Podcast
Questions and Answers
Which diagnostic test is NOT commonly used for colorectal cancer?
Which diagnostic test is NOT commonly used for colorectal cancer?
- Tumor biopsy
- Colonoscopy
- Digital rectal exam
- Hepatitis profile (correct)
What is a common sign or symptom of hepatitis?
What is a common sign or symptom of hepatitis?
- Persistent cough
- Chest pain
- Enlarged tender liver (correct)
- Severe headache
What is a common cause of Viral Hepatitis A & E transmission?
What is a common cause of Viral Hepatitis A & E transmission?
- Sharing needles
- Sexual contact
- Contaminated blood transfusions
- Contaminated food and water (correct)
Which treatment is NOT typically used for Viral Hepatitis B?
Which treatment is NOT typically used for Viral Hepatitis B?
Which complication can occur as a result of chronic Viral Hepatitis B infection?
Which complication can occur as a result of chronic Viral Hepatitis B infection?
What is a common cause of appendicitis?
What is a common cause of appendicitis?
What is a symptom of colorectal cancer?
What is a symptom of colorectal cancer?
Which treatment is commonly utilized for appendicitis?
Which treatment is commonly utilized for appendicitis?
What diagnostic test is commonly used to confirm appendicitis?
What diagnostic test is commonly used to confirm appendicitis?
What complication can arise from untreated appendicitis?
What complication can arise from untreated appendicitis?
What is a significant risk associated with chronic hepatitis?
What is a significant risk associated with chronic hepatitis?
Which of the following best describes the pathophysiology of liver cirrhosis?
Which of the following best describes the pathophysiology of liver cirrhosis?
What demographic is most commonly affected by gallstones?
What demographic is most commonly affected by gallstones?
What is the most common treatment for symptomatic gallstones?
What is the most common treatment for symptomatic gallstones?
Which factor is NOT typically associated with the formation of gallstones?
Which factor is NOT typically associated with the formation of gallstones?
What is the primary function of the stomach in the digestive process?
What is the primary function of the stomach in the digestive process?
Which organ is primarily responsible for the absorption of nutrients?
Which organ is primarily responsible for the absorption of nutrients?
What is the length of the large intestine?
What is the length of the large intestine?
What role does the liver play in the digestive system?
What role does the liver play in the digestive system?
Which accessory organ of digestion is primarily involved in fat digestion?
Which accessory organ of digestion is primarily involved in fat digestion?
Which of the following statements about the small intestine is true?
Which of the following statements about the small intestine is true?
What is the main function of the gall bladder?
What is the main function of the gall bladder?
What is the process called that moves food through the esophagus?
What is the process called that moves food through the esophagus?
What is the primary cause of acute pancreatitis in the majority of cases?
What is the primary cause of acute pancreatitis in the majority of cases?
Which of the following is a common sign of acute pancreatitis?
Which of the following is a common sign of acute pancreatitis?
Which underlying condition is NOT typically associated with acute pancreatitis?
Which underlying condition is NOT typically associated with acute pancreatitis?
What is the recommended initial treatment for a patient with acute pancreatitis?
What is the recommended initial treatment for a patient with acute pancreatitis?
Which of these factors is NOT recognized as a possible aetiology of acute pancreatitis?
Which of these factors is NOT recognized as a possible aetiology of acute pancreatitis?
What contributes to the vascular damage seen in acute pancreatitis?
What contributes to the vascular damage seen in acute pancreatitis?
What is the mortality rate commonly associated with acute pancreatitis?
What is the mortality rate commonly associated with acute pancreatitis?
Which symptom is typically found on an abdominal X-ray in cases of acute pancreatitis?
Which symptom is typically found on an abdominal X-ray in cases of acute pancreatitis?
What is the primary role of the pancreas in digestion?
What is the primary role of the pancreas in digestion?
Which of the following is NOT a common cause of gastritis?
