Podcast
Questions and Answers
What is diffuse parenchymal lung disease?
What is diffuse parenchymal lung disease?
- A group of conditions affecting the pulmonary parenchyma and/or alveolar lumen (correct)
- A type of heart disease
- A specific type of lung disease
- A type of lung infection
What is a typical symptom of diffuse parenchymal lung disease?
What is a typical symptom of diffuse parenchymal lung disease?
- Coughing up blood
- Dry, persistent and distressing cough (correct)
- Sudden loss of breath
- Pain in the chest
What is a common finding on examination in diffuse parenchymal lung disease?
What is a common finding on examination in diffuse parenchymal lung disease?
- Abnormal heart sounds
- Wheezing
- Sroscope sounds
- Crackles (correct)
What is a radiological feature of advanced diffuse parenchymal lung disease?
What is a radiological feature of advanced diffuse parenchymal lung disease?
What is a typical finding on pulmonary function testing in diffuse parenchymal lung disease?
What is a typical finding on pulmonary function testing in diffuse parenchymal lung disease?
What is a condition that can mimic diffuse parenchymal lung disease?
What is a condition that can mimic diffuse parenchymal lung disease?
What is a type of diffuse parenchymal lung disease?
What is a type of diffuse parenchymal lung disease?
What is a complication of advanced diffuse parenchymal lung disease?
What is a complication of advanced diffuse parenchymal lung disease?
What is the most common laboratory investigation for sarcoidosis?
What is the most common laboratory investigation for sarcoidosis?
Which of the following is NOT a cause of diffuse parenchymal lung disease?
Which of the following is NOT a cause of diffuse parenchymal lung disease?
What is the primary purpose of bronchoalveolar lavage?
What is the primary purpose of bronchoalveolar lavage?
What is the definition of idiopathic pulmonary fibrosis?
What is the definition of idiopathic pulmonary fibrosis?
What can be found in occupational fibrosing lung disease through a biopsy?
What can be found in occupational fibrosing lung disease through a biopsy?
What is the purpose of a liver biopsy in sarcoidosis?
What is the purpose of a liver biopsy in sarcoidosis?
What is the association of elevated Ca2+ levels?
What is the association of elevated Ca2+ levels?
Which of the following is a connective tissue disease associated with diffuse parenchymal lung disease?
Which of the following is a connective tissue disease associated with diffuse parenchymal lung disease?
When is bronchoscopy usually indicated?
When is bronchoscopy usually indicated?
What is the primary concern in cases where lung biopsy is being considered?
What is the primary concern in cases where lung biopsy is being considered?
What is the primary goal of pirfenidone and nintedanib treatments?
What is the primary goal of pirfenidone and nintedanib treatments?
What is the definition of pneumoconiosis?
What is the definition of pneumoconiosis?
What is the most important type of pneumoconiosis?
What is the most important type of pneumoconiosis?
What is the result of prolonged inhalation of coal dust?
What is the result of prolonged inhalation of coal dust?
What is the classification of coal worker’s pneumoconiosis based on?
What is the classification of coal worker’s pneumoconiosis based on?
What is simple coal worker’s pneumoconiosis (SCWP) characterized by?
What is simple coal worker’s pneumoconiosis (SCWP) characterized by?
What is an important step in excluding fibrosing diseases caused by occupational exposure, medication, or connective tissue diseases?
What is an important step in excluding fibrosing diseases caused by occupational exposure, medication, or connective tissue diseases?
What is the typical age of onset for IPF?
What is the typical age of onset for IPF?
What is a common symptom of IPF?
What is a common symptom of IPF?
What is a characteristic clinical finding in IPF?
What is a characteristic clinical finding in IPF?
What is the typical pattern of reticular shadowing on chest X-ray in IPF?
What is the typical pattern of reticular shadowing on chest X-ray in IPF?
What is the high positive predictive value of HRCT for the diagnosis of IPF based on?
What is the high positive predictive value of HRCT for the diagnosis of IPF based on?
