acids and salts to emulsify lipids; also contains cholesterol, phospholipids, and bile pigments
Galactose Absorption
- Galactose is phosphorylated in the hepatocytes, which traps it in the liver.
- Galactose can be converted into glucose derivatives, enters glucose metabolism and is stored as liver glycogen.
Glucose Absorption
- Glucose is extensively metabolized in the liver.
- Glucose is not as withheld from further distribution as galactose and fructose.
- Portions of glucose go through the bloodstream to be distributed to:
- Muscle
- Kidney
- Adipose tissue (Insulin-dependent uptake via GLUT4)
Fructose Absorption
- Fructose enters the mucosal cell via GLUT 5.
- Fructose leaves the mucosal cell and is quickly transported via the portal vein into the liver.
- Fructose is phosphorylated in the liver = 'trapped' in the hepatocytes.
- Fructose concentrations are 'kept low'.
Fructose - Public Health Issues
- Not everyone can absorb fructose efficiently.
- Approximately 60% of healthy adults show intestinal distress after consuming 50 grams of pure fructose.
Fructose Absorption
- More fructose can be absorbed with high glucose intake.
- The disaccharidase-related transport system can help with fructose absorption.
- Less intestinal discomfort when fructose and glucose are consumed together or fructose is part of a mixed diet.
- Balancing dietary fructose and glucose can mitigate clinical symptoms in individuals with apparent fructose sensitivity.
Glucose Transporters
- Glucose enters cells via transporters.
- Tissues that are particularly dependent on glucose supply:
- Brain
- Central nervous system
- Erythrocytes
Gluconeogenesis
- Gluconeogenesis is the production of glucose from non-carbohydrate sources.
- Sources include:
- Pyruvate
- Lactate
- Glycerol
- Amino acids
- The major site of gluconeogenesis is the liver.
Gluconeogenesis - Bypass of Pyruvate Kinase Step
- Gluconeogenesis bypasses the pyruvate kinase step of glycolysis.
- Two enzymes catalyze the bypass:
- Pyruvate carboxylase
- Phosphoenolpyruvate carboxykinase
Fiber - Soluble vs Insoluble
- Soluble fiber dissolves in water and forms a gel-like substance.
- Insoluble fiber doesn't dissolve in water.
Fiber - Disease Prevention and Management
- Diabetes mellitus: hypoglycemic effects; food matrix issue; whole wheat cereal vs. cereal fiber
- Heart disease: hypolipidemic and hypocholesterolemic effects
- Obesity: increased satiety; reduced absorption of macronutrients
- Gastrointestinal disorders: prebiotic effects; support growth of beneficial bacteria
- Colon cancer: beneficial bacteria protective against cancer; likely through formation of SCFA
Pectins
- Pectins are soluble fiber.
- Properties of pectins:
- Viscous
- Gel-forming
- Physiological effects:
- Slow down gastric emptying
- Reduced glucose absorption
- Lower cholesterol
- Pectins contribute to the prevention of cardiovascular disease.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.