Which of the following is NOT a common cause of gastritis?
What is a potential complication of untreated gastritis?
What is a potential complication of untreated gastritis?
What symptom is commonly associated with peptic ulcer disease?
What symptom is commonly associated with peptic ulcer disease?
Which of the following treatments is typically recommended for gastritis?
Which of the following treatments is typically recommended for gastritis?
What could lead to a deficiency in vitamin B12 in patients with chronic gastritis?
What could lead to a deficiency in vitamin B12 in patients with chronic gastritis?
Which diagnostic test is used specifically to identify H. pylori infection in peptic ulcer disease?
Which diagnostic test is used specifically to identify H. pylori infection in peptic ulcer disease?
Which of the following is a recognized risk factor for developing peptic ulcer disease?
Which of the following is a recognized risk factor for developing peptic ulcer disease?
Flashcards
Incubation time for Hepatitis C
Incubation time for Hepatitis C
The period between exposure to Hepatitis C virus and the development of symptoms is typically 5 to 9 weeks.
Chronic Hepatitis
Chronic Hepatitis
A long-term inflammation of the liver caused by a persistent infection, often leading to liver damage.
Liver Cirrhosis
Liver Cirrhosis
A chronic, irreversible liver disease characterized by the replacement of healthy liver tissue with scar tissue and fibrosis.
Causes of Liver Cirrhosis
Causes of Liver Cirrhosis
Signup and view all the flashcards
Gallstones
Gallstones
Signup and view all the flashcards
H. pylori
H. pylori
Signup and view all the flashcards
Appendicitis
Appendicitis
Signup and view all the flashcards
McBurney's Point
McBurney's Point
Signup and view all the flashcards
Colorectal Cancer
Colorectal Cancer
Signup and view all the flashcards
Occult Blood
Occult Blood
Signup and view all the flashcards
Hepatitis
Hepatitis
Signup and view all the flashcards
Viral Hepatitis A & E
Viral Hepatitis A & E
Signup and view all the flashcards
Viral Hepatitis B
Viral Hepatitis B
Signup and view all the flashcards
Viral Hepatitis C
Viral Hepatitis C
Signup and view all the flashcards
What is the role of the stomach in digestion?
What is the role of the stomach in digestion?
Signup and view all the flashcards
What is the function of the small intestine?
What is the function of the small intestine?
Signup and view all the flashcards
What are the main functions of the large intestine?
What are the main functions of the large intestine?
Signup and view all the flashcards
What is the key role of bile produced by the liver?
What is the key role of bile produced by the liver?
Signup and view all the flashcards
What does the gallbladder do?
What does the gallbladder do?
Signup and view all the flashcards
What are some core functions of the liver?
What are some core functions of the liver?
Signup and view all the flashcards
What is Peristalsis?
What is Peristalsis?
Signup and view all the flashcards
What are gastric glands?
What are gastric glands?
Signup and view all the flashcards
Pancreas
Pancreas
Signup and view all the flashcards
Gastritis
Gastritis
Signup and view all the flashcards
Causes of Gastritis
Causes of Gastritis
Signup and view all the flashcards
Symptoms of Gastritis
Symptoms of Gastritis
Signup and view all the flashcards
Peptic Ulcer Disease
Peptic Ulcer Disease
Signup and view all the flashcards
Causes of Peptic Ulcer Disease
Causes of Peptic Ulcer Disease
Signup and view all the flashcards
Symptoms of Peptic Ulcer Disease
Symptoms of Peptic Ulcer Disease
Signup and view all the flashcards
Diagnostic Tests for Peptic Ulcer Disease
Diagnostic Tests for Peptic Ulcer Disease
Signup and view all the flashcards
What is acute pancreatitis?
What is acute pancreatitis?
Signup and view all the flashcards
What are the main causes of acute pancreatitis?
What are the main causes of acute pancreatitis?