What is a characteristic feature of advanced IPF on HRCT?
What is a characteristic feature of advanced IPF on HRCT?
What is the significance of pleural plaques on HRCT?
What is the significance of pleural plaques on HRCT?
What is the characteristic of conglomerate masses in Progressive Massive Fibrosis (PMF)?
What is the characteristic of conglomerate masses in Progressive Massive Fibrosis (PMF)?
What is the common symptom associated with the development of PMF?
What is the common symptom associated with the development of PMF?
What is the treatment goal for PMF?
What is the treatment goal for PMF?
What is the condition characterized by the coexistence of rheumatoid arthritis and rounded fibrotic nodules?
What is the condition characterized by the coexistence of rheumatoid arthritis and rounded fibrotic nodules?
What is the usual form of silica inhaled by workers that leads to silicosis?
What is the usual form of silica inhaled by workers that leads to silicosis?
What is the typical duration of silica exposure associated with classic or sub-acute silicosis?
What is the typical duration of silica exposure associated with classic or sub-acute silicosis?
What is the increased risk associated with silicosis?
What is the increased risk associated with silicosis?
What is the primary goal of treatment for silicosis?
What is the primary goal of treatment for silicosis?
Flashcards are hidden until you start studying
Study Notes
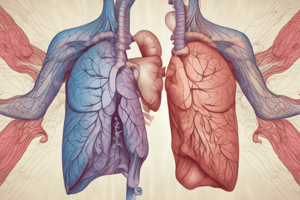
Diffuse Parenchymal Lung Disease
- Heterogeneous group of conditions affecting the pulmonary parenchyma (interstitium) and/or alveolar lumen
- Shares clinical, physiological, and radiographic similarities
Clinical Presentation
- Cough: usually dry, persistent, and distressing
- Breathlessness: usually slowly progressive, insidious onset, acute in some cases
- Examination findings:
- Crackles: typically bilateral and basal
- Clubbing: common in idiopathic pulmonary fibrosis, also seen in other types (e.g., asbestosis)
- Central cyanosis and signs of right heart failure in advanced disease (corpulmonale)
Radiology
- Chest X-ray: typically small lung volumes with reticulonodular shadowing, but may be normal in early or limited disease
- High-resolution computed tomography: combinations of ground glass changes, reticulonodular shadowing, honeycomb cysts, and traction bronchiectasis, depending on stage of disease
PFT
- Typically restrictive ventilatory defect with reduced lung volumes and impaired gas transfer
- Exercise tests assess exercise tolerance and exercise-related fall in SaO2
Acute Interstitial Pneumonia
- Organizing pneumonia
- Bronchopneumonia
- Pulmonary oedema
Conditions that Mimic Diffuse Parenchymal Lung Disease
- Infection:
- Viral pneumonia
- Tuberculosis
- Pneumocystis jirovecii
- Parasite (e.g., lariasis)
- Fungal infection
- Malignancy:
- Leukemia and lymphoma
- Multiple metastases
- Lymphangitic carcinomatosis
- Bronchoalveolar carcinoma
- Pulmonary oedema
- Aspiration pneumonia
Laboratory Investigations
- Full blood count: lymphopenia in sarcoidosis, eosinophilia in pulmonary eosinophilias and drug reactions, neutrophilia in hypersensitivity pneumonitis
- Erythrocyte sedimentation rate and C-reactive protein: non-specifically raised
- Ca2+: may be elevated in sarcoidosis
- Serum angiotensin-converting enzyme: non-specific indicator of disease activity in sarcoidosis
- Lactate dehydrogenase: may be elevated in active alveolitis
- Autoimmune screen: anti-cyclic citrullinated peptide (anti-CCP) and other autoantibodies may suggest connective tissue disease
Radiology and PFT
- Chest X-ray and high-resolution computed tomography
- PFT: typically restrictive ventilatory defect with reduced lung volumes and impaired gas transfer
Bronchoscopy and Biopsy
- Bronchoscope: differential cell counts may point to sarcoidosis, drug-induced pneumonitis, pulmonary eosinophilias, hypersensitivity pneumonitis, or cryptogenic organizing pneumonia
- Transbronchial biopsy: useful in sarcoidosis and differential of malignancy or infection