Signup and view all the flashcards
What are other potential causes of acute pancreatitis?
What are other potential causes of acute pancreatitis?
Signup and view all the flashcards
What happens in the pancreas during acute pancreatitis?
What happens in the pancreas during acute pancreatitis?
Signup and view all the flashcards
What are the signs and symptoms of acute pancreatitis?
What are the signs and symptoms of acute pancreatitis?
Signup and view all the flashcards
How is acute pancreatitis treated?
How is acute pancreatitis treated?
Signup and view all the flashcards
What is the mortality rate for acute pancreatitis?
What is the mortality rate for acute pancreatitis?
Signup and view all the flashcards
What is the significance of high serum amylase and lipase in acute pancreatitis?
What is the significance of high serum amylase and lipase in acute pancreatitis?
Signup and view all the flashcards
Study Notes
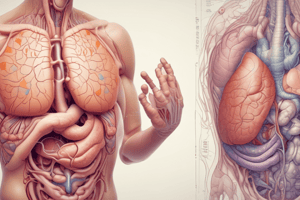
Gastrointestinal System and Accessory Organs
- The presentation covers disorders of the gastrointestinal system and its accessory organs.
- The material includes the anatomy of the digestive system, focusing on the reflected small intestine, and normal anatomy of various parts, including the mouth, pharynx, esophagus, stomach, small intestine, appendix, large intestine, gallbladder, liver, and pancreas.
- It details the oral cavity, including hard and soft palates, tongue, and salivary glands.
- It discusses swallowing (buccal, pharyngeal, esophageal phases) and peristalsis (movement of food through the digestive tract)
- The stomach's function is described as a stretchy bag that holds ingested food, mixing it with gastric juices to break it down.
- The slides detail the structure and functions of various parts of the stomach including layers (serosa, muscularis, submucosa, mucosa).
- The presentation discusses the small intestine, mentioning its length (6 meters), role in digesting and absorbing nutrients with pancreatic enzymes, and the duration food remains there (24-48 hours).
- The large intestine absorbs water and receives waste from the small intestine.
- The accessory organs include the liver, gallbladder, and pancreas. The liver's function is as a factory for antibodies and bile, detoxification device and stores vitamins.
- Gallbladder is shaped like a pear, situated under the liver, and secretes bile to aid fat breakdown.
- The pancreas produces enzymes that aid digestion.
- The content discusses disorders like gastritis, its causes (irritants, bacteria/viral infections, peptic ulcers, bile acid reflux), symptoms (abdominal pain, nausea, vomiting), diagnostic tests (CBC, stool test, endoscopy) and treatments.
- The presentation also covers peptic ulcer disease (including duodenum, gastric mucosa, causes like H.pylori infection, family history, smoking, stress, NSAIDs), symptoms, diagnosis, and treatment options.
- Appendicitis is described as a bacterial infection of the appendix, which requires prompt surgery, often due to trapped feces. It lists symptoms (fever, abdominal pain, anorexia, nausea, vomiting).
- Diagnostic tests and treatments for appendicitis are explained as well: temperature, Mc Burney’s sign, blood test. Ultrasound, and surgery (appendectomy).
- Different types of hepatitis are listed according to causes (toxic liver disease, alcohol, viral ie hepatitis A,B,C,D & E), discussing features like incubation times, symptoms (and related diagnostics), treatment approaches.
- Liver cirrhosis discussed, mentioning causes (alcoholism, bile duct disease, chronic hepatitis). Symptoms and diagnosis.
- The presentation contains information on gallstones and their impact on the bile duct, which is a common cause of hospitalization, and includes discussions on other related conditions like cholecystitis.
- It discusses acute pancreatitis outlining the causes (obstruction of main pancreatic duct and chronic alcohol ingestion),signs, symptoms and treatment: NPO, IV fluids, analgesics, treat underlying cause.
- Lastly slide 68 lists overview of major components of the digestive system with their functions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.