- Video-assisted thoracoscopic lung biopsy (VATS): allows pathological classification, presence of asbestos bodies may suggest asbestosis, silica in occupational fibrosing lung disease
Idiopathic Pulmonary Fibrosis
- Defined as a progressive fibrosing interstitial pneumonia of unknown cause, occurring in adults and associated with the histological or radiological pattern of UIP
- Important differentials include fibrosing diseases caused by occupational exposure, medication, or connective tissue diseases
- Histological features suggest repeated episodes of focal damage to the alveolar epithelium
- Familial cases are rare, but genetic factors that control the inflammatory and fibrotic response are likely to be important
- Strong association with cigarette smoking
Clinical Features of IPF
- Presents in older adults, uncommon before the age of 50 years
- May present as an incidental finding on CT scan or with progressive breathlessness and a non-productive cough
- Constitutional symptoms are unusual
- Clinical findings include finger clubbing and bi-basal fine late inspiratory crackles
Investigations for IPF
- Full blood count, erythrocyte sedimentation rate, and C-reactive protein
- Chest X-ray and high-resolution computed tomography
- Bronchoscope: lymphocytosis may suggest chronic hypersensitivity pneumonitis
- Surgical lung biopsy: should be sought if necessary
Treatment of IPF
- Pirfenidone (an antifibrotic agent) or nintedanib (a tyrosine kinase inhibitor) may be offered
- Both agents have been shown to reduce the rate of decline in lung function
- Neither drug improves cough or breathlessness, and treatment should be discontinued if lung function declines by more than 10% over the first year of treatment
- Medication to control gastro-oesophageal reflux may improve the cough
- Stop smoking, oxygen therapy, and lung transplantation may be considered
Prognosis of IPF
- Median survival of 3 years is widely quoted
- Rate of disease progression varies considerably
Pneumoconiosis
- Permanent alteration of lung structure due to the inhalation of mineral dust and the tissue reactions of the lung to its presence
- Important pneumoconiosis include coal worker's pneumoconiosis, silicosis, and asbestosis
Coal Worker's Pneumoconiosis (CWP)
- Follows prolonged inhalation of coal dust, resulting in a fibrotic reaction and the appearance of scattered discrete fibrotic lesions
- Classification is based on the size and extent of radiographic nodularity
- Simple coal worker's pneumoconiosis (SCWP) refers to the appearance of small radiographic nodules in an otherwise asymptomatic individual
- Progressive massive fibrosis (PMF) refers to the formation of one or more conglomerate masses more than 1 cm in diameter
- Treatment involves removing or reducing coal dust exposure, and is otherwise supportive treatment
- PMF may progress, even after coal dust exposure ceases, and in extreme cases leads to respiratory failure and right ventricular failure
- CWP is not associated with increased risk of lung cancer
- Caplan syndrome describes the coexistence of rheumatoid arthritis and rounded fibrotic nodules 0.5-5 cm in diameter
Silicosis
- Results from the inhalation of crystalline silica, usually in the form of quartz, by workers cutting, grinding, and polishing stone
- Patients experience dry cough and breathlessness with the sensation of chest restriction
- Classic or sub-acute silicosis is most common and usually manifests after 10-20 years of continuous silica exposure
- Accelerated silicosis is associated with a much shorter duration of dust exposure (typically 5-10 years), may present as early as after 1 year of exposure, and follows a more aggressive course
- Intense exposure to very fine crystalline silica dust can cause a more acute disease: silicoproteinosis
- Chronic silicosis can develop after 10-30 years of continuous exposure to lower concentrations of silica dust
- Treatment, aside from stopping exposure, is mainly supportive
- Increased risk of TB (silicotuberculosis), non-tuberculous mycobacterial infection, lung cancer, and COPD
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.